Last Updated on December 2, 2025 by Bilal Hasdemir

Obesity affects millions of adults worldwide. In Canada, it impacts over 26% of adults. The Canadian Medical Association sees obesity as a chronic disease, needing obesity treatment health insurance coverage.Understanding the criteria for insurance coverage weight loss surgery and medications under various plans.
Understanding your health plan’s obesity coverage is essential for those seeking treatment. With healthcare costs rising, understanding what insurance coverage weight loss programs offer is vital. It can greatly affect treatment choices.
Key Takeaways
- Obesity is a recognized chronic disease.
- Insurance coverage for weight loss varies.
- Understanding health plan details is important.
- Comprehensive obesity treatment is available.
- Insurance can significantly impact treatment choices.
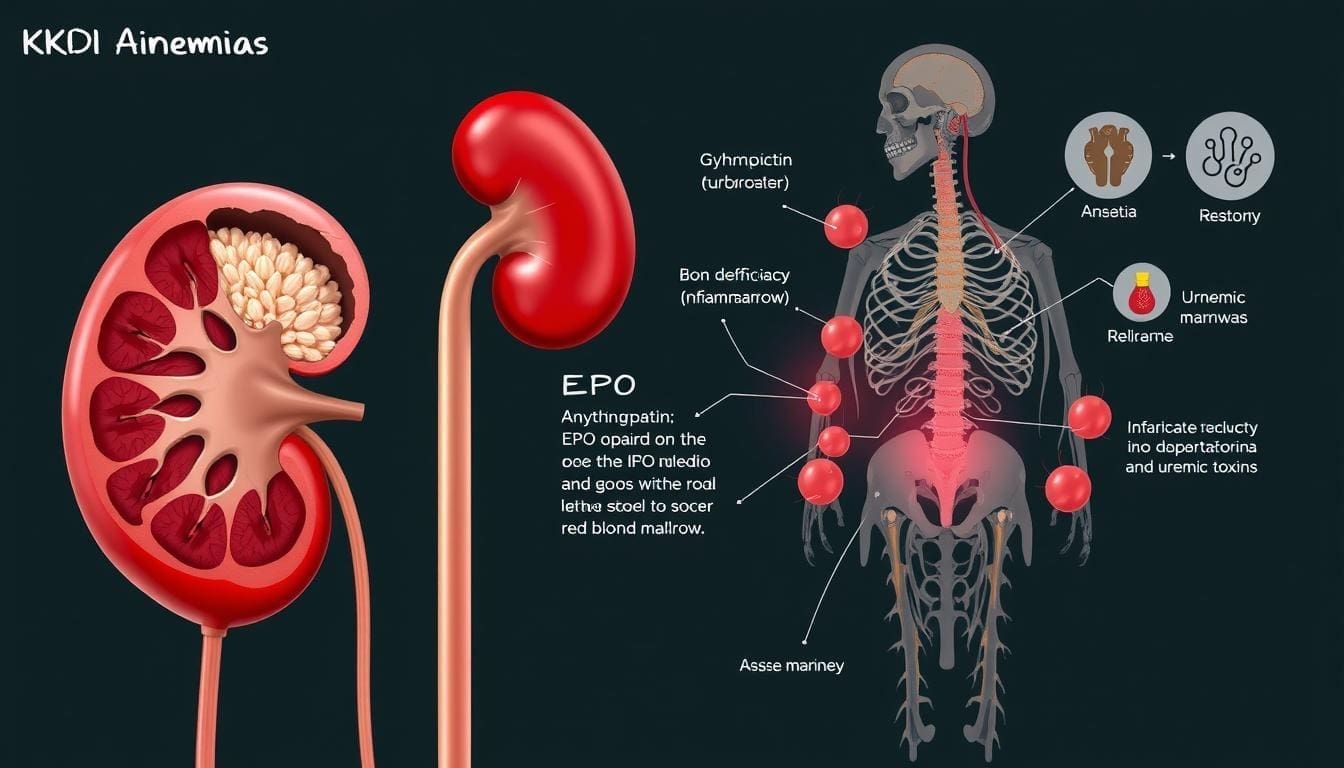
Understanding Obesity as a Medical Condition

Obesity is a complex health issue. The Canadian Medical Association has called it a chronic disease. This shows we need a full medical approach to treat it, which health insurance might cover.
