Many women hope that endometriosis symptoms will lessen after menopause. But, the truth is more complicated. Endometriosis is a long-term condition where tissue like the uterine lining grows outside the uterus. It affects millions of women globally.does endometriosis go awayWhat Is Excision Surgery for Endometriosis and How Does It Work?
Menopause does help many women feel better. Yet, some studies show that a small number of women keep feeling endometriosis pain even after their periods stop. At Liv Hospital, we offer trusted, patient-focused care for these postmenopausal challenges.
Key Takeaways
- Endometriosis is a chronic condition that affects millions of women worldwide.
- Menopause brings relief for many women, but some continue experiencing symptoms.
- Liv Hospital provides comprehensive care for women with endometriosis.
- Postmenopausal endometriosis requires specialized attention.
- Women’s experiences with endometriosis after menopause vary greatly.
Understanding Endometriosis as a Chronic Condition
Endometriosis is a chronic condition that needs ongoing care to manage its symptoms. It causes endometrial tissue to grow outside the uterus, leading to inflammation and scarring. This results in adhesions that can affect a person’s quality of life.
What Is Endometriosis and Who It Affects
Endometriosis often affects the ovaries, fallopian tubes, and the pelvis’s lining. It can greatly impact a person’s life, causing various symptoms. The exact cause is unknown, but hormones, genetics, and environment play roles.
Affected Population: About 1 in 10 women of reproductive age worldwide have endometriosis. The real number might be higher because it’s often underdiagnosed.
Common Symptoms and Diagnostic Challenges
Symptoms of endometriosis include pelvic pain, heavy or irregular bleeding, infertility, and digestive issues. Diagnosing it can be hard because symptoms vary and there’s no simple test. Laparoscopic surgery is often needed for a clear diagnosis.
Symptom | Percentage of Women Affected |
Pelvic Pain | 70-90% |
Heavy or Irregular Bleeding | 40-60% |
Infertility | 30-50% |
Impact on Quality of Life Before Menopause
Endometriosis can greatly affect a woman’s life before menopause. It can cause chronic pain and heavy bleeding. This can lead to fatigue, anxiety, and depression, making daily tasks hard.
For many, symptoms improve or go away after menopause because of lower estrogen levels. Knowing about endometriosis and its management is key to improving life for those affected.
The Relationship Between Hormones and Endometriosis
Hormones and endometriosis are closely linked. Endometriosis is sensitive to hormones, mainly estrogen. This hormone makes endometrial tissue grow, even outside the uterus.
Estrogen’s Critical Role in Endometriosis Development
Estrogen is key in growing endometriotic lesions. It makes endometrial tissue grow, causing pain and inflammation. Knowing how estrogen works helps in finding better treatments.
How Hormonal Fluctuations Affect Symptom Severity
Hormonal changes greatly affect endometriosis symptoms. Changes in estrogen levels, like during the menstrual cycle, can make symptoms worse. Symptoms often get better when estrogen levels are lower.
The Significant Hormonal Shift During Menopause
Menopause brings big hormonal changes, with estrogen levels dropping a lot. This drop can make endometriosis symptoms better for many women. But, 2 to 5 percent of postmenopausal women may keep experiencing symptoms, showing how complex the condition is.
In summary, hormones and endometriosis are deeply connected, with estrogen being a major player. Understanding these connections is key to managing endometriosis, even during big hormonal changes like menopause.
Does Endometriosis Go Away After Menopause?
Menopause changes a woman’s hormones, making some hope their endometriosis symptoms will get better. The decrease in estrogen can help ease symptoms. But, what really happens to endometriosis after menopause?
The General Rule: Symptom Improvement for Most Women
Most women see their endometriosis symptoms improve or go away after menopause. This is because estrogen levels drop, which helps endometriosis. The decrease in estrogen can cause endometrial lesions to shrink, easing symptoms.
