Endometrial cysts, also known as endometriomas or chocolate cysts, are a common problem for millions of women. They happen when endometrial tissue grows outside the uterus. This can cause a lot of pain and affect a woman’s quality of life and fertility endo cyst.
At Liv Hospital, our team is here to help. We offer new, proven ways to find and treat endometrial cyst symptoms. We know how hard endometriosis cysts can be. We’re here to support you in managing your symptoms and finding the right treatment.
Key Takeaways
- Understanding endometrial cysts and their relation to endometriosis
- Recognizing the symptoms and their impact on women’s health
- Exploring diagnostic approaches for endometrial cysts
- Overview of treatment options for managing symptoms
- Support strategies for coping with endometrial cysts
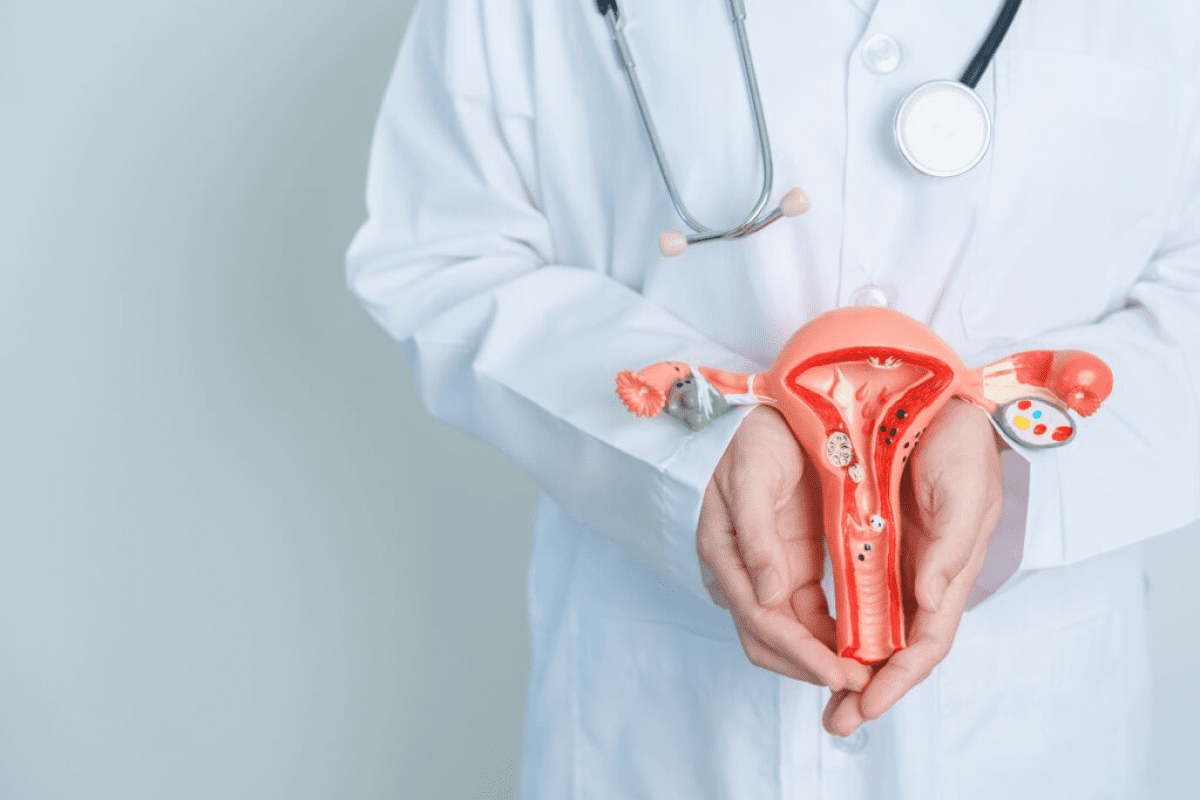
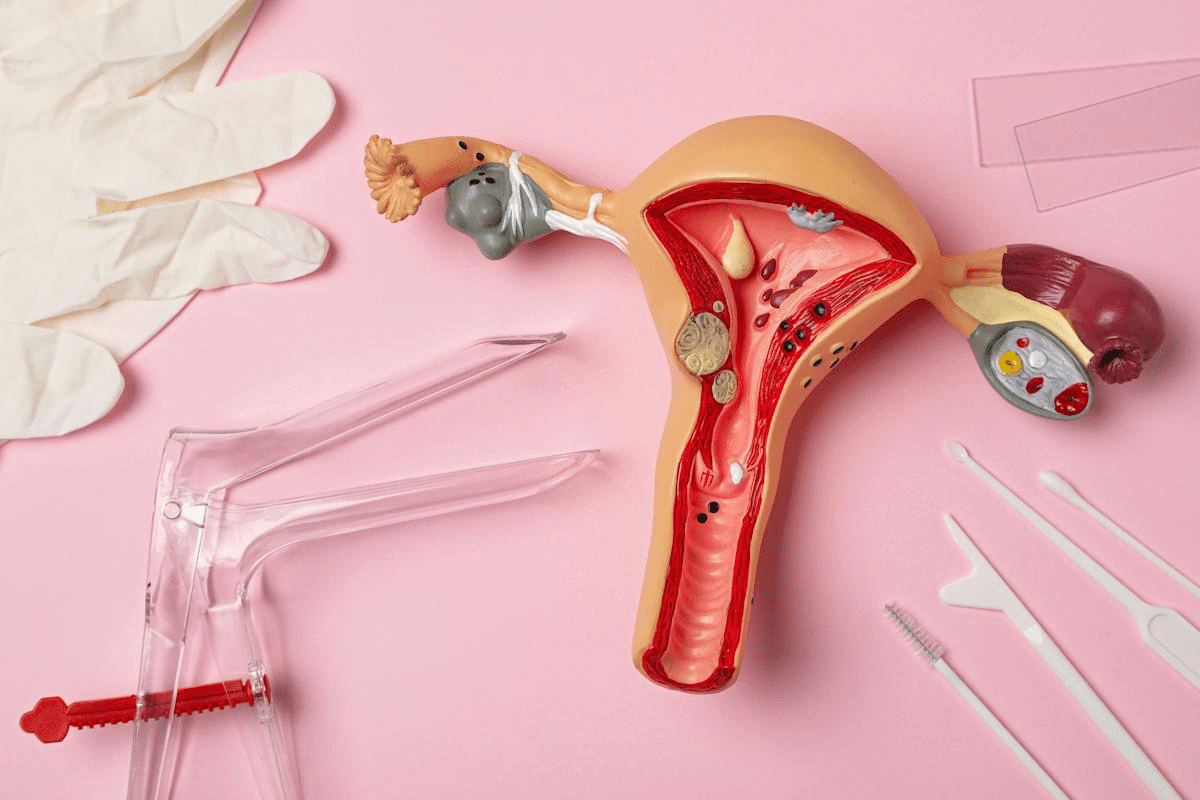
Understanding Endometrial Cysts
Endometriomas, or “chocolate cysts,” are a big worry for those with endometriosis. These cysts grow from the endometrium, the lining of the uterus. Their growth is complex, influenced by many factors.
What Are Endometriomas or “Chocolate Cysts”
Endometriomas are cysts that form when endometrial tissue grows outside the uterus. This leads to the buildup of menstrual blood and debris. The cysts are filled with a thick, dark fluid, earning them the nickname “chocolate” cysts.
These cysts often appear on the ovaries but can also be found on other pelvic structures. The growth of endometrial tissue outside the uterus is a key sign of endometriosis. This condition affects about 10% of women of reproductive age.
How Endometrial Cysts Develop
The growth of endometrial cysts is tied to the menstrual cycle. During menstruation, the tissue outside the uterus bleeds. This leads to inflammation and scarring, eventually forming cysts.
The exact reasons for endometrioma development are not fully known. Hormonal influences, genetic predisposition, and environmental factors are thought to play a role.
Prevalence and Risk Factors
Endometriomas are found in 17-44% of patients with endometriosis. This shows a strong link between the two conditions. Risk factors include a family history of endometriosis, early menstruation, and long menstrual periods.
Knowing these risk factors is key for early diagnosis and treatment of endometrial cysts. Healthcare providers can target interventions for those at higher risk. This helps to reduce symptoms and improve life quality.
