Last Updated on November 13, 2025 by
Thrombocytopenia in children means they have too few platelets. This can cause bruising, bleeding, and other problems. Immune thrombocytopenic purpura (ITP) is the most common type of this condition. What is the most common thrombocytopenia in children? Learn about trombopenie (thrombocytopenia) and get amazing, powerful facts on its prevalence in kids.
At Liv Hospital, we understand how important it is to know about ITP. We know it can be a temporary issue, but its severity and how long it lasts can change. This depends on the child’s age and other factors.
We are committed to giving children with ITP the best care. We follow international standards to ensure they get the best treatment.
Understanding thrombocytopenia in kids is key to their health. It’s when platelet counts drop below 150,000/microL. This condition affects children in many ways.
Thrombocytopenia means having too few platelets in the blood. Platelet counts in kids should be between 150,000 to 450,000/microL. Counts under 150,000/microL are considered low.
Pediatric thrombocytopenia is divided by cause, duration, and severity. It can be acute or chronic, lasting over 12 months. Causes include immune issues and bone marrow problems.
Knowing the type helps doctors choose the right treatment. A detailed diagnosis is essential.
Low platelets can harm a child’s health. It raises the risk of bleeding and bruising. Kids might get easy bruises, nosebleeds, or small spots on their skin.
Severe cases can lead to serious bleeding. This shows why quick diagnosis and treatment are vital.
ITP is the top reason for low platelet counts in kids. It’s a condition where the immune system attacks and destroys platelets. We’ll dive into what causes ITP in children, including its effects and how it happens.
Knowing how common ITP is helps us understand it better. It affects about 4“6 kids per 100,000 each year. This shows ITP is rare but important in kids.
What causes ITP isn’t fully known. But it’s thought to be linked to genes and things like viruses. Studying ITP helps us find better ways to treat it.
ITP can happen to any child, but it’s more common in some ages. It often starts in kids as young as a few months. The highest number of cases is between 2 and 5 years old.
Some studies say more boys get ITP, while others find it’s about the same for both boys and girls. Knowing this helps doctors and parents be more aware.
ITP happens when the immune system attacks platelets. Autoantibodies mark these platelets for destruction, mainly in the spleen. This shortens their life and leads to low platelet counts.
Understanding how ITP works is key to treating it. Research has led to new ways to stop platelet destruction and help them grow back.
It’s important to know how pediatric ITP presents itself early on. This helps in managing it better. Kids with ITP show different symptoms, ranging from mild to severe.
Children with ITP often bruise easily or have small spots on their skin called petechiae. Petechiae are often seen on the legs, arms, and torso. They might also have nosebleeds or bleeding gums.
In some cases, the bleeding can be more serious. This includes bleeding in the stomach or urinary tract.
The symptoms can vary a lot among kids. Some might just have a few bruises. Others might bleed more often and severely.
ITP is divided into mild, moderate, or severe based on bleeding symptoms. This helps doctors decide on treatment and risk of complications. Severity is often categorized as mild, moderate, or severe, based on bleeding frequency and intensity.
One of the most serious complications is intracranial hemorrhage (ICH), or bleeding in the brain. It’s a medical emergency. Other rare complications include serious stomach bleeding or internal hemorrhages.
It’s key to recognize ITP symptoms and understand their severity. This helps manage the condition well and avoid serious problems.
Exploring the causes and triggers of childhood ITP shows a mix of factors. Knowing these causes is key to managing and treating the condition well.
Post-viral infections are a main trigger for childhood ITP. Viruses like measles, mumps, and rubella can lead to ITP. After these infections, the immune system might attack platelets by mistake.
The exact reason is not clear. But, it’s thought that antibodies against viruses can also attack platelets. This leads to their destruction.
