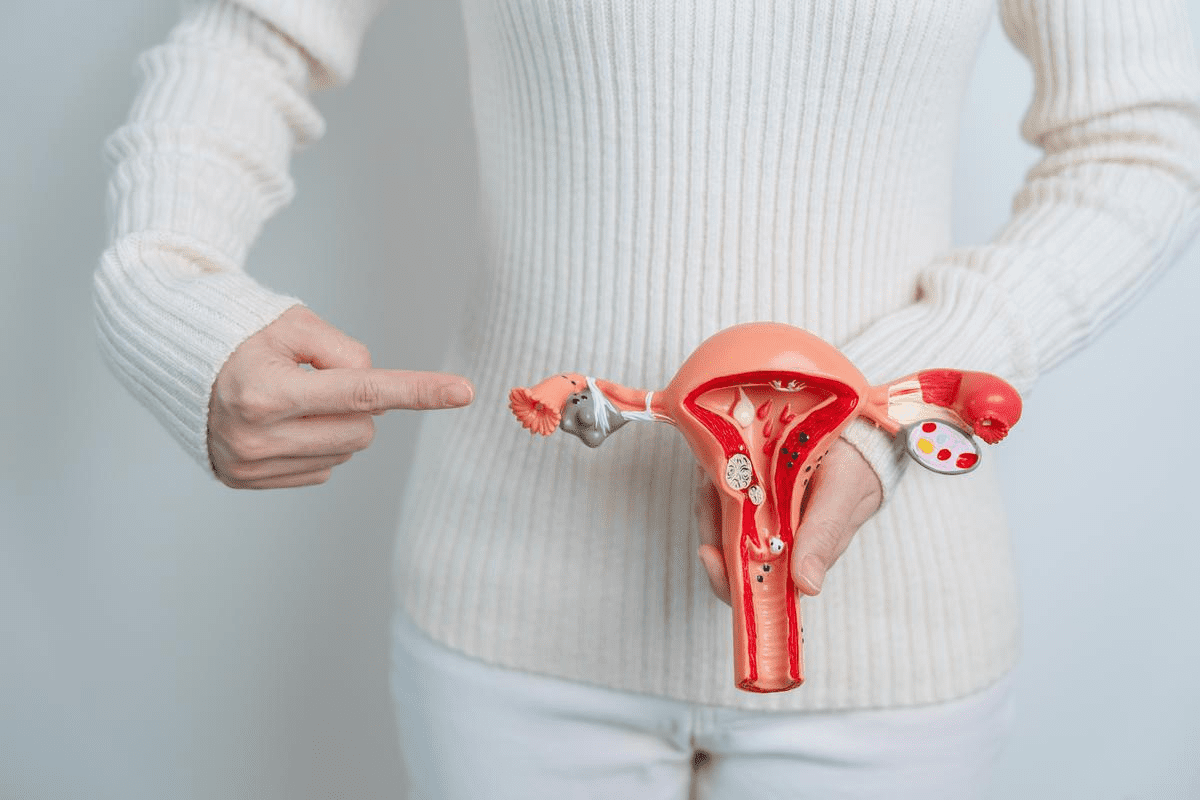
Endometriosis affects about 1 in 10 people assigned female at birth. It causes chronic pelvic pain and can affect fertility. Understanding the treatment options is key to improving quality of life.endometriosis medical procedureRobotic Surgery: An Amazing Example of a Procedure
At Liv Hospital, we use international expertise and personalized care for endometriosis. Our treatments range from pain management to surgery, tailored for each patient.
Effective management of endometriosis requires a deep understanding of the condition and treatments. We aim to provide top-notch healthcare and support for international patients.
Key Takeaways
- Endometriosis affects a significant number of women worldwide, causing pain and fertility issues.
- A range of treatment options are available, from non-surgical to surgical interventions.
- Personalized care is key for managing endometriosis effectively.
- Liv Hospital offers specialized endometriosis care with international expertise.
- Treatment approaches include pain management and surgical options.
Understanding Endometriosis
It’s important to understand endometriosis to help those dealing with it. This chronic condition happens when tissue like the uterus lining grows outside the uterus. It causes pain and discomfort.
What is Endometriosis?
Endometriosis is when endometrial-like tissue grows outside the uterus. This leads to inflammation, scarring, and adhesions. The misplaced tissue bleeds with each menstrual cycle, causing pain and other issues.
