How to avoid neutropenia during chemo? Follow the neutropenic protocol with this amazing and powerful guide to prevention and infection safety.
Chemotherapy-induced neutropenia is a big risk for patients. It can stop life-saving cancer treatments. Avoiding neutropenia needs a careful plan. This plan includes checking patients, using proven methods, and getting hospital help.
It’s key to use effective neutropenia precautions to lower this risk. Knowing the dangers and acting early can help a lot. This way, doctors can make treatments safer for patients.

Key Takeaways
- Assessing patient risk factors is key to preventing neutropenia.
- Using proven methods can greatly lower neutropenia risk.
- Hospital rules are important for managing neutropenia.
- Good communication among doctors is critical.
- Teaching patients about neutropenia precautions is essential for their safety.
Understanding Chemotherapy-Induced Neutropenia (CIN)
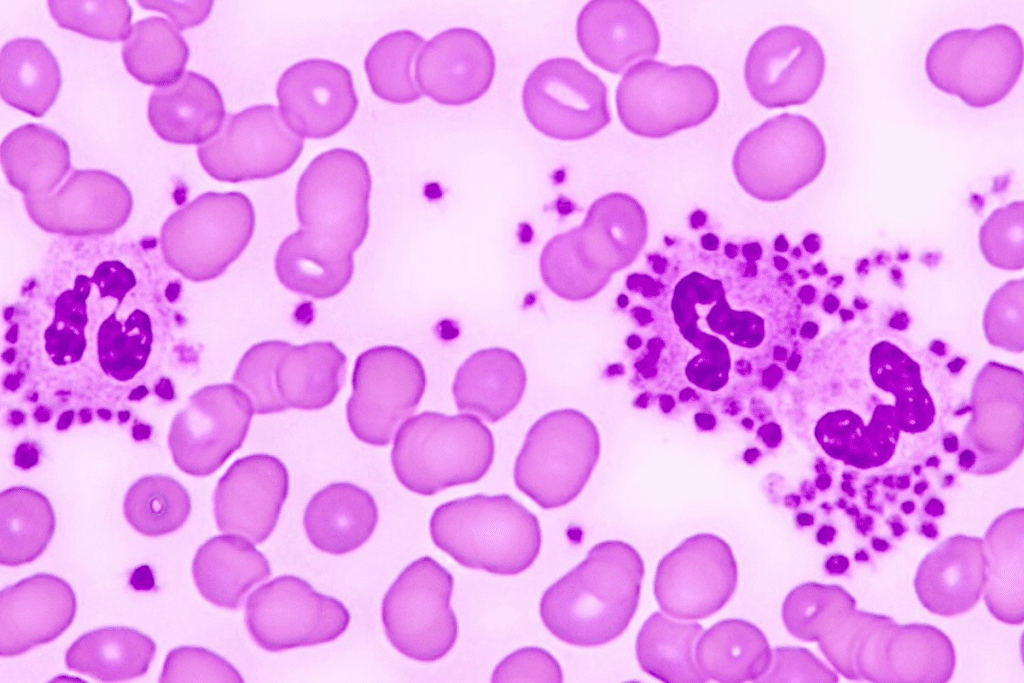
Chemotherapy-induced neutropenia occurs when patients have fewer neutrophils, a key white blood cell. It’s important to know about this to manage cancer treatment risks.
Definition and Mechanism of Neutropenia
Neutropenia means having less than 1500 neutrophils per microliter of blood. If it’s really low, below 500, the risk of getting sick goes up a lot. Chemotherapy harms both cancer cells and healthy cells, like neutrophils, causing neutropenia.

Prevalence Rates Across Different Chemotherapy Regimens
The chance of getting CIN varies from 10% to over 50%. It depends on the treatment and the patient’s health. Some treatments are more likely to cause it. Age, health, and past treatments also play a role.
Knowing these details helps in preventing and managing neutropenia. Taking neutropenic precautions and eating a neutropenic diet can reduce risks.
Understanding neutropenia helps patients and doctors lessen its effects on cancer treatment.
The Impact of Neutropenia on Cancer Treatment
Neutropenia is a common side effect of chemotherapy. It can make cancer treatment less effective by forcing doctors to lower doses or delay treatments. This condition increases the risk of infections and makes managing cancer harder, possibly affecting treatment success.