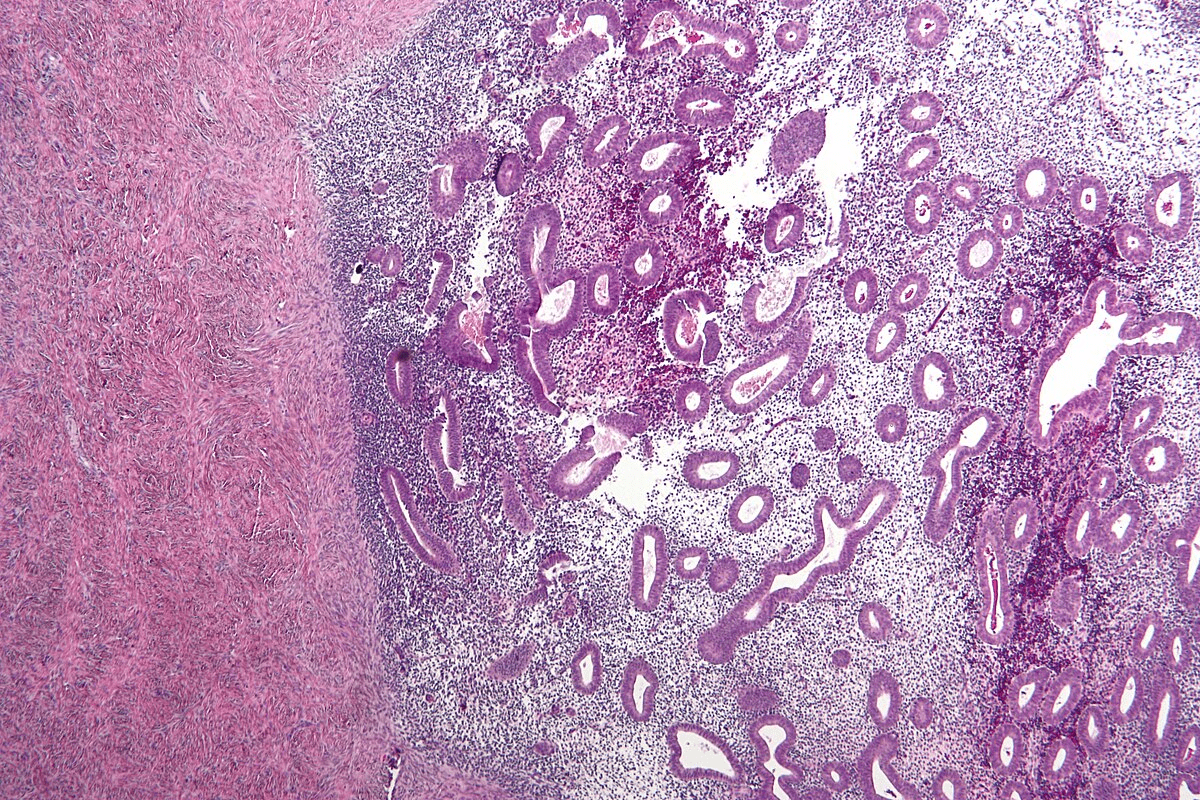
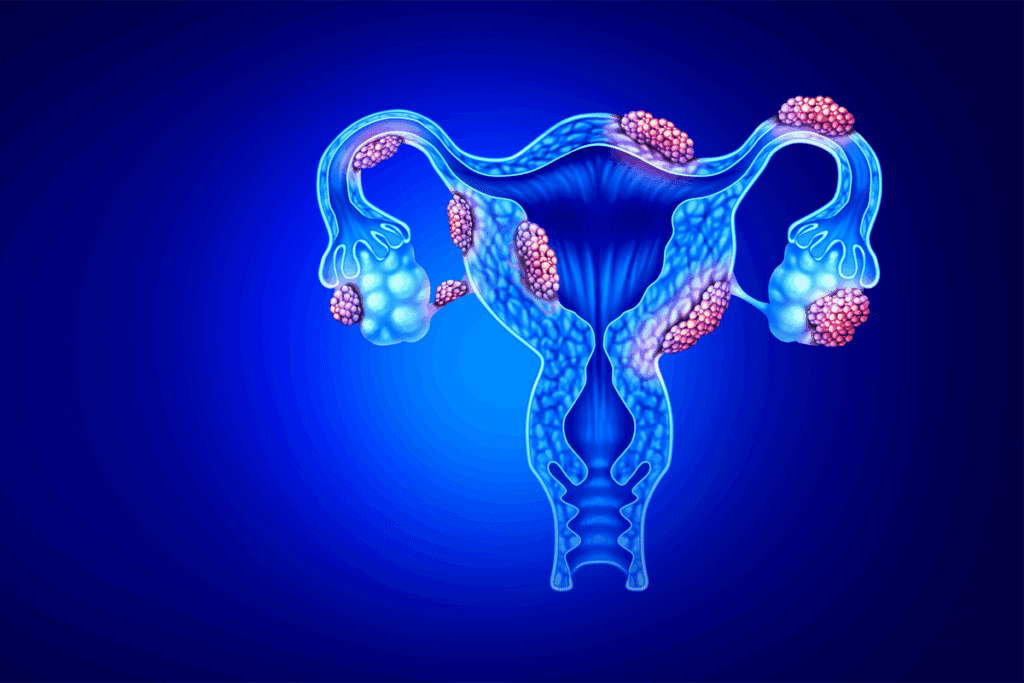
Types of Endo Cysts and Their Characteristics
It’s important to know about the different types of endometrial cysts to manage endometriosis symptoms well. These cysts are a key sign of endometriosis. Each type has its own traits that affect how they are diagnosed and treated.
