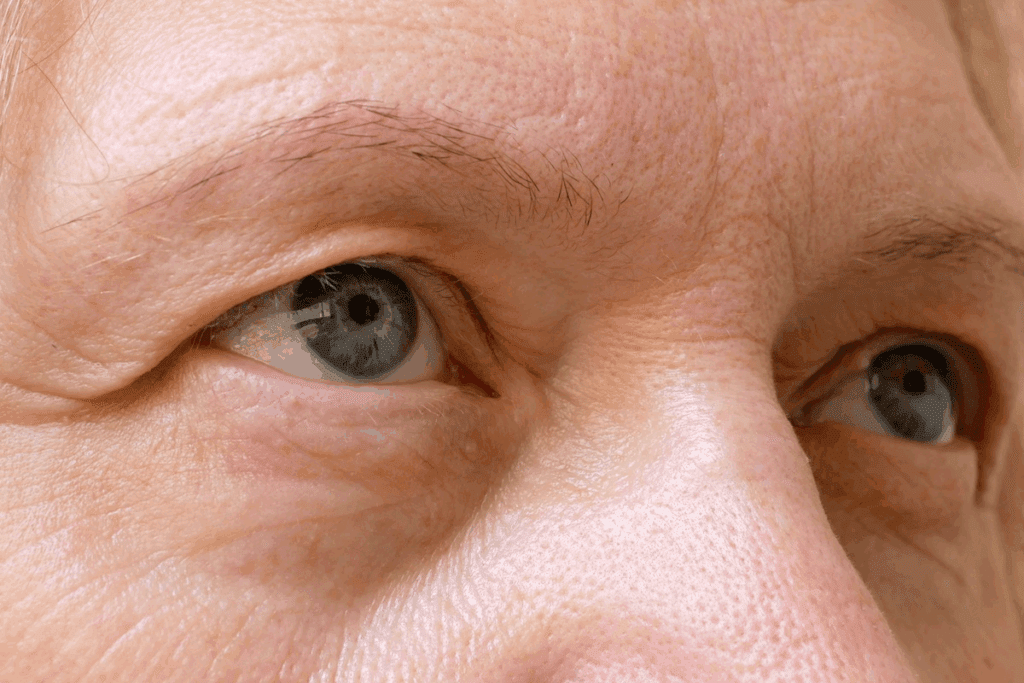
Ever seen your eyes move on their own in jerky or dancing ways? This is called nystagmus. It happens to thousands and can be a simple reaction or a sign of a serious disease. Discover the shocking nystagmus cranial nerve link. Learn how damage to CN VIII (Vestibulocochlear) causes involuntary eye movements.
It’s important to know what causes these involuntary eye movements. At Liv Hospital, we have top experts in brain and eye health. We focus on you to help with this complex issue.
Nystagmus means your eyes move on their own in a rhythmic way. These movements can go side to side, up and down, or even in circles.
Key Takeaways
- Nystagmus is characterized by involuntary, repetitive eye movements.
- These movements can occur in various patterns.
- Understanding nystagmus is key for early detection and treatment.
- Liv Hospital offers top-notch brain and eye health checks.
- We put our patients first in treating nystagmus.
The Nature of Nystagmus: Defining Involuntary Eye Movements

Nystagmus is about involuntary eye movements and their causes. It makes eyes move in a rhythmic way, which can be hard to handle. This condition comes from many neurological and physical reasons, making it hard to diagnose and treat.