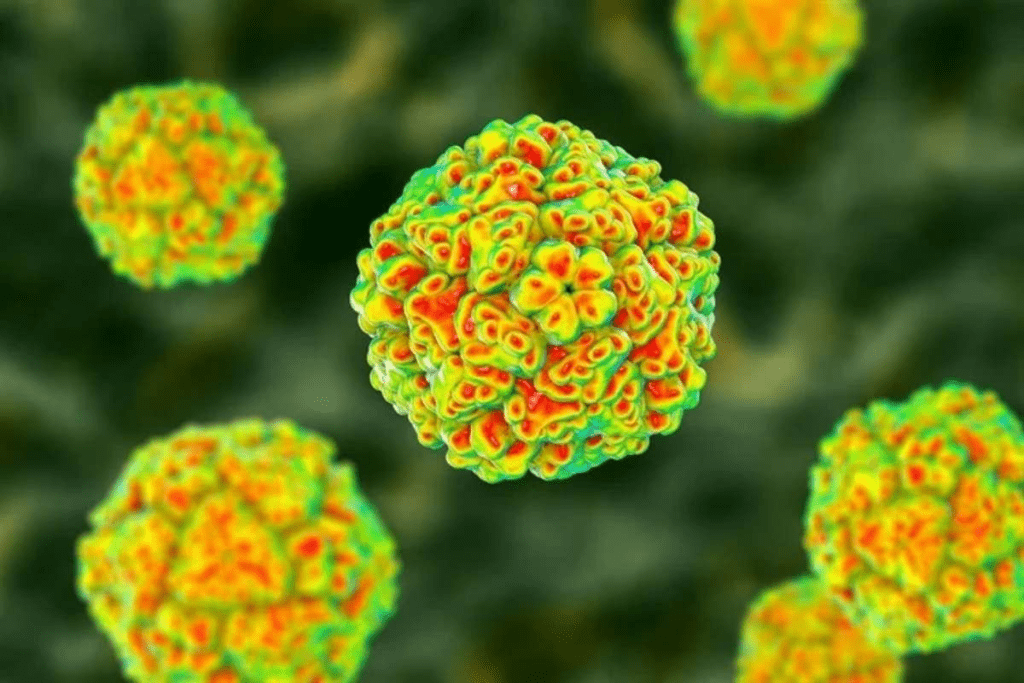
Post-vaccination is another big trigger. Routine immunizations can cause ITP in kids. It’s important for parents and doctors to know about this risk.
The way vaccines cause ITP is similar to post-viral ITP. It’s about an immune reaction to vaccine antigens that also attacks platelets.
Other things can also start ITP in kids. These include genetic predispositions and environmental factors. Sometimes, ITP is linked to other health issues.
Finding these triggers is vital. It helps create a treatment plan that tackles the symptoms and the root causes of ITP.
Getting a correct diagnosis of ITP in kids is key. It means checking for other reasons of low platelet count. “The diagnosis of ITP is often one of exclusion, requiring a thorough check to rule out other possible causes of low platelet count,” say pediatric hematologists.
The first step in diagnosing ITP is to do lab tests. These tests check the platelet count and look for other blood problems. A complete blood count (CBC) is usually the first test. It often shows just low platelets.
More tests might include:
It’s important to figure out if it’s ITP or something else. Many conditions can cause low platelet count. These include:
If a child has symptoms or signs of another problem, it might be secondary thrombocytopenia. This includes:
In these cases, more tests are needed to find the real cause.
A bone marrow test is not always needed for ITP. But, it might be needed in some cases. This includes:
“When the diagnosis is unsure or there are unusual signs, a bone marrow test might be needed,” say guidelines.
This test checks if the bone marrow can make platelets. It also helps rule out other bone marrow problems.
Treating pediatric Immune Thrombocytopenic Purpura (ITP) needs a careful plan. This plan considers how severe the ITP is and what each child needs. Doctors decide whether to treat or just watch based on several things. These include how likely the child is to bleed, their overall health, and how treatment might affect their life.
For mild ITP, doctors might just watch and wait. They check the child’s platelet counts often and look for any signs of bleeding. But if the ITP is more serious or if the child is bleeding a lot, they need to act fast.
Key considerations for observation vs. intervention include:
First treatments for pediatric ITP aim to quickly increase platelet counts. This helps lower the risk of bleeding. These treatments include:
These treatments often work well to manage bleeding and raise platelet counts.
For kids who don’t get better with first treatments or have chronic ITP, doctors might try other options. These include:
These options are used when the benefits are greater than the risks, and the child’s condition needs more help.
For severe or life-threatening bleeding, quick action is key. This might include:
“Immediate interventions, such as platelet transfusions, may be necessary to rapidly increase platelet counts and control bleeding.”
Emergency care is customized for each child’s needs and the bleeding’s severity.
It’s key to know how thrombocytopenia in kids will go. Immune Thrombocytopenic Purpura (ITP) in children often gets better on its own.