Ovarian Endometriomas
Ovarian endometriomas, also called “chocolate cysts,” are common in endometriosis. They happen when endometrial tissue grows in the ovaries. This leads to cysts filled with old blood, making them look like chocolate.
Characteristics of Ovarian Endometriomas:
- Typically found on the ovaries
- Can cause pelvic pain and discomfort
- Associated with infertility issues
- Can vary in size, sometimes growing quite large
Subendometrial Cysts
Subendometrial cysts are found under the uterine lining. They can affect women of all ages. These cysts can cause pain and discomfort.
Key Features of Subendometrial Cysts:
Feature | Description |
Location | Beneath the uterine lining |
Demographics | Reproductive-aged and postmenopausal women |
Symptoms | Pelvic pain, menstrual irregularities |
Cysts in the Uterine Lining
Cysts in the uterine lining are another type of endometrial cyst. They can cause heavy menstrual bleeding and pelvic pain.
Characteristics and Implications:
- Can be associated with heavy menstrual bleeding
- May contribute to pelvic pain and discomfort
- Can be diagnosed through imaging techniques like ultrasound
Knowing about these different cyst types is key for doctors to create the right treatment plans for each patient.
Common Symptoms of Endometrial Cysts
Endometrial cysts can cause a lot of discomfort, like pelvic pain and irregular periods. These issues can really affect a woman’s life. They can make daily tasks hard, impact relationships, and lower overall happiness.
Pelvic Pain Patterns
Pelvic pain is a common symptom of endometrial cysts. This pain can show up in different ways, such as:
- Chronic pelvic pain that lasts a long time
- Dysmenorrhea, or painful menstruation, which can be severe
- Pelvic pain during or after physical activity
Pelvic pain patterns can vary significantly among women. The pain’s severity doesn’t always match the cyst’s size.
Menstrual Irregularities
Women with endometrial cysts often face menstrual irregularities. These can include:
- Heavy or prolonged menstrual bleeding
- Irregular menstrual cycles
- Spotting or breakthrough bleeding between periods
These issues can be upsetting and disrupt daily life.
Dyspareunia (Painful Intercourse)
Dyspareunia, or painful intercourse, is another symptom of endometrial cysts. This pain can happen during or after sex. It can cause a lot of distress for women and their partners.
As one study noted, “The experience of painful intercourse can have profound effects on a woman’s sexual well-being and intimate relationships.”
Fertility Implications
Endometrial cysts can also affect fertility. Women with these cysts might have lower fertility due to:
- Inflammation and adhesions in the pelvic region
- Distortion of the ovarian anatomy
- Hormonal and ovulatory disturbances
It’s estimated that 30-40% of women with endometriosis, which often includes endometrial cysts, experience infertility. Knowing how endometrial cysts affect fertility is key for women planning to have children.
In conclusion, the symptoms of endometrial cysts can be diverse and impactful. They can affect many areas of a woman’s life. Recognizing these symptoms is the first step towards getting the right medical care and managing the condition well.