Medical Definition of Obesity
Obesity is when your Body Mass Index (BMI) is 30 or higher. It means you have too much body fat. This can cause many health problems. The insurance required BMI level for treatments often starts here.
Health Risks Associated with Obesity
Obesity is linked to many health risks. These include diabetes, heart disease, and some cancers. These risks can really affect your life and healthcare costs. Knowing these risks helps figure out if insurance criteria weight surgery and other treatments are needed.
| Health Risk | Description |
| Diabetes | Increased risk of developing type 2 diabetes |
| Heart Disease | Higher risk of heart disease and stroke |
| Cancer | Increased risk of certain cancers, such as breast and colon cancer |
Health experts say obesity is a complex disease needing a detailed treatment plan. This plan might include diet changes, exercise, and sometimes obesity treatment health insurance covers medications or surgery.
Insurance Coverage for Weight Loss: An Overview
Insurance for weight loss treatments varies a lot. It depends on the insurance company and the plan details. It’s key for those looking into bariatric surgery, weight loss meds, and more.
To get insurance for weight loss, you must meet certain criteria. The main one is medical necessity. This is very important for weight loss treatments.
Medical Necessity Requirements
To get insurance, you need to meet specific medical needs. You usually need a high Body Mass Index (BMI). This is often 40 or higher. Or, you need a BMI of 35 or higher with obesity-related health issues.
- Having a high BMI
- Presence of obesity-related comorbidities
- Previous attempts at weight loss
Documentation Needed from Healthcare Providers
Healthcare providers are key in getting insurance approval. They need to provide the right documents. These include:
- A detailed medical history
- Documentation of previous weight loss attempts
- A letter of medical necessity
Knowing these requirements and working with healthcare providers helps. It makes getting insurance for weight loss treatments easier.
Types of Weight Loss Treatments Potentially Covered
Insurance plans may cover various weight loss treatments. This includes non-surgical programs and weight loss medications. Coverage depends on if the treatment is medically necessary, decided by a healthcare provider.
Non-Surgical Weight Loss Programs
Insurance often covers non-surgical weight loss programs if they’re needed. These programs offer dietary counseling, behavioral therapy, and lifestyle changes. Coverage can differ based on the insurance and the program. For example, some plans might cover visits to a registered dietitian or weight management programs.
Weight Loss Medications
Weight loss medications like Wegovy and Ozempic are popular, but coverage varies. Coverage for these medications often requires prior authorization and proof of medical need. Some plans cover certain medications, while others don’t. Always check with your insurance to see what’s covered under your plan.
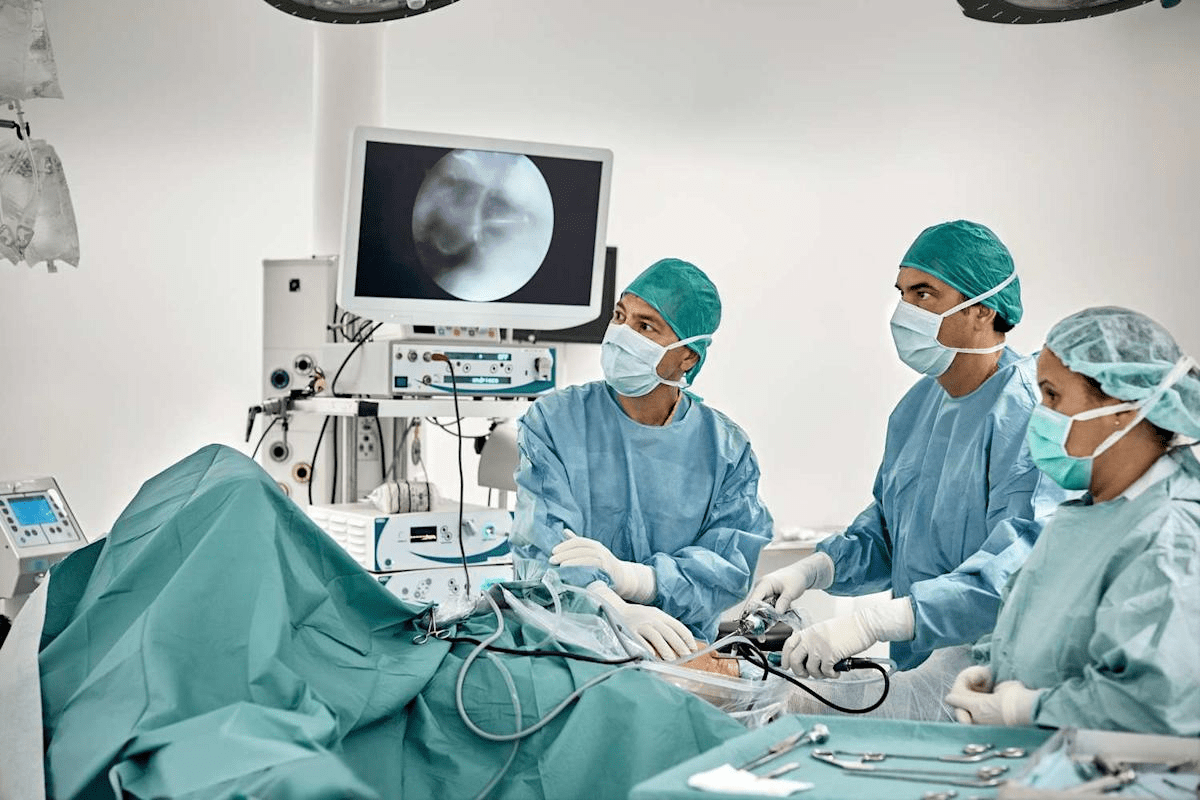
Bariatric Surgery Insurance Coverage