The Mechanism Behind Rhythmic Eye Oscillations
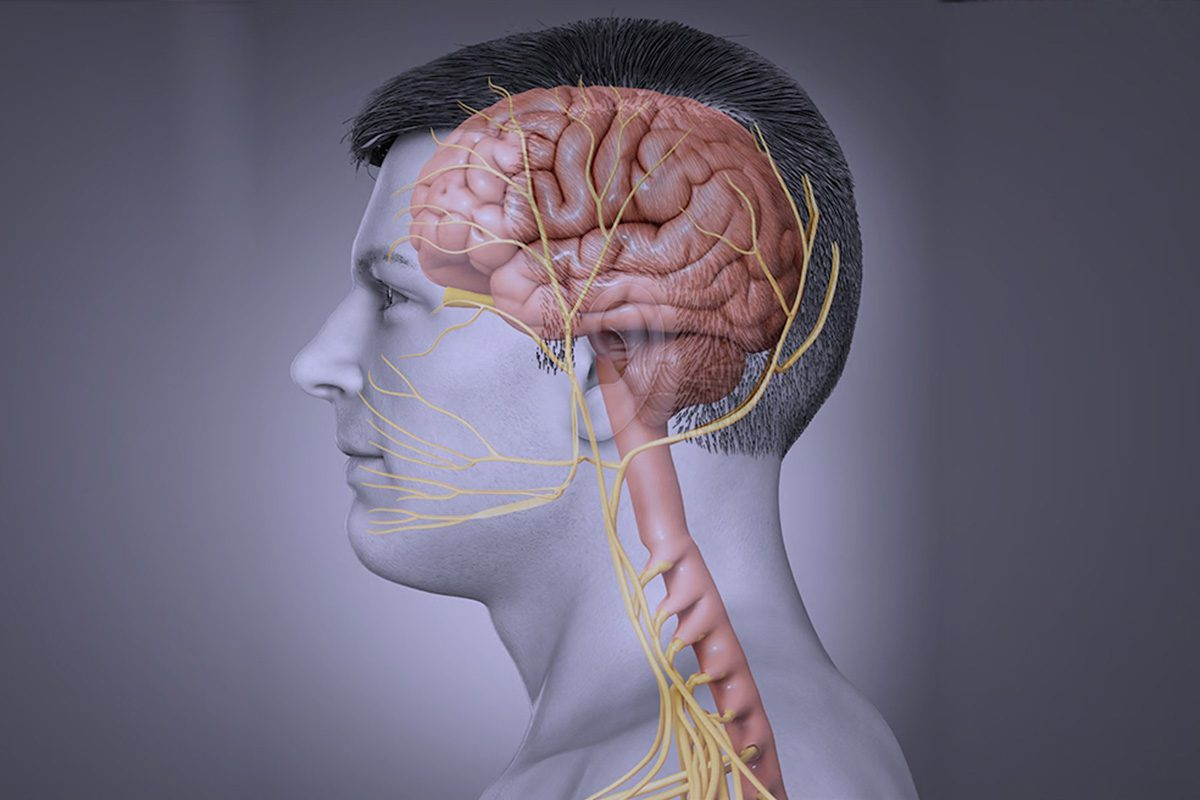
Nystagmus happens when cranial nerves III, IV, and VI don’t work right. These nerves control how our eyes move and stay in place. The vestibulo-ocular reflex is key for keeping our vision steady when we move our head. If this reflex doesn’t work, we get nystagmus.
The vestibulo-ocular reflex is a complex process. It involves the vestibular and oculomotor systems. Any problem in this system can cause the eye movements seen in nystagmus. Issues like vestibular dysfunction, brainstem lesions, or cerebellar disorders can lead to nystagmus.
How Normal Eye Movement Differs from Nystagmus
Normal eye movements are precise and controlled. They help us track objects, read, and move around. Nystagmus, on the other hand, is about involuntary and repetitive eye movements. This can really hurt our vision.
The main difference is in how we control our eye movements. In nystagmus, this control is lost.
Here’s a quick comparison:
- Normal eye movements are voluntary and controlled.
- Nystagmus involves involuntary eye oscillations.
- The vestibulo-ocular reflex is key for stable vision.
Doctors say, “Nystagmus is not just about the eyes. It shows complex neurological and physical processes.” Knowing these differences helps us find better treatments.
“The diagnosis and treatment of nystagmus require a deep understanding of its causes and the complex relationship between the vestibular system, cranial nerves, and the brain.”
— Medical Expert
Types and Patterns of Nystagmus
Nystagmus comes in many forms, each with its own unique traits. Knowing these differences is key for doctors to diagnose and treat nystagmus correctly.
Jerk Nystagmus: Understanding the Fast-Slow Pattern
Jerk nystagmus has a slow drift followed by a quick fix. It’s often linked to problems with the vestibular system. The slow part moves away from the lesion, while the fast part moves towards it.
Key features of jerk nystagmus include:
- A slow phase followed by a quick corrective saccade
- Direction is defined by the fast phase
- Often associated with vestibular or brainstem lesions
Pendular Nystagmus: Symmetrical Oscillations
Pendular nystagmus shows equal movements in both directions, like a wave. It’s often linked to vision or brain issues.