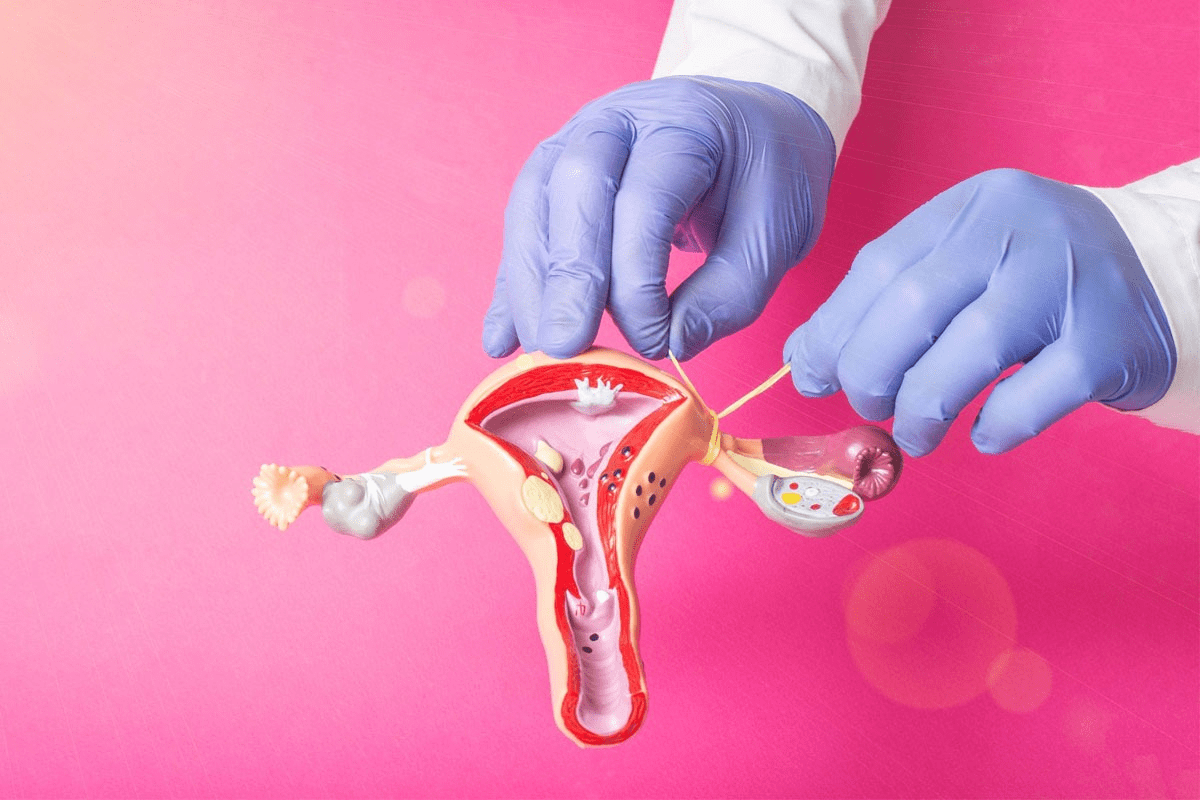
Diagnosing Endometrial Cysts
Diagnosing endometrial cysts is complex. It involves physical exams, imaging tests, and sometimes surgery. Getting an accurate diagnosis is key to finding the right treatment.
Physical Examination Process
A healthcare provider starts with a thorough physical exam. This includes a pelvic exam to check for any issues or tenderness. The goal is to find any signs of an endometrial cyst.
Imaging Tests (Ultrasound, MRI)
Imaging tests are vital for diagnosing endometrial cysts. Ultrasound is often the first choice, as it can spot cysts on ovaries. MRI may also be used for more detailed images to confirm the diagnosis.
Laparoscopy and Tissue Sampling
In some cases, a laparoscopy is needed. It involves a thin, lighted tube through a small incision. This allows for both diagnosis and treatment in one go.
Biomarkers and Blood Tests
Researchers are looking into biomarkers and blood tests for diagnosis. While not definitive alone, they may help identify who needs further testing.
By using these methods together, healthcare providers can accurately diagnose endometrial cysts. They can then create a treatment plan that meets the individual’s needs.
Medical Treatments for Symptom Relief
Many women find relief from endometrial cyst symptoms through medical treatments. These treatments aim to lessen pain, balance menstrual cycles, and boost life quality. We’ll look at the different medical options, like hormonal therapies and pain management.