For those thinking about bariatric surgery, understanding insurance is key. These surgeries, like gastric bypass and lap band, can change lives. But, insurance rules vary a lot between companies.
To get insurance for bariatric surgery, you need to show it’s medically necessary. This means your doctor must say it’s needed for obesity and related health issues.
Gastric Bypass Insurance Coverage
Gastric bypass is a common surgery for weight loss. To get insurance, you usually need a BMI of 40 or more. Or, a BMI of 35 with obesity-related health problems. Getting approval from your insurance is a must, with a detailed look at your health history.
Gastric Sleeve Insurance Approval
Gastric sleeve surgery is another weight loss choice. To get insurance, the rules are similar to gastric bypass. Showing you’ve tried to lose weight before and have obesity-related health issues helps a lot.
Lap Band Covered by Insurance
Lap band surgery is a less invasive option. Insurance for lap band varies. Some insurers want you to try other weight loss methods first. Insurance depends on your health and obesity-related conditions.
In short, bariatric surgery is a great option for weight loss. But, dealing with insurance needs careful planning. Work with your doctor to meet insurance requirements.
- Check your insurance policy details for bariatric surgery coverage.
- Consult with your healthcare provider to understand the medical necessity requirements.
- Ensure you have thorough documentation of your obesity treatment history.
Insurance Coverage for Weight Loss Medications
More people are looking into weight loss medications like Wegovy and Ozempic. This has made it clear how important it is to know about insurance coverage for these drugs. As these treatments become more common, people want to understand how to deal with insurance for weight loss drugs.
Insurance plans differ a lot in what they cover for weight loss medications. Some might cover certain drugs under specific conditions. Others might not cover them at all.
Commonly Covered Weight Loss Drugs
Some weight loss medications are often covered by insurance, like Wegovy and Ozempic. These drugs help with weight management and type 2 diabetes. Whether or not you get coverage depends on your health and your insurance policy.
Prior Authorization Requirements
Getting insurance to cover weight loss medications often requires prior authorization. This means your doctor needs to get approval from your insurance before you can get the medication. The rules for getting this approval can change, but usually, you need to show it’s medically necessary and you’ve tried other weight loss methods.
Knowing the details of your insurance plan and the prior authorization process can make it easier to get the weight loss medications you need.
Medicare Bariatric Surgery Coverage
Medicare’s coverage for bariatric surgery has its own rules. It covers some types of surgery to help people with obesity. This can improve their health.
Eligibility Criteria for Medicare Coverage
To get Medicare coverage, you need to meet certain criteria. You must have a Body Mass Index (BMI) of 35 or more. You also need to have at least one health problem and have tried to lose weight before.