Treatment Delays and Dose Reductions
When neutropenia happens, doctors often have to change the chemotherapy plan. This might mean delaying or reducing the dose. These changes can make the treatment less effective because sticking to the original plan is key for the best results. For example, lowering the dose can make it harder to kill cancer cells.
Hospitalization Risks and Healthcare Costs
Febrile neutropenia (FN) is a serious issue that can lead to infections and often needs hospitalization. Hospital stays not only increase costs but also bring risks of infections and other problems. It’s important to have neutropenic precautions in hospital settings to lower these risks.
It’s vital to understand how neutropenia affects cancer treatment. This knowledge helps in finding ways to manage and prevent it. It can improve treatment results and cut down on healthcare expenses.
Assessing Your Risk for Neutropenic Complications
Every chemotherapy patient faces different risks of neutropenic complications. A personalized risk assessment is key. It helps find those at high risk and takes steps to prevent problems.
Patient-specific risk factors
Age, health, and past treatments can raise your risk of neutropenia. Older adults and those who’ve had radiation or neutropenia before are at higher risk. Spotting these factors early helps tailor your treatment to lower risks.
Chemotherapy regimen considerations
The type and strength of your chemotherapy matter a lot. Some drugs are more likely to cause neutropenia. Knowing your chemotherapy details helps your team prepare for and reduce risks.
Timing of neutropenia during treatment cycles
Neutropenia usually hits 7-14 days after treatment. Keeping an eye on your blood counts during these times is vital.
“The timing of neutropenia can vary depending on the chemotherapy regimen and individual patient factors.”
Regular check-ups and blood tests are key to catching and managing neutropenia early.
By grasping these factors and teaming up with your healthcare team, you can craft a plan to lessen your risk of neutropenic issues.
Medical Interventions to Prevent Neutropenia
Medical treatments, like G-CSF therapy, are key in stopping neutropenia in patients receiving chemotherapy. Neutropenia is a big side effect of chemo that can cause delays, dose cuts, and higher costs.
Granulocyte-Colony Stimulating Factor (G-CSF) therapy
G-CSF therapy boosts the production of granulocytes, a white blood cell type, to stop neutropenia. Prophylactic administration of G-CSF cuts down febrile neutropenia (FN) and helps get chemo on time.
Timing and administration protocols
The timing and how G-CSF is given change based on the chemo plan and patient risks. Usually, it’s given subcutaneously or intravenously 24-48 hours after chemo.
Effectiveness rates and considerations
Research shows G-CSF therapy works well in lowering neutropenia and FN risks in chemo patients. But, how well it works depends on many things, such like the chemo type, patient age, and health.
Some important things to think about with G-CSF therapy are:
- Patient-specific risk factors for neutropenia
- Chemotherapy regimen and dose intensity
- Timing and duration of G-CSF therapy
Understanding G-CSF therapy’s role in preventing neutropenia helps healthcare providers make good plans to lower this risk. This supports patients going through chemo.
Neutropenic Precautions: Essential Guidelines
Neutropenic precautions are key to reducing infection risks during chemotherapy. They help protect patients with weak immune systems from harmful pathogens. These steps are essential to keep patients safe.
Hospital-Based Neutropenic Precautions
In hospitals, patients with neutropenia are kept in private rooms. This reduces their exposure to infections. Healthcare staff must wash their hands often and wear protective gear when near the patient.
Key measures include:
- Using sterile equipment and supplies
- Limiting visitor access
- Avoiding contact with individuals who are sick
Home-Based Neutropenic Precautions
At home, patients need a safe space to avoid infections. They should stay away from sick people and keep their environment clean. It’s also important to avoid polluted areas.
Important home-based precautions include:
- Avoiding crowded areas and public places
- Using a mask when going outside
- Maintaining good hygiene practices, such as frequent handwashing
When to Implement Precautionary Measures
Start neutropenic precautions when a patient’s neutrophil count drops below 500 cells per microliter. It’s important for patients to follow their healthcare team’s advice on when to start and stop these measures.
Monitoring and adjusting precautions based on:
- Neutrophil count levels
- Presence of fever or other signs of infection
- Changes in overall health status
The Neutropenic Diet: Food Safety and Nutrition
A well-planned neutropenic diet can greatly lower the chance of getting infections during chemotherapy. This diet aims to cut down on harmful bacteria and other germs in food.