Characteristics of pendular nystagmus include:
- Symmetrical oscillations without a distinct fast or slow phase
- Often seen in patients with visual deprivation or certain neurological disorders
- May be associated with conditions like multiple sclerosis
Directional Classifications: Horizontal, Vertical, and Rotary
Nystagmus can be classified by direction. Horizontal nystagmus is usually due to ear problems. Vertical nystagmus points to brain issues. Rotary nystagmus, with a twist, can come from both ear and brain problems.
The directional classification includes:
- Horizontal nystagmus, often associated with peripheral vestibular dysfunction
- Vertical nystagmus, typically indicating central nervous system pathology
- Rotary or torsional nystagmus, seen in both peripheral and central vestibular disorders
Knowing the different types and patterns of nystagmus is vital for correct diagnosis and treatment. By understanding jerk and pendular nystagmus, and their directions, doctors can find the cause and plan the right treatment.
Nystagmus and Cranial Nerve Function
Nystagmus and cranial nerve function are closely linked. Nystagmus is a condition that affects how our eyes move. It involves the coordination of nerves III, IV, and VI, which control our eye movements.
The Oculomotor System: Cranial Nerves III, IV, and VI
The oculomotor system is key for eye movement. Cranial nerve III (oculomotor nerve) controls four eye muscles. Cranial nerve IV (trochlear nerve) works with the superior oblique muscle. Cranial nerve VI (abducens nerve) controls the lateral rectus muscle. Any problem with these nerves can cause nystagmus.
Vestibular Input: The Role of Cranial Nerve VIII
Cranial nerve VIII, or the vestibulocochlear nerve, sends balance information to the brain. It works with the oculomotor system for eye movement. Problems with this nerve can cause vestibular nystagmus, where eyes move abnormally in response to balance stimuli.
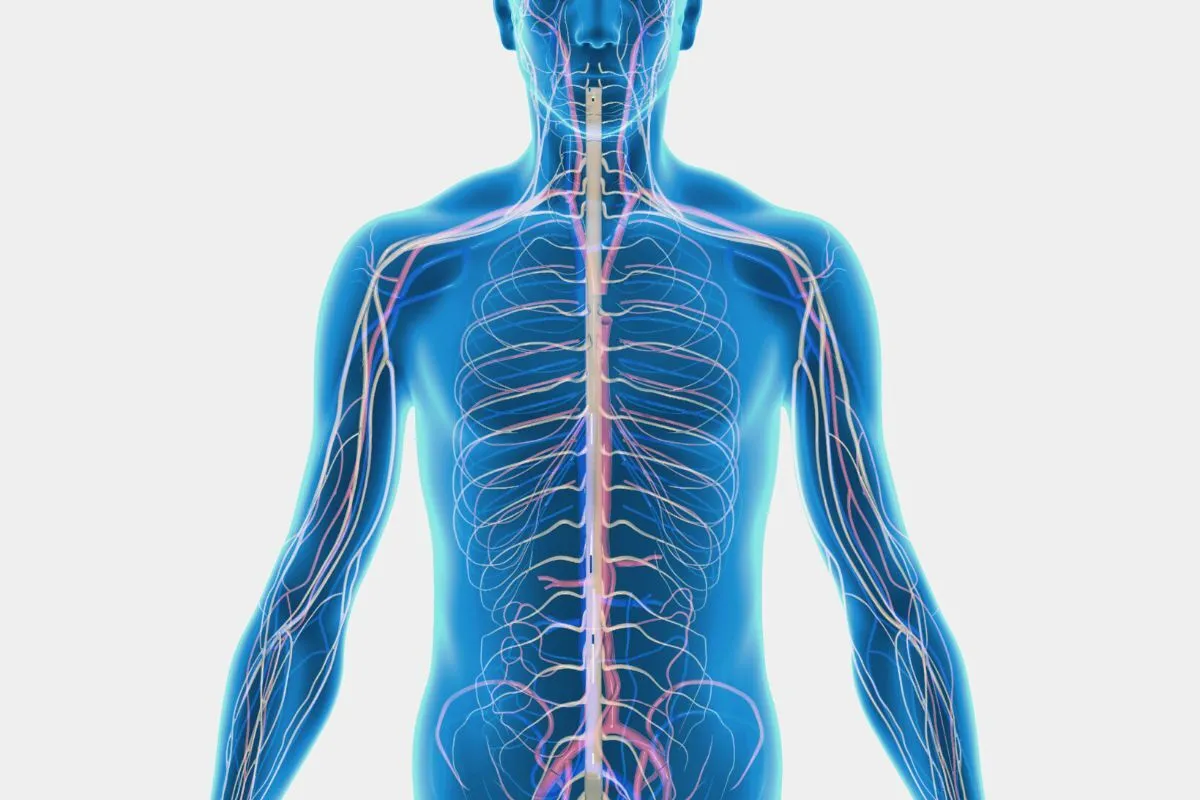
Neural Pathways Controlling Eye Position
Eye position is controlled by a complex network in the brain. The medial longitudinal fasciculus (MLF) is a key pathway. It helps coordinate eye movements. Damage to the MLF can cause internuclear ophthalmoplegia, often linked to nystagmus.