- Having a BMI of 35 or higher
- Presence of at least one comorbidity
- Previous attempts at weight loss through other means
Medicare Coverage Limitations
Medicare does cover some bariatric surgeries, but there are limits. It only covers surgeries that are really needed. This includes Roux-en-Y gastric bypass and laparoscopic adjustable gastric banding.
| Procedure | Medicare Coverage |
| Roux-en-Y Gastric Bypass | Covered |
| Laparoscopic Adjustable Gastric Banding | Covered |
| Sleeve Gastrectomy | Covered under certain conditions |
It’s key for patients to talk to their doctors. They can figure out the best treatment. And they can understand what Medicare needs for coverage.
Medicaid Obesity Surgery Approval
Medicaid coverage for obesity surgery varies a lot from state to state. Medicaid is a program shared by the federal and state governments. But, what surgeries are covered can change a lot from one state to another.
State-by-State Variations in Coverage
Every state has its own Medicaid program with its own rules. For example, some states might cover gastric bypass surgery. Others might also cover gastric sleeve or lap band procedures. It’s important to know these state-by-state variations if you’re looking for Medicaid to cover your surgery.
The rules for getting approved can also change. Some states might need more proof or have different BMI rules for who can get surgery.
Qualifying for Medicaid Weight Loss Coverage
To get Medicaid to cover weight loss surgery, you need to meet certain requirements. You must have a certain BMI, health conditions, and proof from doctors. Prior authorization is often needed, which means a detailed check of your health history and why you need surgery.
Working with your healthcare team to get the right documents and go through the approval process can help a lot. It can increase your chances of getting coverage.
Private Insurance Bariatric Benefits
The world of private insurance bariatric benefits is complex. Each insurance company offers different levels of coverage. This means people thinking about bariatric surgery need to check their insurance closely.
Major Insurance Providers’ Policies
Big insurance companies have their own rules about bariatric surgery. For example:
| Insurance Provider | Coverage Details | Pre-Approval Requirements |
| Blue Cross Blue Shield | Covers gastric bypass and gastric sleeve surgery | Requires documentation of medical necessity |
| Aetna | Covers bariatric surgery with certain criteria | Needs pre-approval and documentation of previous weight loss attempts |
| Cigna | Offers coverage for bariatric surgery with specific requirements | Requires pre-authorization and meeting certain health criteria |
Supplemental Coverage Options
Some people can buy supplemental coverage to help with bariatric surgery costs. This extra insurance can protect against unexpected bills.
Looking into supplemental coverage options is key. Make sure to understand what’s covered, any limits, and the cost of the insurance.
Insurance Required BMI Level and Other Eligibility Criteria
Insurance companies have specific rules for weight loss coverage. They look at your BMI and other health factors.
Standard BMI Requirements
Most insurance companies need a BMI of 40 or higher for surgery coverage. If your BMI is between 35 and 39.9, you might get coverage if you have health issues too.
| BMI Category | Typical Insurance Requirement |
| 40 or higher | Generally covered |
| 35-39.9 with comorbidities | Often covered with documentation |
| Below 35 | Typically not covered for surgery |
Comorbidity Considerations
Having health issues like diabetes or high blood pressure can affect insurance decisions. Insurance companies want proof of these conditions to approve weight loss treatments.
Common comorbidities considered by insurance providers include:
- Diabetes
- Hypertension
- Sleep apnea
- High cholesterol
Pre-Surgery Requirements
Before surgery, insurance companies need patients to go through evaluations and programs. This includes diet advice, mental health checks, and getting ready for surgery.
A typical pre-surgery requirement includes:
- Nutritional counseling
- Psychological evaluation
- Documentation of previous weight loss attempts
Affordable Care Act and Weight Loss Coverage
The Affordable Care Act has made big changes in how we treat obesity. It has added new rules for insurance to cover weight loss treatments.
Essential Health Benefits and Obesity Treatment
The Affordable Care Act says health plans must cover certain services. This includes obesity screening and counseling for adults. These are key parts of weight loss care.
Thanks to the ACA, people don’t have to pay a lot to get these services. This makes it easier for them to get the care they need.
Preventive Services Coverage
The ACA also requires coverage for preventive services. This includes obesity screening and counseling. People can get these services without paying extra.