Hormonal Contraceptives
Hormonal contraceptives are often the first choice for endometrial cyst symptoms. They help control hormonal changes that can cause cysts and pain. Birth control pills, patches, and vaginal rings are used to cut down on menstrual cramps, heavy bleeding, and cyst pain.
The benefits of hormonal contraceptives include:
- Reduced menstrual pain
- Regulation of menstrual cycles
- Decreased risk of new cyst formation
Progestins and Aromatase Inhibitors
Progestins mimic progesterone, a hormone key to the menstrual cycle. They help reduce endometrial tissue growth and ease symptoms. Aromatase inhibitors block estrogen production, which can help stop cyst growth. These are good for women who can’t use hormonal contraceptives or don’t respond well.
GnRH Agonists and Antagonists
GnRH agonists and antagonists are used to treat endometrial cysts. They lower estrogen levels, shrinking cysts and preventing new ones. Though effective, they can have side effects and are used for severe cases.
Pain Management Medications
Managing pain is key in treating endometrial cysts. Over-the-counter pain relievers like ibuprofen and naproxen help with mild to moderate pain. For severe pain, prescription drugs might be needed. It’s important to work with a healthcare provider to find the best pain relief.
Here’s a summary of the medical treatments discussed:
Treatment | Mechanism of Action | Benefits |
Hormonal Contraceptives | Regulate hormonal fluctuations | Reduce menstrual pain, regulate cycles, decrease new cyst risk |
Progestins | Reduce endometrial tissue growth | Alleviate symptoms, reduce cyst growth |
Aromatase Inhibitors | Block estrogen production | Reduce cyst growth, alleviate symptoms |
GnRH Agonists/Antagonists | Suppress estrogen production | Shrink existing cysts, prevent new ones |
Pain Management Medications | Relieve pain | Manage mild to severe pain |
Surgical Approaches for Endometrial Cysts
When other treatments don’t work, surgery is often needed for endometrial cysts. Surgery aims to remove the cysts without harming the ovaries. This is important for women who might want to have children in the future.
Conservative Surgery (Cystectomy)
Cystectomy is a common surgery for endometrial cysts. It involves:
- Removing the cyst while keeping the rest of the ovary safe
- Lowering the chance of the cyst coming back
- Helping with symptoms like pelvic pain and painful sex
Cystectomy is great for women who want to keep their fertility.
Ablation Techniques
Ablation methods destroy the cyst tissue instead of removing it. These methods are good for:
- Making the cyst smaller and easing symptoms
- Shortening recovery time
- Keeping the ovaries working well
Ablation is often chosen for smaller cysts or when surgery is too risky.
Considerations for Radical Surgery
In some cases, more serious surgery is needed. This includes:
- Oophorectomy (removing the ovary)
- Hysterectomy (taking out the uterus)
These surgeries are usually for women who have finished having children or have very bad symptoms.
Recovery and Post-Surgical Care
Recovering from surgery for endometrial cysts means:
- Watching for any problems
- Controlling pain after surgery
- Getting follow-up care to heal right
Good care after surgery helps prevent cysts from coming back and ensures the best results.
We know surgery is a big choice. Our team is here to give you all the care and support you need during and after surgery.
Daily Pain Management Strategies
Women with endometrial cysts face daily challenges in managing pain. There are several ways to ease this pain. These methods can make living with endometrial cysts more manageable.
Heat and Cold Therapy
Heat and cold therapy are simple yet effective pain management tools. A heating pad or warm water bottle on the lower abdomen relaxes uterine muscles and reduces cramps. Cold packs can also numb the pain for some women.
Over-the-Counter Pain Relief
Over-the-counter (OTC) pain medications are key for daily pain management. NSAIDs like ibuprofen are great for reducing pain and inflammation. Always follow the dosage and talk to a healthcare provider before starting any new medication.
Managing Flare-Ups During Menstruation
Menstruation often brings on endometrial cyst symptoms. To manage these, adjust your pain management plan and use more heat therapy or OTC pain relief. Keeping a symptom diary helps track patterns and prepare for flare-ups.
When to Seek Emergency Care
Knowing when to seek emergency care is vital. Severe pain, heavy bleeding, fever, or chills are signs of complications. Acting quickly can prevent serious health problems.