Cranial Nerve | Function | Muscle(s) Innervated |
III (Oculomotor) | Controls several eye movements | Medial rectus, superior rectus, inferior rectus, inferior oblique |
IV (Trochlear) | Controls superior oblique muscle | Superior oblique |
VI (Abducens) | Controls lateral rectus muscle | Lateral rectus |
VIII (Vestibulocochlear) | Transmits vestibular information | N/A |
Peripheral Vestibular Causes of Nystagmus
The peripheral vestibular system is key for balance. Its problems can cause nystagmus. This happens when the inner ear and the vestibular nerve are affected, leading to odd eye movements.
Benign Paroxysmal Positional Vertigo (BPPV)
BPPV is a common cause of nystagmus. It causes brief, intense vertigo when you move your head. This happens when tiny crystals in the inner ear move and bother the vestibular organs.
Key features of BPPV include:
- Vertigo triggered by head movements
- Nystagmus associated with vertigo
- Brief duration of symptoms
Ménière’s Disease and Endolymphatic Hydrops
Ménière’s Disease affects the vestibular system, causing nystagmus. It brings vertigo, tinnitus, hearing loss, and ear fullness. The cause is not clear, but it’s linked to fluid imbalance in the inner ear.
Common symptoms of Ménière’s Disease include:
- Recurring episodes of vertigo
- Tinnitus or ringing in the ears
- Hearing loss, mainly in low frequencies
- A feeling of fullness or pressure in the ear
Vestibular Neuritis and Labyrinthitis
Vestibular neuritis and labyrinthitis are inflammatory issues. Vestibular neuritis inflames the vestibular nerve, causing severe vertigo and nystagmus. Labyrinthitis inflames the inner ear, leading to similar symptoms and hearing loss.
Treatment for these conditions often involves:
- Vestibular rehabilitation therapy
- Medications to alleviate vertigo and nausea
- In some cases, corticosteroids to reduce inflammation
Central Nervous System Origins of Nystagmus
Understanding where nystagmus comes from in the central nervous system is key. It helps us diagnose and treat neurological issues. Conditions like brainstem, cerebellum, or vestibular problems can cause nystagmus. Let’s dive into how these issues lead to nystagmus.
Brainstem Lesions and Their Effects
Lesions in the brainstem can lead to different types of nystagmus. The brainstem is vital for combining sensory inputs to control eye movements. Damage here can disrupt this process, causing nystagmus.
For example, damage to the medial longitudinal fasciculus can cause internuclear ophthalmoplegia. This is often linked to nystagmus.
The type and direction of nystagmus can tell us a lot about the damage. Upbeat nystagmus might point to medulla or midbrain issues. On the other hand, downbeat nystagmus suggests problems at the craniocervical junction.
Cerebellar Dysfunction and Gaze-Evoked Nystagmus
Cerebellar issues are another major cause of nystagmus, like gaze-evoked nystagmus. The cerebellum helps fine-tune eye movements and keep gaze steady. Damage here can make it hard to keep eyes in odd positions, leading to nystagmus.
Gaze-evoked nystagmus happens when trying to look sideways. It’s common in those with cerebellar degeneration or damage to the flocculus or nodulus.
Congenital Brain Abnormalities
Certain brain abnormalities present at birth or early childhood can cause nystagmus. Conditions like albinism, aniridia, or developmental disorders can lead to it. These often affect the visual pathway or oculomotor system.
In summary, nystagmus can stem from various central nervous system issues. Knowing these causes is vital for diagnosing and treating nystagmus and related neurological conditions.