Prevalence and Risk Factors
Endometriosis affects about 1 in 10 people assigned female at birth. The exact number can vary. Several factors can raise the risk, like a family history, early menstruation, and certain reproductive tract issues.
Risk Factor | Description |
Family History | Having a first-degree relative with endometriosis may increase the risk. |
Early Menstruation | Starting menstruation before age 11 may be associated with a higher risk. |
Reproductive Tract Anomalies | Certain anomalies may obstruct menstrual flow, increasing the risk. |
Common Symptoms and Their Impact
Endometriosis symptoms vary but often include pelvic pain, heavy or irregular bleeding, and infertility. These symptoms can greatly affect daily life, impacting both physical and emotional health.
It’s key to recognize symptoms and understand the condition to manage endometriosis well. Knowing the prevalence and risk factors helps individuals get the right medical care and support.
Diagnosing Endometriosis
To find out if someone has endometriosis, doctors use many methods. They start with a physical check-up and might do more detailed tests like laparoscopy. Knowing the exact diagnosis helps doctors choose the right treatment.
Initial Evaluation and Physical Examination
The first step is talking about your health and doing a physical check. Doctors look at your symptoms, how often you get your period, and if your family has endometriosis. They might find tenderness or other signs in your pelvic area. But, some women with endometriosis might not show any signs during this check-up.
Key parts of the first check-up are:
- Talking about your health and periods
- Checking how symptoms affect your daily life
- Doing a pelvic exam to find any issues
Diagnostic Imaging Techniques
Imaging tests are also important for checking endometriosis. Doctors use:
- Ultrasound: It helps find endometriomas and check the ovaries.
- MRI (Magnetic Resonance Imaging): It gives clear pictures of the pelvic area, spotting implants and adhesions.
Even with these tests, some small implants or adhesions might not show up.
Laparoscopic Diagnosis: The Definitive Method
Laparoscopy is the best way to diagnose endometriosis. It’s a small surgery where a doctor looks inside the pelvic area through a tiny camera. This way, they can see endometrial implants and adhesions directly.
Laparoscopy has many benefits:
- It lets doctors see endometrial lesions clearly
- They can take biopsies to confirm the diagnosis
- They can also treat endometriosis during the surgery
Diagnostic Method | Advantages | Limitations |
Physical Examination | Non-invasive, first check | May miss some cases, like mild ones |
Ultrasound | Non-invasive, finds endometriomas | Can miss smaller implants or adhesions |
MRI | Gives detailed images, spots implants and adhesions | Costly, not always needed for first diagnosis |
Laparoscopy | Direct view, allows for biopsy and treatment | Requires surgery, needs skilled doctors |
By using these different ways to check for endometriosis, doctors can find out for sure if someone has it. Then, they can plan the best treatment for each patient.
Non-Surgical Treatment Approaches
Non-surgical treatments are key in easing endometriosis symptoms and boosting quality of life. They are effective in managing pain and other symptoms linked to endometriosis.
Over-the-Counter Pain Management
For many, managing endometriosis pain starts with over-the-counter (OTC) pain relief. Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen are often used to lessen pain and swelling. It’s important to stick to the recommended dosage and talk to a healthcare provider to avoid side effects.
- Ibuprofen: Effective for reducing pain and inflammation.
- Naproxen: Another NSAID that can help manage pain.
Hormone Therapy Options
Hormone therapy is a key part of treating endometriosis. It helps control hormonal effects on endometrial tissue, reducing symptoms. Common hormone therapy options include:
- Birth Control Pills: Continuous use can help reduce menstrual cramps and heavy bleeding.
- Gonadotropin-Releasing Hormone (GnRH) Agonists: These medications can decrease estrogen production, slowing the growth of endometrial tissue.
- Progestins: Synthetic progestins can help thin the lining of the uterus, reducing bleeding and pain.
Lifestyle Modifications for Symptom Relief
Along with medical treatments, lifestyle changes can also help with symptoms. These include:
- Dietary Changes: Eating a balanced diet rich in fruits, vegetables, and omega-3 fatty acids can help reduce inflammation.
- Regular Exercise: Physical activity can help reduce pain and improve overall well-being.
- Stress Management: Techniques like meditation and yoga can help manage stress, which is often associated with endometriosis symptoms.