Statistical Evidence of Postmenopausal Relief
Research shows many women feel better after menopause. While exact numbers vary, most agree that postmenopausal women have fewer severe symptoms. This evidence suggests menopause can end the pain for many.
Typical Timeframe for Symptom Resolution
How long it takes for symptoms to improve varies. Some feel better right after menopause, while others take years. The severity of endometriosis and hormone levels play a role in this.
What Medical Research Reveals About Recovery Rates
Medical studies shed light on recovery rates for endometriosis after menopause. While many see big improvements, some women may keep experiencing symptoms. Knowing what affects recovery helps doctors tailor care for each woman.
Even though menopause helps many, it’s not a cure for all. Symptoms persist for some, showing endometriosis’s complexity. This underlines the need for ongoing medical support.
When Endometriosis Persists: Exceptions to the Rule
Most women see their endometriosis symptoms lessen after menopause. But, a small group keeps experiencing pain. This is important to know about endometriosis.
The 2-5% Who Continue to Experience Symptoms
About 2-5% of women after menopause keep feeling endometriosis symptoms. This might seem small, but it affects many women worldwide. They don’t get relief from their symptoms, even after menopause.
These women often deal with pelvic pain, heavy bleeding, and other endometriosis symptoms. Their symptoms can last because of ongoing estrogen, endometrial lesions, and hormonal changes during menopause.
Risk Factors That Predict Symptom Persistence
Some factors can tell if endometriosis symptoms will keep going after menopause. These include:
- History of severe endometriosis: Women with severe endometriosis are more likely to keep feeling symptoms.
- Obesity: Being overweight can lead to more estrogen, making symptoms worse.
- Hormone replacement therapy (HRT): HRT, mainly estrogen-only, can make symptoms come back in some women.
Understanding Continued Pain Mechanisms
The reasons for ongoing pain in postmenopausal endometriosis are complex. Key factors include:
- Inflammation: Ongoing inflammation can keep irritating nerves and causing pain.
- Nerve sensitization: Long-term pain can make nerves more sensitive, increasing pain perception.
- Hormonal influences: Some estrogen is made even after menopause, which can affect endometriosis lesions.
Knowing these mechanisms is key to finding better treatments for women with ongoing endometriosis symptoms after menopause.
Recognizing Endometriosis Symptoms After Menopause
Menopause is a big change for women, but some may find that endometriosis symptoms don’t go away. It’s important to know how these symptoms can change and how to tell them apart from other health issues.
How Symptoms May Change After Menopause
After menopause, endometriosis symptoms can change because estrogen levels drop. Yet, some women may keep feeling pelvic pain, painful sex, and issues with bowel or urine. How often and how bad these symptoms are can differ a lot from person to person.
Studies in molecular biology show that endometrial lesions might make their own estrogen. This could be why some women after menopause keep feeling symptoms.
Distinguishing Endometriosis Pain from Other Conditions
Telling endometriosis pain from other health issues can be hard. Symptoms like pelvic pain can look like many other diseases. This includes problems with the gut, muscles, or other gynecological issues.
Getting a clear diagnosis is key. A doctor will need to look at your medical history, do a physical check, and might use imaging tests. This helps figure out what’s causing your pain.
Symptom | Endometriosis | Other Conditions |
Pelvic Pain | Common, can be cyclic or constant | Can be associated with various conditions, including PID, ovarian cysts, or musculoskeletal issues |
Bowel Symptoms | Can include painful bowel movements, constipation, or diarrhea | May be related to IBS, diverticulitis, or other gastrointestinal conditions |
Urinary Symptoms | Can include painful urination or frequency | May be related to UTIs, overactive bladder, or interstitial cystitis |
Bowel Endometriosis Symptoms in Postmenopausal Women
Bowel endometriosis can cause a lot of discomfort, like painful bowel movements, constipation, or diarrhea. For women after menopause, these symptoms can be hard to diagnose because they can look like other gut problems.