Diseases That Cause Nystagmus
Certain diseases, like multiple sclerosis and Wernicke’s encephalopathy, can cause nystagmus. This happens because they affect the brain’s ability to control eye movements. Nystagmus is a complex condition that can result from various neurological disorders, affecting the quality of life for those affected.
Multiple Sclerosis and Demyelinating Disorders
Multiple sclerosis (MS) is a chronic disease that can cause nystagmus. It happens because of lesions in the brainstem or cerebellum. MS is when the immune system attacks the protective covering of nerve fibers, disrupting communication between the brain and the rest of the body.
The presence of nystagmus in MS patients often indicates a more severe disease course. It can significantly impact their visual function and overall quality of life.
Cerebellar Degeneration Syndromes
Cerebellar degeneration is the progressive deterioration of the cerebellum. It’s responsible for coordinating movements, including eye movements. Various syndromes can lead to cerebellar degeneration, resulting in nystagmus among other symptoms.
These conditions can be hereditary or acquired due to factors such as alcohol abuse or certain medications. The nystagmus associated with cerebellar degeneration is often gaze-evoked, meaning it occurs when the individual looks in certain directions.
Progressive Supranuclear Palsy
Progressive supranuclear palsy (PSP) is a rare neurodegenerative disorder that affects movement, including eye movements. One of the hallmark symptoms of PSP is difficulty moving the eyes, which can lead to a form of nystagmus.
PSP also causes other significant symptoms, including balance problems, speech difficulties, and cognitive decline. The nystagmus in PSP is often accompanied by other ocular motor abnormalities.
Wernicke’s Encephalopathy
Wernicke’s encephalopathy is a serious neurological condition caused by thiamine (vitamin B1) deficiency. It’s often seen in individuals with chronic alcoholism. This condition is characterized by a triad of symptoms: confusion, ophthalmoplegia (weakness or paralysis in the eye muscles), and ataxia (loss of coordination).
Nystagmus is a common finding in Wernicke’s encephalopathy. It results from the damage to the brainstem and other central nervous system structures.
Medications and Substances That Induce Nystagmus
Medications and substances can cause nystagmus, which is when your eyes move on their own. This can happen with many drugs. It’s important for doctors and patients to know how these can affect the eyes and balance.
Anticonvulsants: Phenytoin and Carbamazepine
Phenytoin and carbamazepine can cause nystagmus, mainly at high doses. These drugs help with seizures and sometimes pain or bipolar disorder. They can mess with how the brain controls eye movements.
Sedatives and Tranquilizers
Sedatives and tranquilizers, like diazepam, can also cause nystagmus. They calm the brain but can affect balance and eye control, leading to nystagmus.
Alcohol and Recreational Drug Effects
Alcohol and some recreational drugs can lead to nystagmus. They impact the brain and balance, affecting how the eyes move.
Lithium and Antipsychotic Medications
Lithium and some antipsychotic medications can also cause nystagmus. These drugs can mess with eye movement pathways, including balance and eye control.
Doctors need to watch for nystagmus caused by medications. Finding the cause involves looking at medical history and current drugs and substances.
Metabolic and Systemic Causes of Involuntary Eye Movements
Nystagmus, or involuntary eye movements, can be caused by many factors. These include metabolic and systemic issues that affect the nervous system and how we see. Knowing these causes helps doctors diagnose and treat the problem.
Vitamin B1 Deficiency and Nutritional Factors
Vitamin B1 (Thiamine) deficiency is a big reason for nystagmus. It can cause Wernicke’s encephalopathy, with symptoms like nystagmus, confusion, and ataxia. Lack of vitamins B1 and B12 can also harm the nervous system, causing eye movement problems.
Thyroid Dysfunction and Endocrine Disorders
Thyroid problems can also lead to nystagmus. Both too much and too little thyroid hormone can mess with the nervous system and cause eye issues. Endocrine disorders, like thyroid-associated ophthalmopathy, can also cause nystagmus due to inflammation and swelling around the eye.
Electrolyte Imbalances and Their Ocular Effects
Imbalances in sodium, potassium, and calcium can really affect how we see. These imbalances can mess with the neural control of eye movements, causing nystagmus. Fixing these imbalances is key to managing nystagmus caused by metabolic issues.