By using these non-surgical treatment approaches, women with endometriosis can find significant relief from symptoms and improve their quality of life.
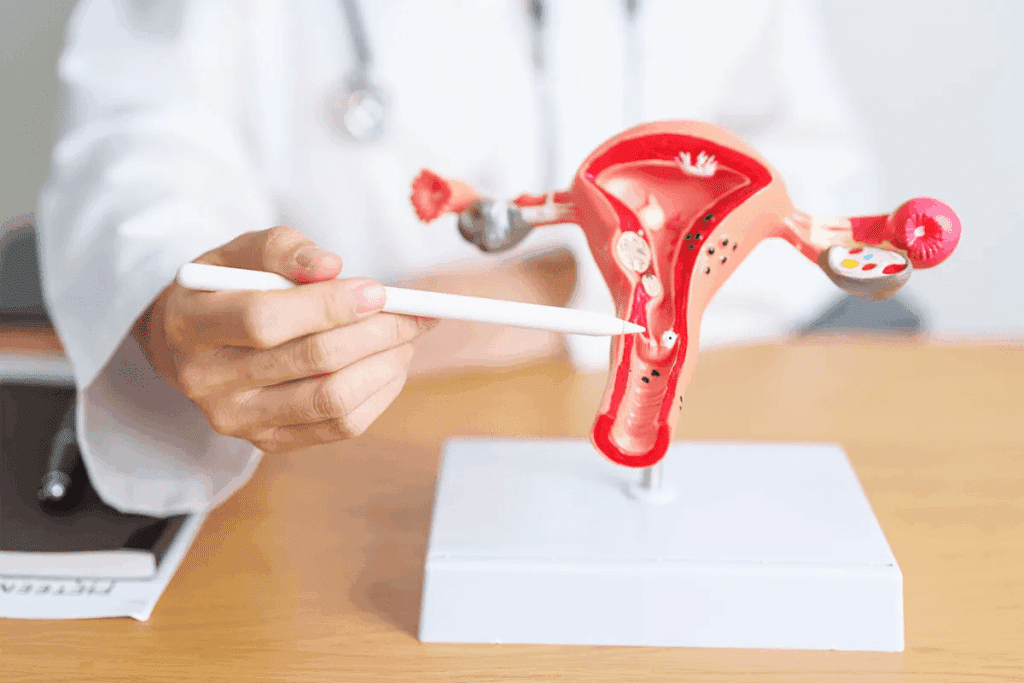
Endometriosis Medical Procedures: An Overview
Surgery for endometriosis includes many procedures to treat the disease. It’s important to know the different surgeries and what they mean.
Conservative vs. Definitive Surgical Approaches
There are two main types of surgery for endometriosis. Conservative surgery removes endometrial lesions but keeps the reproductive organs. This is for women who want to keep their fertility.
- Laparoscopic surgery is a common conservative method, known for its minimally invasive nature and quicker recovery times.
- It allows for the removal of endometrial growths and adhesions, helping to alleviate symptoms.
Definitive surgery includes more extensive procedures, like hysterectomy, where the uterus is removed. This is usually for women with severe symptoms who don’t plan to have more children.
When Surgery Is Recommended
Deciding to have surgery for endometriosis depends on several things. These include how bad the symptoms are, how much the disease has spread, and if the patient wants to have more children. Surgery is often suggested when:
- Symptoms are very bad and affect daily life a lot.
- Other treatments haven’t worked well enough.
- There are big endometriomas or a lot of adhesions.
Preparing for Endometriosis Surgery
Before surgery, talking to your doctor about risks, benefits, and other options is key. Preoperative preparation may include:
- Imaging tests to see how far the disease has spread.
- Looking at your medical history to find any risks.
- Talking about what to expect after surgery and how to recover.
Knowing about the different surgeries and what to expect helps patients make better choices for their care.