About 85% of kids with ITP get better within six months. This is a big part of knowing how well a child will do.
ITP in kids can be either acute or chronic. Acute ITP usually gets better in six months. Chronic ITP lasts longer.
Knowing if a child has acute or chronic ITP helps plan treatment. Acute ITP often needs little treatment because it gets better by itself. Chronic ITP might need more treatment and ongoing care.
Some things can tell if a child’s ITP will last a long time. These include:
Outcomes for kids with ITP depend on if it’s acute or chronic. Kids with acute ITP usually get better in a few months.
Kids with chronic ITP have a more mixed outcome. Some have ongoing low platelet counts, while others have times of better health. Keeping up with their care is very important.
We stress the need for a personalized approach to treating ITP in kids. This means looking at each child’s risk factors and how they react to treatment. This way, we can make their lives better and improve their health.
Children can have different types of thrombocytopenia, not just ITP. It can be caused by infections, leukemia, or genetic disorders. Knowing the types helps doctors diagnose and treat it right.
Neonatal thrombocytopenia is when newborns have low platelet counts. It can happen due to mom’s health issues, infections, or genes. A top pediatric hematologist says it’s critical to diagnose and treat it quickly to avoid problems.
There are two main reasons for neonatal thrombocytopenia. One is when mom’s antibodies against platelets pass to the baby. The other is infections or genetic issues that affect platelet making.
Some medicines can lower platelet counts, causing drug-induced thrombocytopenia. This can happen through an immune reaction or by harming the bone marrow. Antibiotics, anticonvulsants, and heparin are common offenders.
To diagnose, doctors look at the medicines the child is taking and run tests. If the drug is found to be the cause, stopping it is the first step. Sometimes, other treatments are needed to help platelet counts.
Genetic and inherited thrombocytopenias are caused by gene mutations. They can affect platelet counts in different ways. Wiskott-Aldrich syndrome and Bernard-Soulier syndrome are examples.
Doctors use genetic tests and look at platelet shape to diagnose. Treatment depends on the condition and may include platelet transfusions and other bleeding prevention measures.
Secondary thrombocytopenias happen because of another condition or disease. This can be due to infections like HIV or hepatitis C, cancer, or autoimmune diseases.
Treating the underlying cause is key to managing secondary thrombocytopenia. Sometimes, specific treatments are needed to help platelet counts and prevent bleeding.
In conclusion, thrombocytopenia in children comes in many forms. Knowing the different causes is vital for proper care.
Thrombocytopenia in children is a complex condition with many causes and symptoms. Immune thrombocytopenic purpura (ITP) is the most common type. Understanding its causes, symptoms, and treatments is key to managing it well.
At Liv Hospital, we offer complete care for children with thrombocytopenia. We use the latest evidence-based treatments. Our team is dedicated to providing top-notch care for international patients.
We know that low platelet counts can come from many sources. These include post-viral infections, post-vaccination reactions, and genetic factors. By understanding these causes, we can create treatment plans that meet each child’s needs.
At Liv Hospital, we care deeply about our patients. We provide compassionate and personalized care to children with thrombocytopenia. We are committed to helping them achieve the best health outcomes.
Thrombocytopenia in children means they have too few platelets. This can cause bleeding and bruising. The most common type is called immune thrombocytopenic purpura (ITP).
Thrombocytopenia in children can be caused by many things. This includes infections and vaccines. ITP happens when the body attacks and destroys platelets.
Symptoms of ITP in children can vary. They might have bruises, spots, or bleeding. Some kids might not show any signs at all.
Doctors use tests like a complete blood count (CBC) to find ITP. They also check to see if there are other reasons for low platelets.
Treatment for ITP in kids depends on how bad it is. Doctors might watch it, use steroids first, or try other treatments if needed.
How well kids with ITP do varies. Some get better quickly, while others have it for a long time. How long it lasts and how well it responds to treatment can help predict this.
Other types of thrombocytopenia in kids include neonatal, drug-induced, genetic, and secondary forms. Each has its own causes and effects.
Low platelet counts in kids can come from many sources. This includes ITP, infections, medicines, and genetic disorders.
ITP can make kids more prone to bleeding and bruising. This is a worry for active kids or those who play sports.
Acute ITP is short-term and usually goes away in a few months. Chronic ITP lasts longer and needs ongoing care.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!