Patients with blood cancers or autoimmune diseases face a tough choice. The idea of a bone marrow transplant can be scary. This procedure, known as stem cell transplantation, replaces damaged bone marrow with healthy stem cells. However, the newest blood therapy for cancer offers additional options beyond traditional transplants, including targeted therapies, immunotherapy, and genetic therapies, providing hope to many patients.
But not everyone can get this treatment. New treatments, such as targeted therapies, immunotherapy, and genetic therapies, are now available. They offer hope to those who need it.
Medical research is transforming the way we treat these diseases. Now, there’s a big push for personalized medicine. These new alternatives give patients more choices and better results.
Key Takeaways
- Advancements in targeted therapies offer new hope for blood cancer patients.
- Immunotherapy is emerging as a viable treatment option for autoimmune diseases.
- Genetic treatments are being explored as a cure for some blood cancers.
- Personalized medicine is becoming key in treatment approaches.
- Patients who can’t get traditional stem cell transplants now have other options.
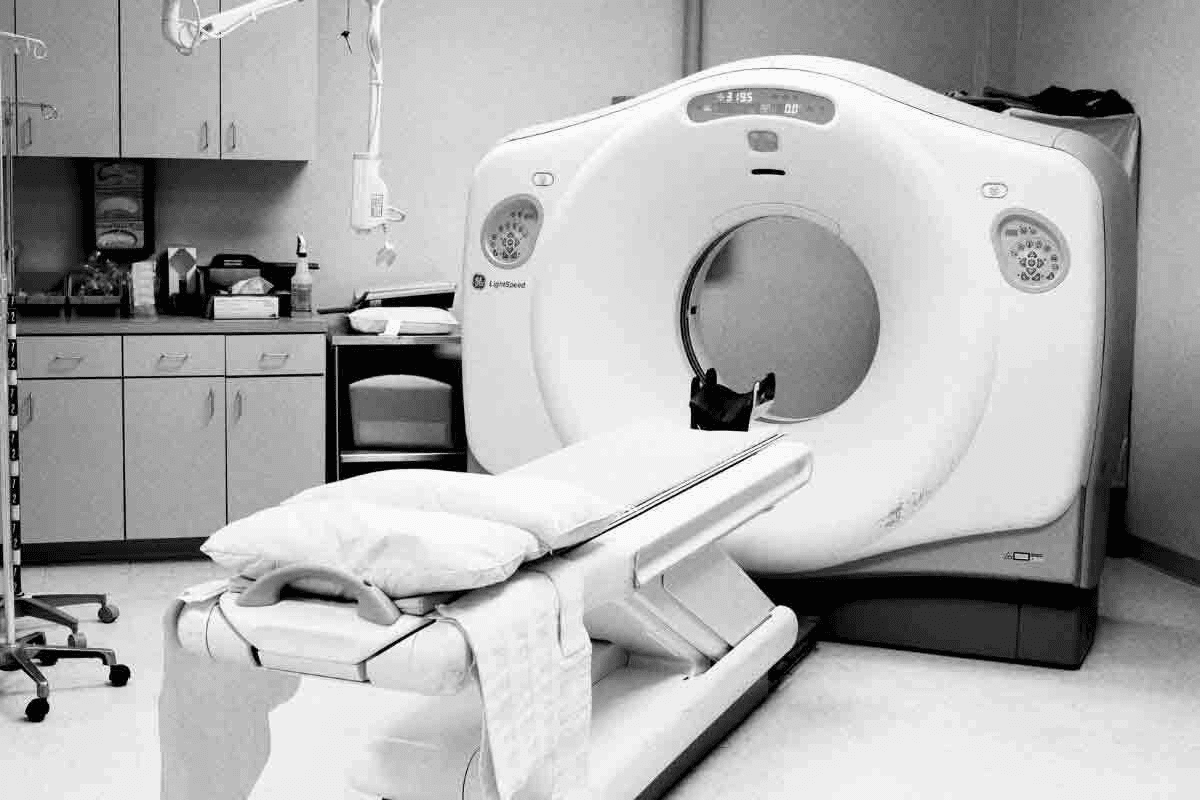
Understanding Stem Cell Transplantation
Stem cell transplantation replaces damaged or diseased cells with healthy ones. It offers hope to those with life-threatening conditions. This procedure is key in treating cancers and blood disorders.