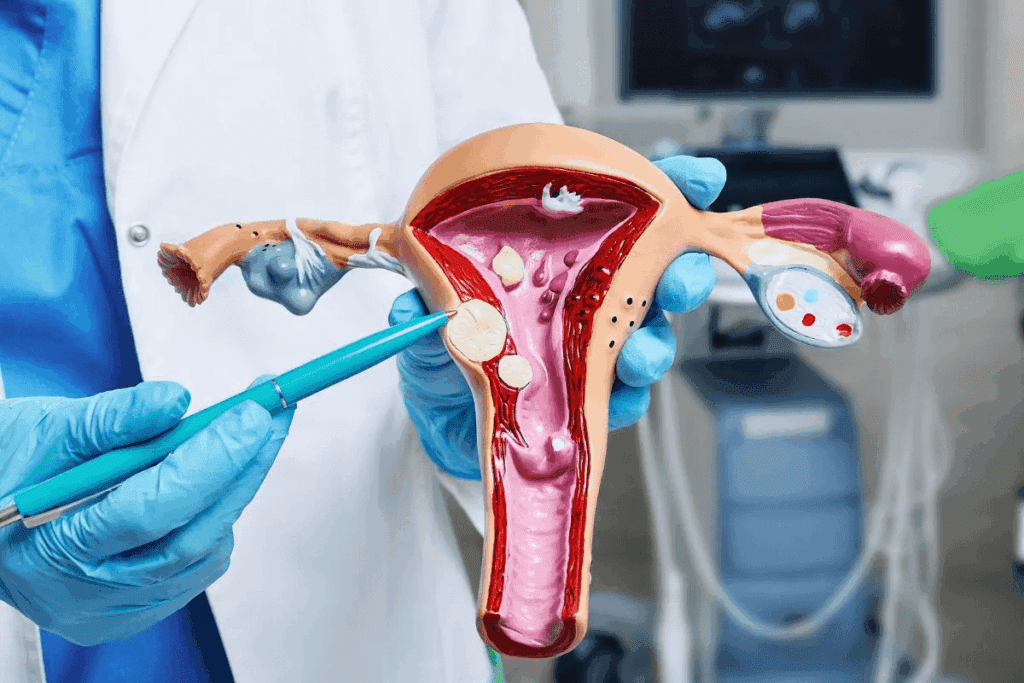
Laparoscopy: The Gold Standard Treatment
Laparoscopy has changed how we treat endometriosis. It’s a minimally invasive surgery that helps diagnose and treat endometriosis. Surgeons use small incisions to insert tools and a laparoscope. This lets them see and remove endometrial lesions without harming healthy tissue.
How Laparoscopic Surgery Works
First, patients get general anesthesia for comfort. Then, a small incision near the navel is made for the laparoscope. This gives a clear view of the pelvic organs on a monitor.
More small incisions are made for surgical tools. These tools help remove endometrial implants, cysts, and adhesions. The goal is to remove as much bad tissue as possible while keeping healthy tissue safe.
Laparoscopic surgery has many benefits. It uses smaller incisions, causes less pain, and has shorter hospital stays. This makes it a good choice for many women with endometriosis.
Recovery Timeline and Post-Op Care
Recovery time after laparoscopic surgery varies. Most women can get back to normal in a few weeks. Right after surgery, patients stay in a recovery room until they’re stable enough to go home.
After surgery, patients need to manage pain with medication, rest, and follow-up appointments. It’s important to follow the surgeon’s instructions to avoid complications and ensure a smooth recovery. This includes avoiding heavy lifting, strenuous activities, and sex for a while.
Success Rates and Recurrence Statistics
Laparoscopic surgery is very effective in managing endometriosis symptoms. Many women see a big improvement. But, success depends on the severity of the endometriosis, the surgeon’s skill, and the patient’s health.
Studies show that surgery can provide relief for several years. But, endometriosis can come back. The chance of recurrence depends on the stage of endometriosis, how well the surgery was done, and if the patient gets other treatments like hormone therapy.
It’s important to know about the chance of recurrence. This helps manage expectations and plan for the future. We work with our patients to create a treatment plan. This may include more surgeries, medical therapy, and lifestyle changes to manage symptoms and improve quality of life.
Laparotomy and Advanced Surgical Options
Advanced surgeries like laparotomy can help manage severe endometriosis. When simpler treatments don’t work, these more complex procedures might be needed.
When Laparotomy Is Necessary
Laparotomy involves a bigger cut in the belly. It’s used when smaller surgeries can’t reach the problem. This method lets doctors remove big growths or adhesions.
We suggest laparotomy when:
- Endometriosis has harmed nearby organs a lot.
- Smaller surgeries can’t get through because of too many adhesions.
- There are big endometriomas that need to be taken out.