By using these strategies daily, women with endometrial cysts can manage their symptoms better. This improves their overall quality of life.
Lifestyle Modifications to Reduce Symptoms
Making lifestyle changes can help ease symptoms of endometrial cysts. By following certain diets, exercising regularly, getting enough sleep, and managing stress, you can manage your condition better.
Anti-Inflammatory Diet Approaches
An anti-inflammatory diet can lessen endometrial cyst symptoms. Eat foods high in omega-3s, antioxidants, and fiber. Stay away from processed foods and sugars.
- Add foods like salmon, spinach, and berries to your meals.
- Limit or avoid processed meats and sugary snacks.
Exercise and Physical Activity Benefits
Exercise benefits those with endometrial cysts by reducing pain and improving mood. Try yoga, swimming, or brisk walking.
- Do at least 30 minutes of moderate exercise daily.
- Try low-impact exercises like yoga or Pilates for flexibility and stress relief.
Sleep Hygiene and Symptom Management
Good sleep hygiene is key for symptom management. Stick to a regular sleep schedule, create a calm sleep space, and avoid stimulants before bed.
- Have a bedtime routine to signal sleep time.
- Steer clear of caffeine and screens before bed.
Stress Reduction Techniques
Stress reduction is essential for easing endometrial cyst symptoms. Use meditation, deep breathing, and mindfulness to lower stress.
- Practice mindfulness or meditation every day to reduce stress.
- Do things that make you happy and distract you from stress.
Complementary and Alternative Therapies
More people are looking into complementary and alternative therapies for endometrial cysts. These methods can help alongside traditional treatments. They aim to improve quality of life and offer extra relief.
Acupuncture and Traditional Chinese Medicine
Acupuncture is a big part of traditional Chinese medicine. It uses fine needles in specific body points to help heal and ease pain. Studies show it can lessen pain and improve symptoms in women with endometriosis, similar to endometrial cysts.
Benefits of Acupuncture:
- Reduces pelvic pain
- Improves menstrual regularity
- Enhances overall well-being
Herbal and Nutritional Supplements
Some herbal and nutritional supplements might ease symptoms of endometrial cysts. Here are a few:
Supplement | Potential Benefits |
Turmeric/Curcumin | Anti-inflammatory properties |
Omega-3 Fatty Acids | Reduces inflammation, promotes hormonal balance |
Vitamin D | Regulates hormonal pathways, improves symptoms |
Mind-Body Practices for Symptom Relief
Mind-body practices like meditation, yoga, and cognitive-behavioral therapy (CBT) are helpful. They manage emotional and physical symptoms of endometrial cysts.
Mind-body practices can reduce stress, improve coping, and boost well-being.
Some effective mind-body practices include:
- Meditation and mindfulness
- Yoga and tai chi
- Cognitive-behavioral therapy (CBT)
Managing Fertility with Endometrial Cysts
Women with endometrial cysts face challenges in getting pregnant. It’s key to know how to manage these cysts to improve chances of pregnancy. Endometrial cysts, or endometriomas, can harm fertility, so tackling the issue is vital.
Impact on Conception
Endometrial cysts can harm fertility in several ways. They can cause inflammation and adhesions in the pelvic area. This can damage ovaries and fallopian tubes, making it hard to conceive.
The cysts can also lower the quality of eggs and embryos. This makes getting pregnant even tougher.
Fertility Preservation Options
Women with endometrial cysts who want to conceive later have options. Egg freezing and embryo cryopreservation are available. These methods help preserve fertility before treatments like surgery or hormonal therapies.
Talking to a healthcare provider about these options is important. They can help choose the best plan for each woman’s situation.
Assisted Reproductive Technologies
Assisted reproductive technologies (ART) can help women with endometrial cysts get pregnant. In vitro fertilization (IVF) is a common method. It involves fertilizing eggs outside the body and then transferring the embryos to the uterus.
The success of ART depends on several factors. These include the woman’s age, egg and sperm quality, and other fertility issues.
Pregnancy Considerations with Endometriosis
Women with endometriosis, including those with endometrial cysts, need close monitoring during pregnancy. Pregnancy might ease symptoms, but there are risks to watch out for. These include preterm labor and placenta previa.
It’s important for obstetricians and endometriosis specialists to work together. This ensures a healthy pregnancy for these women.