What is a stem cell transplant?
A stem cell transplant replaces a patient’s bad cells with good ones. These cells can turn into different body cells, like blood or bone cells. It’s used after treatments like chemotherapy to fix the bone marrow.
Types of stem cell transplants
There are two main types: autologous and allogeneic. Autologous uses the patient’s own cells. Allogeneic uses cells from a donor. The choice depends on the patient’s health and the cancer type.
Knowing the difference is key for those thinking about a stem cell transplant for cancer. Autologous transplants avoid graft-versus-host disease. Allogeneic transplants might offer a graft-versus-tumor effect, which can help in some cases.
Common conditions treated with stem cell transplants
Stem cell transplants treat leukemia, lymphoma, and more. For those with marrow transplant leukemia, it’s a possible cure. The decision to get a transplant depends on health, disease stage, and treatment response.
When looking at allogeneic transplants, it’s important to know who cannot donate bone marrow. Donors must match the recipient. Some medical conditions or lifestyle choices can make someone ineligible to donate.
Effectiveness and Success Rates of Stem Cell Transplants
Stem cell transplants have changed how we treat blood cancers. They give hope to patients all over the world. The success of these transplants depends on several factors. These include the type of cancer, the patient’s health, and the donor’s match.
Survival Rates for Blood Cancers
Recent studies show promising survival rates for blood cancer patients. For example, a three-year survival rate of 79% for multiple myeloma and 92% for Hodgkin lymphoma has been found. These numbers highlight the effectiveness of stem cell transplants in improving patient outcomes.
When it comes to leukemia BMT, survival rates vary. This depends on the leukemia type and transplant timing. Yet, better transplant techniques and care have led to higher survival rates over time.
Outcomes for Multiple Myeloma and Lymphomas
Stem cell transplants are now a key treatment for multiple myeloma. They often lead to long-term remission and a better quality of life. For certain lymphomas, like Hodgkin lymphoma, transplants can be a cure, even when other treatments fail.
The success of these transplants comes from the new immune system they create. This is key in fighting cancer and aiming for a bone marrow cancer cure.
Long-term Prognosis and Quality of Life
The long-term outlook after a stem cell transplant varies. It depends on the cancer type, the patient’s age, and health. Some patients may be cured, while others need ongoing treatment.
Quality of life after transplant is important. Many patients can live normally again, but some face long-term side effects. Better care and therapies have greatly improved life for those with stem cell transplants for leukemia and other cancers.
In summary, stem cell transplants are a powerful treatment for blood cancers. They offer better survival rates and quality of life. As research advances, we can look forward to even better transplant outcomes and care for patients.
Limitations and Challenges of Stem Cell Transplantation
The process of stem cell transplantation is complex and has many challenges. Finding a suitable bone marrow match is one of them. Managing complications after the transplant is another. This procedure can save lives but has its own set of limitations.
Eligibility Restrictions
Not all patients can get stem cell transplantation. Eligibility criteria are strict. They look at the patient’s health, disease stage, and donor availability. Patients with certain health issues or past treatments might not qualify.
Bone Marrow Compatibility Issues
Finding a bone marrow donor is key to transplant success. Family members have a better chance of being a match. But, even with family, there’s no guarantee. For those without a family donor, finding an unrelated one can be long and uncertain.
Graft-Versus-Host Disease and Other Complications
Graft-versus-host disease (GVHD) is a big risk of stem cell transplant. It happens when the donor’s immune cells attack the recipient’s body. GVHD can be mild or severe. Other risks include infections, organ damage, and graft failure.
Recovery Timeline and Challenges
Recovering from a stem cell transplant is long and hard. Patients often stay in the hospital for weeks. They may need months or years to fully recover. The recovery timeline depends on the transplant type, patient health, and any complications.