When we see postmenopausal women with bowel symptoms, we should think about bowel endometriosis. A detailed check-up, including imaging and endoscopy, is important to make a correct diagnosis.
The Science Behind Postmenopausal Endometriosis
Postmenopausal endometriosis involves many factors like hormones, genes, and how genes are turned on or off. Knowing about these is key to dealing with endometriosis symptoms after menopause.
Continued Estrogen Production After Menopause
Even after menopause, the body keeps making estrogen. Adipose tissue and skin are big sources of estrone, a type of estrogen. This estrogen helps endometriosis grow.
Studies show that a little estrogen is enough to keep endometriosis going. This is why some women with endometriosis keep feeling symptoms even after menopause.
Self-Sustaining Endometrial Lesions
Endometrial lesions can grow their own blood supply and make their own estrogen. This makes them keep growing even when estrogen levels are low.
- These lesions can invade nearby tissues, causing pain and discomfort.
- They might also resist hormone treatments, making treatment hard.
- The way these lesions adapt and survive makes treating postmenopausal endometriosis complex.
Genetic and Epigenetic Changes Affecting Estrogen Sensitivity
Genes and how they are turned on or off play a big role in endometriosis. These changes can make endometrial cells more sensitive to estrogen.
“The epigenetic modifications in endometrial cells can lead to an increased sensitivity to estrogen, facilitating the growth and maintenance of endometriotic lesions even in a postmenopausal environment.”
It’s important to understand these genetic and epigenetic changes for better treatments. Scientists are working hard to find new ways to treat postmenopausal endometriosis.
New-Onset Endometriosis After Menopause
Endometriosis can start after menopause, which is unusual. It’s a condition often linked to the reproductive years. Yet, some women are first diagnosed with it after menopause.
Can You Develop Endometriosis Years After Menopause?
Yes, it’s possible to get endometriosis years after menopause, though it’s rare. Research shows a small number of women are diagnosed with it after menopause. This brings up questions about what causes it at this age.
Delayed Diagnosis vs. New Development
It’s important to tell if endometriosis is a delayed diagnosis or a new case. Some cases might be a late discovery of endometriosis that was there before menopause. Others might be new due to certain risk factors.
Risk Factors for Postmenopausal Endometriosis
There are several risk factors for endometriosis after menopause. These include genetics, obesity, and a history of endometriosis. Knowing these risk factors helps in diagnosing and treating the condition.
Risk Factor | Description | Impact on Diagnosis |
Genetic Predisposition | Family history of endometriosis | Increases likelihood of diagnosis |
Obesity | Higher body mass index (BMI) | Associated with increased estrogen levels |
Previous History of Endometriosis | Previous diagnosis or symptoms | Higher risk of persistent or new lesions |
We know that endometriosis after menopause is rare but needs attention. Understanding the risk factors and the chance of new cases helps doctors provide better care. This way, they can support women with this condition more effectively.