Food Preparation Guidelines
Keeping food safe is key. This means cooking food well, avoiding raw or undercooked meats, and making sure all tools and surfaces are clean.
Using a food thermometer is a good way to check if meats are cooked right. It’s also important to keep raw and cooked foods separate to avoid contamination.
Foods to Avoid During Neutropenic Periods
Some foods are riskier and should be skipped durinneutropeniaic. These include raw or undercooked eggs, unpasteurized dairy, and raw sprouts.
Also, avoid deli meats and hot dogs unless they’re heated up well. Make sure to wash fresh fruits and veggies before eating them.
Nutritional Strategies to Support Immune Function
Eating a balanced diet is vital for a strong immune system. This means getting enough protein, vitamins, and minerals.
Try to eat a variety of foods, like lean proteins, whole grains, and colorful fruits and veggies. Drinking lots of water is also key.
Healthcare experts say, “A balanced neutropenic diet is very important for chemotherapy patients. It helps lower infection risks and aids in recovery.”
Infection Prevention Strategies for Neutropenic Patients
Keeping infections away is key for those with neutropenia, often caused by chemo. People with neutropenia are more at risk because their immune systems are weak. So, it’s important to use good prevention methods.
Personal Hygiene Practices
Good personal hygiene is a must to stop infections. Frequent handwashing with soap and water or an alcohol-based sanitizer is very effective. Also, showering or bathing daily helps keep the skin clean.
Environmental Considerations
The environment also plays a big part in preventing infections. Neutropenic patients should steer clear of crowded places and stay away from sick people. Keeping their living space clean and well-ventilated at home can also help.
Avoiding Infection Sources
It’s important to stay away from things that could cause infections. This means avoiding raw or undercooked foods and being careful around pets and their waste. Patients should also watch out for places with infection risks, like construction sites.
By following these steps, neutropenic patients can lower their chance of getting infections. This makes their treatment safer.
Monitoring for Signs of Neutropenic Fever
Spotting neutropenic fever early is key to better treatment. It’s a serious condition that needs quick action and care.
Temperature Monitoring Protocols
People getting chemo should learn how to check their temperature correctly. They need to use a thermometer correctly and log their temperature often. This is most important when they’re at risk for neutropenia.
Early Warning Signs of Infection
Signs of infection include fever, chills, sore throat, cough, shortness of breath, or pain when urinating. Patients should watch for these signs and tell their doctor right away.
When to Seek Immediate Medical Attention
If a patient feels feverish or shows other signs, they should see a doctor immediately. Quick action can stop serious problems from neutropenic fever.
The Role of Multidisciplinary Care in Managing Neutropenia
Multidisciplinary care is key in reducing neutropenia risks in chemotherapy patients. It involves a team effort, patient education, and clear communication.
Coordination between Oncology, Nursing, and Pharmacy
Oncology professionals, nurses, and pharmacists must work together. Nurses are essential in teaching patients about infection prevention and watching for fever signs. Pharmacists help by managing medications like G-CSF to prevent neutropenia.
Good teamwork ensures patients get the best care. Regular talks and planning help spot and fix problems quickly.
Patient Education and Support Resources
Teaching patients about neutropenia is vital. They need to know about neutropenic precautions, diet tips, and how to watch for fever.
- Understanding neutropenia risks and their impact on treatment
- Learning how to prevent infections at home
- Knowing the early signs of neutropenic fever
Communication Strategies with Your Healthcare Team
Good communication between patients and healthcare teams is critical. Patients should ask questions and share concerns. Regular check-ins with doctors can catch problems early and improve care.
Using a team approach to manage neutropenia can lead to better care for chemotherapy patients. This can greatly improve their health outcomes.
Advanced Approaches to Neutropenic Management
New treatments and personalized care are changing how we manage neutropenia. These new methods and plans are helping patients get better and avoid complications.
Emerging Therapies and Research
New Granulocyte-Colony Stimulating Factor (G-CSF) therapies are showing great promise. Researchers are working hard to find more ways to lessthea’s effects.
- Investigational drugs targeting specific pathways involved in neutropenia
- Novel formulations of existing therapies to improve efficacy and safety
Personalized Medicine Approaches
Personalized medicine is key in fighting neutropenia. It lets doctors tailor treatments to each patient. This way, they can make chemotherapy safer and more effective.