Hysterectomy: Benefits and Limitations
Hysterectomy removes the uterus. It’s a strong treatment for endometriosis, best for women who don’t want more kids. But, it’s a big surgery with big effects.
The good things about hysterectomy are:
- It might stop endometriosis symptoms.
- It could lower the chance of it coming back.
But, there are downsides and things to think about:
- It’s a permanent choice that affects fertility.
- It might not solve all symptoms if the ovaries stay.
Procedure | Benefits | Limitations |
Hysterectomy | Potential elimination of symptoms, reduced risk of recurrence | Irreversible, impacts fertility, possible ongoing symptoms |
Laparotomy | Direct access for removal of endometrial growths, effective for complex cases | Larger incision, longer recovery time |
Oophorectomy and Its Long-term Implications
Oophorectomy removes the ovaries, sometimes with hysterectomy to stop endometriosis from coming back. But, it affects hormone levels and can lead to early menopause.
We might suggest oophorectomy if:
- The patient is close to menopause.
- There’s a big chance of ovarian endometriomas.
Long-term effects include:
- Instant menopause from surgery.
- Need for hormone therapy.
It’s important for patients and doctors to know about these surgeries. Each one has its own good and bad sides. The right choice depends on the person’s situation and health history.
Treating Endometriosis Cysts and Specific Complications
Endometriosis treatment focuses on managing issues like endometriomas and deep infiltrating endometriosis. These problems can really affect someone’s life, making it important to handle them well.
Endometriomas (Chocolate Cysts)
Endometriomas, or chocolate cysts, are filled with old blood. They’re a big problem for people with endometriosis, causing a lot of pain. To treat them, doctors might remove them surgically, which is safer for bigger cysts and can lower cancer risk.
Whether to remove a cyst depends on its size, how it makes you feel, and if you want kids. Laparoscopic surgery is often chosen because it’s less invasive and you heal faster.
Treatment Approach | Description | Benefits |
Surgical Removal | Laparoscopic surgery to remove the endometrioma | Reduces pain, potentially reduces cancer risk |
Hormonal Therapy | Using hormones to reduce cyst growth and symptoms | Avoids surgery, can reduce symptoms |
Deep Infiltrating Endometriosis Management
Deep infiltrating endometriosis (DIE) grows into tissues and organs, causing a lot of pain. Treating DIE needs a team effort, including surgery, hormones, and pain control.
Surgery for DIE is complex and aims to ease pain without harming organs. Expert surgical teams are key for the best results.
Adhesion Prevention and Treatment
Adhesions are fibrous bands that can form between organs or the wall of the abdomen. They often come from surgery or endometriosis. Doctors try to prevent adhesions during surgery to keep organs working right.
Addressing Endometriosis Blood Clots
Endometriosis can cause blood clots, mainly during menstruation. It’s important to manage heavy bleeding to stop clots. Hormones and pain relief can help with this.
Handling endometriosis complications well means a better life for those affected. Healthcare teams tailor treatments to meet each person’s needs, improving their quality of life.
Can Endometriosis Be Cured?
To understand if endometriosis can be cured, we need to look at today’s medical treatments. We must also know the difference between managing symptoms and completely getting rid of the condition.
Current Medical Understanding
Right now, there’s no surefire cure for endometriosis. But, different treatments can help control its symptoms and slow it down. We know endometriosis is complex, so treatment plans must fit each person’s needs.
Our doctors believe that a mix of medical treatments and lifestyle changes can greatly improve life for those with endometriosis.
Treatment vs. Cure: Setting Realistic Expectations
It’s key to understand the difference between treating and curing endometriosis. Treatments can ease symptoms, but because endometriosis is chronic, ongoing care is usually needed.
We want to be clear with patients about what treatments can do. We focus on how they can improve life quality, not cure the condition.
Does Endometriosis Go Away on Its Own?
Many wonder if endometriosis can just go away by itself. The answer is not simple. Some women might see their symptoms lessen, like after menopause.
But, this isn’t true for everyone. Many women keep dealing with symptoms their whole lives.
Long-term Prognosis and Management
The future outlook for people with endometriosis can vary a lot. Good management, like medical care and lifestyle changes, is key to a better life.
We help patients create plans that fit their needs. This way, they get care that’s just right for them.