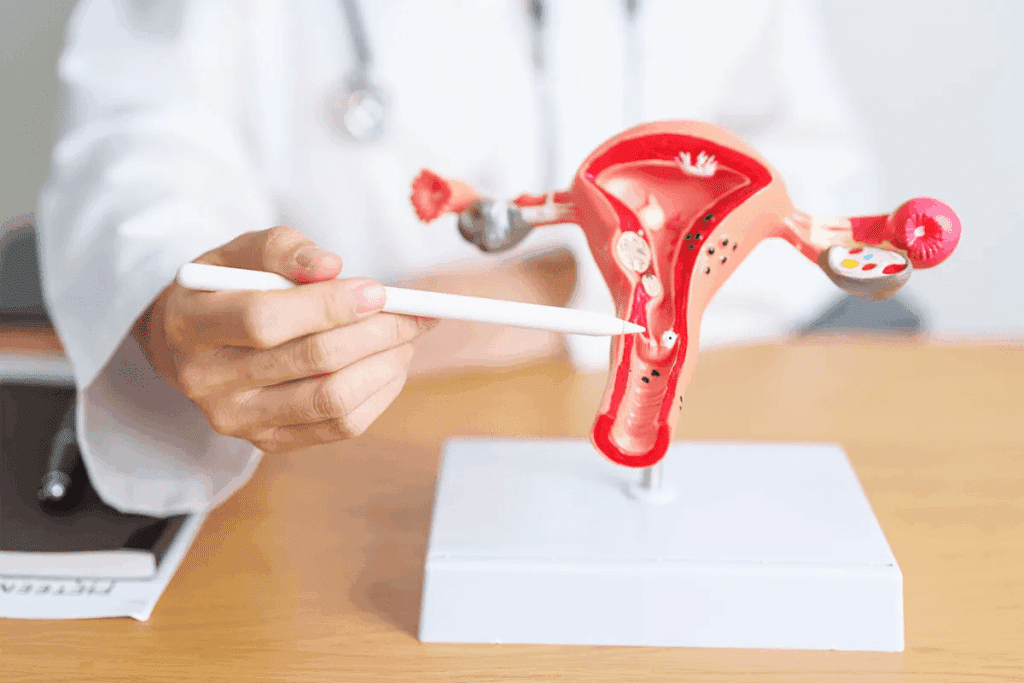
Treatment Options for Postmenopausal Endometriosis
Managing endometriosis after menopause needs a personalized plan. This plan aims to ease symptoms and boost quality of life. With lower estrogen levels, treatment shifts from reproductive years to focus on symptom relief and preventing issues.
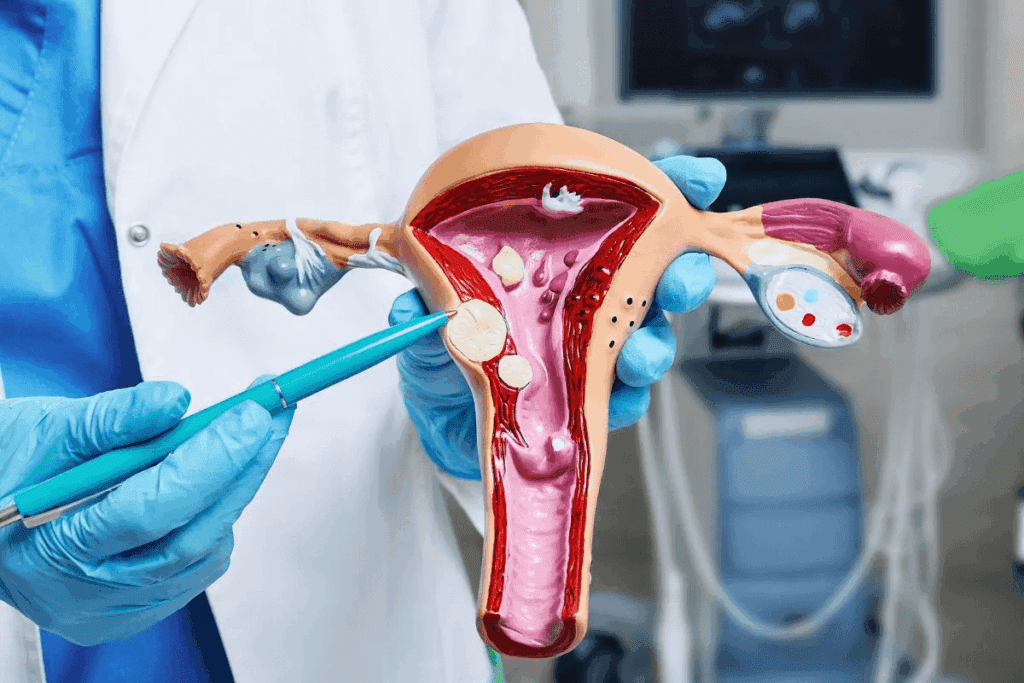
Surgical Approaches for Persistent Symptoms
Surgery is a key option for postmenopausal women with severe symptoms. It aims to remove painful endometrial lesions and adhesions. Before surgery, a detailed evaluation helps decide the best approach.
