Last Updated on November 13, 2025 by
Why can’t you have chemo if your platelets are low? Learn the chemotherapy contraindications low platelets and the dangerous risks.
At Liv Hospital, we know that chemotherapy is a key treatment for many cancers. But it comes with risks. One big worry is how chemotherapy affects platelet counts. Platelets help our blood clot, and low counts mean a higher risk of bleeding.

When platelet counts fall below 50,000/ µL, the chance of bleeding is higher. And if they drop below 20,000/ µL, the risk of severe, life-threatening bleeding grows. We work hard to manage these risks for the best results for our patients.
Platelets are key to stopping bleeding by forming clots. Knowing how they work is vital for treating conditions like thrombocytopenia, a side effect of chemotherapy.
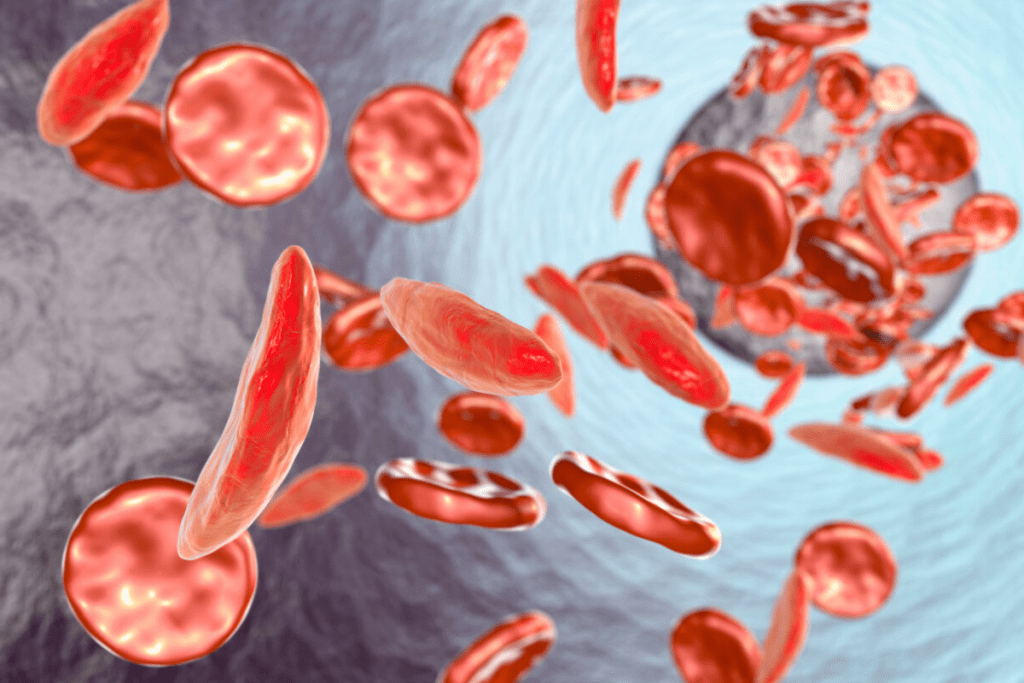
Platelets are small, colorless fragments in our blood. They form clots to stop bleeding. When a blood vessel gets hurt, platelets stick to it and attract more.
This creates a platelet plug that seals the injury. Platelets are essential for keeping our blood vessels healthy. Without enough, we face serious health problems.
A normal platelet count is between 150,000 and 450,000 per microliter of blood. Counts below this can mean thrombocytopenia, a bleeding risk. It’s key to watch platelet counts for those on treatments like chemotherapy.
Chemotherapy harms fast-growing cells, like cancer and platelet-making cells in the bone marrow. This can lower platelet production, causing thrombocytopenia. The impact of chemotherapy on platelet counts varies by treatment and patient.
Understanding this risk helps manage complications from low platelet counts during cancer treatment.
Thrombocytopenia is a big worry for cancer patients getting chemotherapy. It’s about having too few platelets in the blood. We’ll look at how this affects treatment and care for patients.