This helps people get the help they need to lose weight. It’s a big part of the ACA’s plan to fight obesity.
| Service | Coverage under ACA | Out-of-Pocket Cost |
| Obesity Screening | Covered as Essential Health Benefit | No copay |
| Behavioral Counseling | Covered as Preventive Service | No coinsurance |
| Nutritional Counseling | Covered under some plans | Varies by plan |
Covered Weight Management Programs
Insurance often covers weight management programs. This shows how important a full approach to losing weight and staying healthy is.
These programs offer many services to help people reach and keep a healthy weight.
Nutritional Counseling Coverage
Nutritional counseling is key in weight management. Insurance covers nutritional counseling with experts to make meal plans just for you.
Insurance might also pay for group or one-on-one nutrition classes. These help people learn about eating well and planning meals.
Behavioral Therapy and Lifestyle Interventions
Behavioral therapy and lifestyle changes are also part of these programs. They help people change their eating and lifestyle habits that affect their weight.
Behavioral therapy includes counseling for emotional eating and managing stress. It tackles the psychological side of weight issues.
| Program Component | Description | Insurance Coverage |
| Nutritional Counseling | Personalized meal planning and nutrition guidance | Often covered, may require copay |
| Behavioral Therapy | Counseling for emotional eating and lifestyle changes | Typically covered, may have limitations |
| Lifestyle Interventions | Programs to promote physical activity and healthy habits | Varies by insurance plan |
Conclusion: Maximizing Your Weight Loss Benefits
Knowing what your insurance covers is key to getting the most out of weight loss treatments. This knowledge helps you make smart choices for your health.
Insurance might cover things like non-surgical weight loss programs, certain medications, and even bariatric surgery. To get the most from your coverage, you need to meet certain medical requirements. Your healthcare provider must also provide the right documentation.
Reviewing your insurance policy and talking to your doctor is a good first step. This way, you can find the best treatment for you. It helps you reach your weight loss goals without spending too much money.
By understanding your insurance and taking charge of your weight loss, you can improve your health. Start by looking over your insurance plan today. This is the first step to making the most of your weight loss benefits.
FAQ
What is considered a medically necessary weight loss treatment?
A medically necessary weight loss treatment is needed to treat a health issue like obesity. A doctor must recommend it. Insurance companies need proof of medical necessity to approve it.
What documentation is needed from healthcare providers to qualify for insurance coverage?
Healthcare providers must document a patient’s health issue, like obesity, and the treatment plan. This includes a letter of medical necessity, medical records, and test results.
Are non-surgical weight loss programs covered by insurance?
Some insurance plans cover non-surgical weight loss programs. This includes nutritional counseling and behavioral therapy. But, coverage depends on the insurance provider and plan.
What weight loss medications are commonly covered by insurance?
Insurance may cover certain weight loss medications. These include orlistat, phentermine, and lorcaserin. But, coverage varies by insurance provider and plan. Prior authorization may be needed.
What are the requirements for insurance coverage of bariatric surgery?
Insurance companies have specific criteria for bariatric surgery coverage. Patients must have a BMI of 40 or higher. Or, a BMI of 35 or higher with one or more health issues.
Is gastric sleeve surgery covered by insurance?
Gastric sleeve surgery may be covered by insurance. It must be deemed medically necessary. And, the patient must meet the insurance company’s criteria.
Does Medicare cover bariatric surgery?
Medicare covers bariatric surgery, like gastric bypass and gastric sleeve. Patients must meet certain criteria. This includes a BMI of 40 or higher, or a BMI of 35 or higher with health issues.
Does Medicaid cover obesity surgery?
Medicaid coverage for obesity surgery varies by state. Some states have more restrictive policies than others.
What are the insurance required BMI levels for weight loss coverage?
Insurance companies require a BMI of 30 or higher for weight loss coverage. Or, a BMI of 25 or higher with health issues.
How does the Affordable Care Act impact weight loss coverage?
The Affordable Care Act requires insurance plans to cover certain preventive services. This includes obesity screening and counseling. These services are covered without copays or coinsurance.
Are weight management programs, such as nutritional counseling, covered by insurance?
Some insurance plans cover weight management programs. This includes nutritional counseling and behavioral therapy. These programs are part of obesity treatment coverage.
What is prior authorization, and why is it required for weight loss medications?
Prior authorization is a process where insurance companies require approval before prescribing certain medications. It’s often needed for weight loss medications. This ensures they are used only when medically necessary.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4533773/