Genetic profiling and biomarker analysis are being explored to predict patient-specific risks and guide treatment decisions.
Clinical Trials and Future Directions
Clinical trials are vital for improving neutropenic care. They test new treatments and strategies. This research will lead to better care for patients in the future.
Healthcare providers need to keep up with the latest in neutropenic management. This way, they can give patients the best care during chemotherapy.
Thrombocytopenia and Other Blood Count Concerns During Chemotherapy
Blood count issues, like thrombocytopenia, can make cancer treatment harder. Patients often face many blood count problems. It’s important to manage these issues well.
Managing Multiple Cytopenias Simultaneously
Handling multiple blood count problems at once is tough. It needs a team effort to lower risks. Key strategies include:
- Regular monitoring of blood counts
- Adjusting chemotherapy dosages
- Implementing supportive care measures
Monitoring Complete Blood Counts
It’s key to keep an eye on complete blood counts (CBCs) regularly. CBCs spot problems early, so we can act fast. Key components of CBC monitoring include:
- How often should to take blood tests
- Checking white blood cell, red blood cell, and platelet counts
- Changing treatment based on CBC results
Complementary Approaches to Blood Count Support
Some non-medical ways can also help with blood counts. These include eating right, changing your lifestyle, and managing stress.
Conclusion: Creating Your Neutropenia Prevention Plan
Creating a neutropenia prevention plan is key for those getting chemotherapy. Knowing the risks and taking steps to prevent them can lower the chance of neutropenic problems.
Doctors and nurses are important in teaching patients about neutropenia precautions. Working with their healthcare team, patients can make a plan that fits their needs. This includes tips on preventing infections, what to eat, and watching for fever signs.
A good prevention plan helps patients manage their care better. It can also reduce the need for treatment delays and hospital stays. By following the advice in this article, patients can do better in their treatment and live a better life.
FAQ’s:
What are neutropenic precautions?
Neutropenic precautions are steps taken to lower the risk of getting sick. They are for people with low neutrophil counts, often during chemo. These steps include avoiding big crowds, wearing masks, and keeping clean.
What is a neutropenic diet?
A neutropenic diet is a special meal plan for those with weak immune systems. It aims to keep food safe and nutritious to fight off infections. Foods to avoid include raw meats, unpasteurized dairy, and unwashed fruits and veggies.
How can I avoid neutropenia during chemotherapy?
To avoid neutropenia, a mix of patient care, evidence-based treatments, and hospital support is needed. This includes using G-CSF therapy, following neutropenic precautions, and sticking to a neutropenic diet.
What is the role of G-CSF therapy in preventing neutropenia?
G-CSF therapy boosts neutrophil production, reducing the risk of neutropenia and febrile neutropenia. It helps ensure chemotherapy can be given on time, without delays.
When should I implement neutropenic precautions?
Start neutropenic precautions when your neutrophil count is low, usually during chemo. The exact timing depends on your risk factors and treatment plan.
How can I manage thrombocytopenia during chemotherapy?
Managing thrombocytopenia means watching blood counts, avoiding bleeding, and possibly getting platelet transfusions. Working closely with your healthcare team is key.
What are the signs and symptoms of neutropenic fever?
Neutropenic fever is a high temperature over 38 °C (100.4 °F) in people with low neutrophil counts. Look out for chills, sweating, and feeling unwell. Seek medical help right away if you have these symptoms.
How can I support my immune system during chemotherapy?
To support your immune system, eat well, follow neutropenic precautions, and drink plenty of water. Foods high in antioxidants and fiber can also help.
What is the importance of monitoring complete blood counts during chemotherapy?
Checking complete blood counts is vital to catch changes in blood cell counts. It helps doctors adjust treatments and add support as needed.
How can I work with my healthcare team to manage neutropenia?
Managing neutropenia requires teamwork between you and your healthcare team. They should teach you about neutropenic precautions, diet, and watching for signs.
Reference
Punnapuzha, S. (2023). Febrile neutropenia. In StatPearls. National Library of Medicine. https://www.ncbi.nlm.nih.gov/books/NBK541102/
Blayney, D. W., et al. (2022). Chemotherapy-induced neutropenia and emerging agents for its treatment. European Journal of Cancer Care, 31(5), e13456. https://www.sciencedirect.com/science/article/pii/S0305737222000913