Doctors find thrombocytopenia by checking blood tests for platelet counts. A normal count is between 150,000 and 450,000 platelets per microliter. If it’s lower, it means you have thrombocytopenia.
Diagnosis involves: Blood tests to monitor platelet counts, mainly when patients are on chemotherapy. These tests help catch thrombocytopenia early.
The severity of thrombocytopenia is based on the platelet count. This helps doctors decide how to treat it. The severity levels are:
Thrombocytopenia is more common in some cancers, like leukemia. It’s because the disease can stop platelets from being made. It also depends on the chemotherapy used.
Knowing how common thrombocytopenia is in different cancers is key. It helps doctors find better ways to manage it. We’ll keep looking into this in the next parts.
Chemotherapy contraindications with low platelets are based on the increased risk of bleeding in these patients. When platelet counts drop too low, the chance of serious bleeding goes up. We make sure to delay or change treatment to keep patients safe.
Deciding to delay or change chemotherapy depends on how low the platelet count is. Counts under 50,000/ µL are often too low for chemotherapy because of the bleeding risk. Counts this low need careful thought and might mean changing treatment plans.
Studies show that chemotherapy should be adjusted if platelet counts are too low to avoid bleeding. Low platelet counts raise the risk of serious bleeding, mainly in those receiving intensive chemotherapy. The risk of bleeding also depends on other factors specific to the patient.
Our team carefully decides when to delay treatment due to low platelets. We look at how low the platelet count is, the patient’s overall health, and other treatment options. The main goal is to treat cancer effectively while avoiding bleeding risks. Sometimes, we might use platelet transfusions or special drugs to help platelets recover before starting chemotherapy.
Low platelet counts can lead to serious bleeding risks. This can be dangerous and even life-threatening. At Liv Hospital, we focus on understanding these risks to give our patients the best care.
The risk of bleeding is linked to platelet counts. Risk stratification based on platelet levels helps us spot patients at high risk. The lower the platelet count, the greater the risk of bleeding.
Those with very low platelet counts need extra care and close watch.
It’s important for patients to know the signs and symptoms of dangerous bleeding. Look out for small spots on the skin, bruises, and any bleeding that won’t stop. If you notice these, tell your doctor right away.
Some bleeding situations need quick medical help. This includes bleeding that won’t stop, big bruises, or signs of bleeding inside, like black stools or vomiting blood. Prompt action is key to avoiding serious problems.
At Liv Hospital, we teach our patients to spot these emergencies. We also offer support and resources to help them manage their condition well.
It’s key to know how often thrombocytopenia happens in people getting chemotherapy. This condition means not enough platelets in the blood. It’s a big worry when treating cancer, and chemotherapy makes it worse.
Research shows that how often thrombocytopenia occurs changes with different chemotherapy plans. Some treatments, like those that slow down bone marrow, raise the risk of low platelets. Here’s what we’ve found:
Grade III/IV thrombocytopenia is very serious, with platelet counts very low. This makes it hard for blood to clot, leading to a big risk of bleeding. People with this level of thrombocytopenia face:
We need to watch these patients closely and change their treatment plans to lower these risks.
Finding out who might get thrombocytopenia early is very important. We’ve found a few things that can help predict it, like:
Knowing these factors helps us make treatment plans that reduce the chance of thrombocytopenia and its problems.
Chemotherapy with low platelets can cause serious and even life-threatening problems. At Liv Hospital, we carefully check these risks to give our patients the best care.
Hemorrhagic complications are a big worry for patients with low platelets receiving chemotherapy. These can be from small bleeds to serious hemorrhages. “The risk of bleeding is a major factor in determining the safety of chemotherapy administration.” We do everything we can to lower this risk and make sure our patients get the right treatment to avoid these issues.
Thrombocytopenia can cause treatment delays, which can harm cancer treatment results. Delaying or modifying chemotherapy might make treatment less effective, leading to a poorer outcome. We aim to balance treating cancer effectively with managing low platelet risks.
“The management of thrombocytopenia is key to ensuring cancer patients can keep their treatment going without big breaks.”