Fertility Considerations and Treatment Options
Understanding how endometriosis affects fertility is key for those wanting to start a family. Endometriosis is when tissue like the uterus lining grows outside the uterus. This causes pain, inflammation, and can affect fertility.
The path to parenthood is tough for those with endometriosis. This condition can harm fertility by causing inflammation, adhesions, and changes in the reproductive organs.
How Endometriosis Affects Fertility
Endometriosis can lead to inflammation and scarring in the reproductive organs. This can block fallopian tubes or distort the uterus, making it hard for an egg to implant.
It also causes hormonal imbalances and ovulation problems, making it harder to conceive. We’ll look at how these factors work together and the treatments available to help with fertility.
Fertility-Preserving Surgical Approaches
Surgery is key in preserving fertility for those with endometriosis. Laparoscopic surgery is used to remove lesions, cysts, and adhesions that harm fertility.
By removing these issues, fertility chances improve. It’s important to talk to a healthcare provider about the benefits and risks of surgery to find the best option.
Assisted Reproductive Technologies
Assisted reproductive technologies (ART) like IVF are a way to have a child for many. ART can help overcome fertility problems caused by endometriosis.
We will work with fertility experts to create a treatment plan that fits each person’s needs. This increases the chances of a successful pregnancy.
Conclusion: Living with Endometriosis
Living with endometriosis means having a detailed treatment plan and making lifestyle changes. We’ve looked at many ways to manage it, from non-surgical methods to advanced surgeries.
Good treatment for endometriosis combines medicine and lifestyle changes. Knowing about the condition helps people choose the best care for themselves.
Dealing with endometriosis is tough, but the right support and treatment can help. It’s key to work with doctors to create a treatment plan that fits your needs.
Managing endometriosis in a holistic way can greatly improve your life. We’re here to offer support and help for those living with endometriosis.
FAQ
References
World Health Organization. Endometriosis Treatment: Procedures, Options, and Improving Quality of Life. Retrieved from https://www.who.int/news-room/fact-sheets/detail/endometriosis
Can endometriosis be cured?
No, there’s no cure for endometriosis. But, treatments can help manage symptoms and improve life quality.
How do you treat endometriosis?
Treatments include pain meds, hormone therapy, and lifestyle changes. Surgery like laparoscopy may also be needed, depending on the case.
What are the treatment options for endometriosis?
Options include pain relief, hormone therapy, and surgery. This includes laparoscopic surgery and hysterectomy. There are also ways to preserve fertility.
How is endometriosis diagnosed?
Diagnosis starts with an initial check-up and physical exam. Imaging and laparoscopy are also used to confirm endometriosis.
Does endometriosis go away on its own?
Sometimes, symptoms may lessen on their own. But, most cases need medical help to manage symptoms well.
Can you get rid of endometriosis?
You can’t completely get rid of endometriosis. But, treatments can greatly reduce symptoms and improve daily life.
What is the best treatment for endometriosis pain?
The best treatment combines pain meds, hormone therapy, and lifestyle changes. It’s tailored to each person’s needs.
How do you fix endometriosis?
Fixing endometriosis means a treatment plan. This may include medical, surgical, and lifestyle changes to manage symptoms and improve life quality.
Is there a cure for endometriosis?
No cure exists for endometriosis. But, treatments can manage symptoms effectively.
What are the surgical options for treating endometriosis?
Surgical options include laparoscopic surgery and hysterectomy. The choice depends on the case’s severity and the patient’s health and fertility.
How does endometriosis affect fertility?
Endometriosis can affect fertility by causing inflammation and adhesions. But, treatments and assisted reproductive technologies can help.
Can endometriosis be treated without surgery?
Yes, non-surgical treatments like pain management and hormone therapy can manage symptoms effectively.
What is the relationship between endometriosis and blood clots?
Endometriosis can lead to heavy menstrual bleeding and blood clots. Treatment may involve managing menstrual flow and addressing complications.
How do you remove endometriosis?
Removing endometriosis often involves surgery like laparoscopy. It aims to excise endometrial lesions and affected tissues.
Is endometriosis treatment available?
Yes, treatments are available to manage symptoms. These range from medical therapies to surgical interventions.
Can endometriosis be managed without medical treatment?
While lifestyle changes can help mild symptoms, most cases need medical treatment. This is to control symptoms and prevent complications.