“Surgical intervention can offer significant relief for women with persistent symptoms,” says a leading gynecological surgery expert. “But, it’s important to consider the benefits and risks and the patient’s overall health.”
Medication Management Strategies
Medication is vital in managing symptoms of postmenopausal endometriosis. NSAIDs help with pain, and other meds address specific symptoms. We choose medications based on the patient’s health history and current status.
- Pain relief medications
- Hormonal therapies
- Alternative pain management options
Hormone Replacement Therapy Considerations
Hormone replacement therapy (HRT) is a topic of discussion for postmenopausal women with endometriosis. HRT can ease menopausal symptoms but needs careful consideration due to the risk of stimulating endometrial growth.
We stress the importance of discussing HRT’s risks and benefits with a healthcare provider. This helps make an informed decision.
Alternative and Complementary Treatments
Along with traditional treatments, alternative and complementary therapies can help. These include dietary changes, acupuncture, and holistic approaches. We encourage patients to explore these options with a healthcare professional’s guidance.
Dealing with postmenopausal endometriosis treatment shows that a multi-faceted approach works best. By considering various options and tailoring treatment to each individual, we can better manage symptoms and improve life quality.
Conclusion: Living Well with Endometriosis Beyond Menopause
Understanding endometriosis and managing it after menopause is key for better living. Symptoms may get better after menopause, but some women might keep experiencing them or get new ones.
There are many ways to manage endometriosis after menopause. This includes surgery, medication, and alternative therapies. It’s important to get care that fits each woman’s needs, as everyone’s experience is different.
Dealing with endometriosis means taking a full approach to health after menopause. Knowing how endometriosis works with hormonal changes helps women manage their health better.
Even though endometriosis can stick around or start after menopause, the right care can make a big difference. We aim to give women the knowledge and support they need to live well with endometriosis beyond menopause.
FAQ
Does endometriosis stop after menopause?
For most women, endometriosis symptoms lessen after menopause. This is because estrogen levels drop. But, some women might keep experiencing symptoms.
Can you stil have endometriosis symptoms after menopause?
Yes, some women keep feeling endometriosis symptoms after menopause. This is less common. Reasons include ongoing estrogen, self-sustaining lesions, and genetic changes.
What are the symptoms of endometriosis after menopause?
Symptoms after menopause are similar to before. These include pelvic pain, heavy bleeding, and bowel issues. But, how often and how bad these symptoms are can change.
How is endometriosis diagnosed after menopause?
Diagnosing endometriosis after menopause is hard. Symptoms can be like other conditions. Doctors use a detailed medical history, physical check-ups, and imaging tests like ultrasound or MRI.
What are the treatment options for postmenopausal endometriosis?
Treatments include surgery, medication, hormone therapy, and alternative methods. The right treatment depends on symptoms, medical history, and personal choices.
Can hormone replacement therapy (HRT) worsen endometriosis symptoms after menopause?
HRT might make symptoms worse in some women, if estrogen isn’t balanced with progesterone. But, the decision to use HRT should consider risks and benefits.
Is it possible to develop endometriosis after menopause?
Yes, it’s possible to get diagnosed with endometriosis after menopause. This could be due to a late diagnosis or new cases.
What are the risk factors for developing endometriosis after menopause?
Risk factors include a history of endometriosis, obesity, and genetic changes that affect estrogen sensitivity.
How can endometriosis pain be managed after menopause?
Pain can be managed with medication, lifestyle changes, and alternative therapies. A healthcare provider can create a personalized plan.
References
National Center for Biotechnology Information. Endometriosis: Visual Guide to Stages, Symptoms, and Diagnosis. Retrieved from
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1924845/