Special Considerations for Postmenopausal Women
Endometrial cysts are less common in postmenopausal women. They bring unique challenges in diagnosis and treatment. As women age, the nature of these cysts and how they are managed changes a lot.
Prevalence and Presentation Differences
Endometrial cysts are much rarer after menopause. But when they do happen, they can be different. Postmenopausal women often feel pelvic pain or discomfort from these cysts.
Hormonal changes in postmenopause can affect endometrial cysts. Lower estrogen levels might change their size and symptoms.
Characteristics | Premenopausal Women | Postmenopausal Women |
Prevalence | Higher | Lower |
Symptoms | Often related to menstrual cycle | More likely to be persistent pelvic pain |
Hormonal Influence | Estrogen and progesterone fluctuations | Decreased estrogen levels |
Diagnostic Challenges
Diagnosing endometrial cysts in postmenopausal women is tough. They are rare, and other conditions can look similar. Ultrasound and MRI are key for diagnosis.
When checking for endometrial cysts in older women, we must think of many possible causes. This includes ovarian cancer and other pelvic issues.
Treatment Approaches for Older Women
Treating endometrial cysts in older women depends on several factors. These include the woman’s health, the cyst’s size and symptoms, and the risk of cancer. Surgery, like laparoscopy, is often used.
Personalized care is vital. We consider each patient’s health and wishes when choosing treatment.
For older women, surgery should be carefully considered. It depends on symptoms, cyst details, and the patient’s risk for surgery.
Conclusion
We’ve looked into endometrial cysts, from how they form to treatment choices. Handling endometrial cysts well means using medicine, changing your lifestyle, and sometimes surgery.
Getting relief from symptoms is key. Knowing your treatment options, like birth control and surgery, helps you choose the best path. Eating right and managing stress can also help lessen symptoms.
If you’re dealing with endometrial cyst symptoms, see a doctor. They can help you find ways to feel better and live better. Working with your doctor, you can make a plan that works for you.
With the right mix of medical help and self-care, managing endometrial cysts is possible. We urge you to be proactive in your care. Look into different treatments and lifestyle changes to help you.
FAQ
What are endometrial cysts, and how do they develop?
Endometrial cysts, also known as endometriomas, are cysts that form when endometrial tissue grows outside the uterus. This often happens on the ovaries. They develop due to abnormal growth of endometrial cells, influenced by hormones and other factors.
What are the common symptoms of endometrial cysts?
Symptoms can vary, but common ones include pelvic pain, irregular periods, painful sex, and fertility issues. Knowing these symptoms is key to getting the right medical help.
How are endometrial cysts diagnosed?
Diagnosing endometrial cysts involves a physical exam, imaging tests like ultrasound or MRI, and sometimes laparoscopy. Blood tests may also be used. A thorough diagnosis is important to find the best treatment.
What are the treatment options for managing endometrial cyst symptoms?
Treatments range from medical therapies like hormonal contraceptives and pain meds to surgery. We tailor treatment plans to each patient’s needs.
Can lifestyle modifications help alleviate symptoms of endometrial cysts?
Yes, making lifestyle changes can help. This includes an anti-inflammatory diet, regular exercise, good sleep, and stress reduction techniques.
How do endometrial cysts impact fertility?
They can cause inflammation, adhesions, and distortions that affect fertility. We discuss options like assisted reproductive technologies and fertility preservation with our patients.
Are there complementary therapies that can help manage symptoms?
Yes, therapies like acupuncture, herbal supplements, and mind-body practices can help manage symptoms. They are used alongside conventional treatments.
Do endometrial cysts continue to be a concern after menopause?
Yes, they can be a concern for postmenopausal women. We address the unique challenges and treatments for this stage.
Can endometriosis cause cysts, and what is the relationship between endometriosis and endometrial cysts?
Yes, endometriosis can lead to cysts, like ovarian endometriomas. We explore this connection and its impact on symptoms and fertility.
What is the role of hormonal therapies in managing endometrial cysts?
Hormonal therapies, like contraceptives and GnRH agonists, help manage symptoms by controlling hormone effects on endometrial tissue. We discuss these options in detail.
When should surgical intervention be considered for endometrial cysts?
Surgery is considered for severe symptoms, fertility issues, or when other treatments fail. We decide on surgery based on each case.
References
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK559230/