Low platelet counts and related issues can really affect a patient’s quality. Fatigue, anxiety, and frequent medical visits can harm well-being. We focus on giving care that improves not just medical treatment but also life quality for our patients.
To deal with low platelet counts during chemotherapy, several strategies are used. Managing thrombocytopenia well is key to safely continuing cancer treatment.
Platelet transfusions are often used to manage severe thrombocytopenia. They increase platelet counts, lowering the risk of bleeding. The decision to give a transfusion depends on the patient’s platelet count, health, and bleeding risk.
Guidelines suggest transfusions for counts below 10,000/ µL. But, this can change based on the situation and other risk factors.
Thrombopoietic agents like romiplostim and eltrombopag boost platelet production in the bone marrow. They help manage chemotherapy-induced thrombocytopenia by increasing platelets, possibly reducing transfusion needs.
Managing thrombocytopenia sometimes means adjusting chemotherapy doses. This can include lowering the chemotherapy dose or changing the schedule to let platelet counts recover. Dose changes are made based on the patient’s health and the chemotherapy used.
These strategies help healthcare providers manage thrombocytopenia risks. This way, patients can keep up with their cancer treatment plans.
Patient education and self-monitoring are key in cancer care. They help patients stick to their treatment and stay safe. At Liv Hospital, we teach patients about their treatment and how to monitor their health.
Patients on chemotherapy should know the signs of low platelets, or thrombocytopenia. Common symptoms include:
Spotting these signs early can help patients get help fast. This can prevent serious bleeding problems.
Changing your lifestyle can lower bleeding risks during cancer treatment. Patients are advised to:
Patients need to know when to call their healthcare providers. They should seek immediate medical attention if they experience:
At Liv Hospital, we focus on patient-centered care. We give patients the support they need during treatment. Our goal is to help them manage their condition well and reduce risks.
“Empowering patients with knowledge about their treatment and possible side effects is a key part of our care. This way, they can actively participate in their recovery.”
Liv Hospital Care Team
Managing cancer treatment and platelet safety is a big challenge. At Liv Hospital, we get how complex it is. We balance the risks and benefits of chemotherapy and work to lower bleeding risks.
Dealing with low platelet counts in cancer patients is tricky. We aim to find the right balance between effective treatment and safety. Our goal is to give our patients the best care possible.
We focus on keeping platelet safety first and follow strict rules for chemotherapy. Our goal is to offer top-notch healthcare to international patients. We tailor our care to reduce risks from low platelet counts, making treatment more effective.
A low platelet count, or thrombocytopenia, occurs when the count is below 150,000 platelets per microliter of blood. Counts below 50,000/ µL increase the risk of bleeding. Counts below 20,000/ µL raise the risk of severe hemorrhage.
Chemotherapy targets cells that grow fast, like cancer cells and bone marrow cells. This can lower platelet production, leading to thrombocytopenia.
Chemotherapy with low platelets can cause severe bleeding. It may also need to be stopped. This can really affect a person’s quality of life.
We use different ways to manage thrombocytopenia caused by chemotherapy. This includes platelet transfusions and special drugs. We adjust treatment plans based on each patient’s needs.
Patients learn to spot signs like visible bleeding and bruising. They also know when to get medical help right away.
Yes, making lifestyle changes can help. Patients are told to avoid injuries and use soft-bristle toothbrushes. They should also be careful with sharp objects.
Our team carefully looks at the risks of low platelets. We balance these risks against the need for effective treatment. We might delay or change treatment to keep patients safe.
We focus on platelet counts but also check white blood cell counts. Chemotherapy can affect all blood cells. A normal white blood cell count is between 4,500 and 11,000 cells per microliter.
Leukopenia can be caused by chemotherapy. It can also be linked to certain cancers, like leukemia.
We manage white blood cell counts through medical care. Patients can also help by eating well, staying hydrated, and following our advice on managing side effects.
Gao, A., et al. (2023). Chemotherapy-induced thrombocytopenia: Literature review. Annals of Hematology, 102(1), 15-27. https://pmc.ncbi.nlm.nih.gov/articles/PMC9877263/
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!