Metabolic Cause | Ocular Effect | Associated Condition |
Vitamin B1 Deficiency | Nystagmus, Ophthalmoplegia | Wernicke’s Encephalopathy |
Thyroid Dysfunction | Nystagmus, Exophthalmos | Thyroid-Associated Ophthalmopathy |
Electrolyte Imbalance | Nystagmus, Diplopia | Various Neurological Disorders |
Recognizing Symptoms and Diagnostic Approaches
Spotting the signs of nystagmus is key to getting a correct diagnosis and treatment. Nystagmus shows up in different ways, so a detailed check is needed.
Common Symptoms Associated with Nystagmus
People with nystagmus might see their eyes move on their own, have blurry vision, or feel light sensitivity. These issues can really affect daily life and happiness.
Common symptoms include:
- Involuntary, rhythmic eye movements
- Blurred or distorted vision
- Dizziness or vertigo
- Nausea or vomiting
- Headaches or eye strain
Knowing these symptoms well is important for finding out if someone has nystagmus and what might be causing it.
Neurological Examination Techniques
A detailed check by a neurologist is essential for diagnosing nystagmus. This check looks at eye movements, how the body balances, and the brain’s overall health.
We use different methods in this check, like:
- Looking at how eyes move in different directions
- Testing balance with caloric tests
- Checking the brain and nerves, including those controlling the face and eyes
A top neurologist says, “A detailed check is the main way to find nystagmus. It helps doctors find the cause and plan the best treatment.”
“Finding nystagmus needs a careful approach. It combines a detailed check with special tests to find the cause and plan treatment.”
Advanced Imaging and Laboratory Testing
Along with the neurological check, advanced tests and lab work are also key. These help find any problems that might be causing the nystagmus.
Diagnostic Test | Purpose |
MRI or CT scans | To find any brain problems |
Electronystagmography (ENG) | To record eye movements and check balance |
Blood tests | To look for metabolic or systemic issues |
By using all these tests together, we can accurately diagnose nystagmus. Then, we can make a treatment plan that fits each patient’s needs.
Conclusion: Treatment Options and Living with Nystagmus
Managing nystagmus well starts with finding the root cause. We look at different treatments for nystagmus, making sure they fit each person’s needs.
There are many ways to treat nystagmus. These include medicines, botulinum toxin shots, eye treatments, and surgery. The right treatment depends on the cause and how bad the nystagmus is. For example, drugs can help with symptoms, while surgery fixes problems like eye misalignment.
Dealing with nystagmus can be tough, but with the right care, people can live well. We stress the need for a full care plan. This includes medical help and changes in daily life to boost quality of life.
Knowing what causes nystagmus and looking into treatments helps those with it. They can then find ways to manage their symptoms better.
FAQ
What is nystagmus?
Nystagmus is a condition where your eyes move on their own. It can happen for many reasons, like problems in the brain or eyes.
What are the different types of nystagmus?
There are several types of nystagmus. These include jerk, pendular, and rotary nystagmus. Each type has its own signs and meanings.
What cranial nerves are involved in controlling eye movements?
Eye movements are controlled by cranial nerves III, IV, and VI. Cranial nerve VIII helps keep your balance and where you are in space.
What are the peripheral vestibular causes of nystagmus?
Peripheral vestibular causes include Benign Paroxysmal Positional Vertigo (BPPV) and Ménière’s Disease. These affect the inner ear and balance system.
Can medications cause nystagmus?
Yes, some medicines can cause nystagmus. This includes anticonvulsants, sedatives, and some drugs of abuse.
What are the central nervous system origins of nystagmus?
Nystagmus can come from the brainstem or cerebellum. It can also be caused by brain problems at birth.
What diseases can cause nystagmus?
Many diseases can cause nystagmus. This includes multiple sclerosis and Wernicke’s encephalopathy. It’s important to get a full check-up.
How is nystagmus diagnosed?
Doctors use a detailed check-up and tests to find out why you have nystagmus. They might use imaging and lab tests.
What are the symptoms associated with nystagmus?
Symptoms include eye movements you can’t control and blurred vision. You might also feel dizzy and have trouble balancing.
Can metabolic and systemic conditions cause nystagmus?
Yes, conditions like vitamin deficiencies and thyroid problems can cause nystagmus. It’s important to get checked out thoroughly.
What are the treatment options for nystagmus?
Treatment depends on why you have nystagmus and what you need. It might include medicines, vision therapy, or other help to improve your life.
References
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1279674/