In summary, stem cell transplantation is a valuable option for many. But it’s important to know its limitations and challenges. Understanding these can help patients and their families make better decisions about their care.
When Patients Need Alternatives to Transplantation
Stem cell transplantation isn’t right for everyone, like those with certain health issues or diseases that don’t respond to treatment. It’s a good option for many blood cancers and disorders. But some patients need to look at other choices.
Who cannot undergo a bone marrow transplant??
Some people can’t get bone marrow transplants because of their age, health, or medical conditions. Older adults or those with serious health problems might face too many risks. So, they need other treatments.
- Patients with severe organ dysfunction
- Those with active infections or certain types of cancer
- Individuals with a history of previous treatments that may impact transplant success
Treatment-resistant conditions
For those with conditions that don’t respond to treatment, stem cell transplants might not work. In these cases, doctors look for other treatments that match the patient’s condition. Treatment-resistant conditions often need new and personalized ways to treat them.
For example, people with blood cancers that keep coming back might try targeted or immunotherapies. These options can give them hope for better disease management or even remission.
Patient preference considerations
What patients want to do is very important in choosing treatments. Some might not want to risk the side effects of stem cell transplants, like GVHD or needing to take strong medicines for a long time. So, they look for treatments with fewer risks.
Talking to doctors about all the options is key. Patient-centered care means looking at what each person needs, wants, and values.
Understanding the limits of stem cell transplants helps doctors and patients find the best alternatives together. This team effort makes sure patients get care that fits their unique situation.
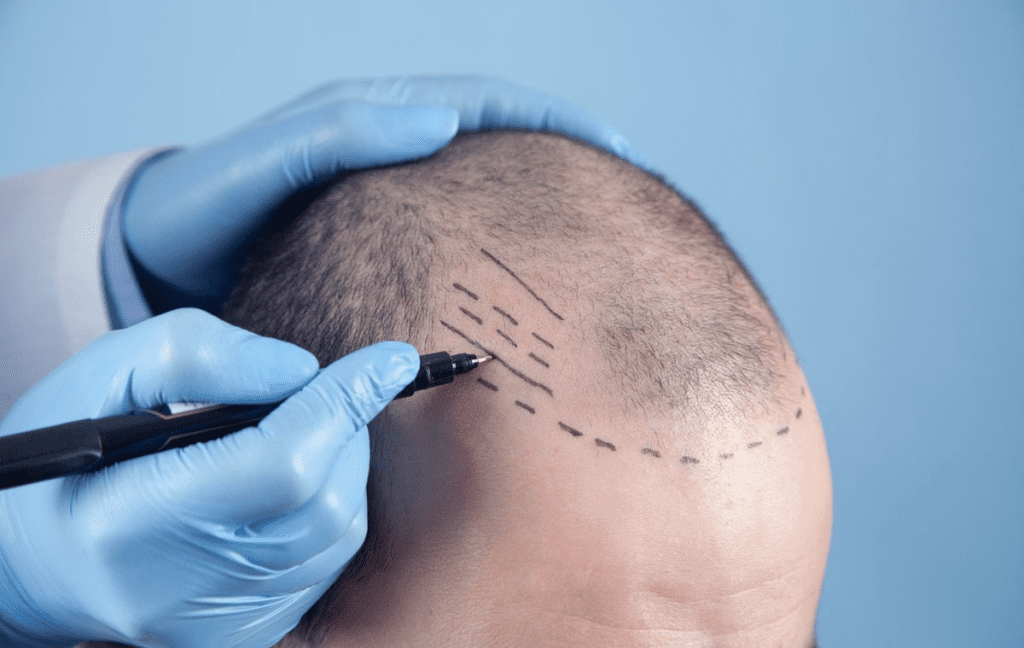
Targeted Therapies for Blood Cancers
Targeted therapies have changed how we treat blood cancers. They offer a new option instead of stem cell transplants. These therapies focus on cancer cells, harming fewer healthy cells.
How Targeted Therapies Work
Targeted therapies target specific cancer cell traits, like proteins or genes. They aim to stop cancer cells from growing and surviving.
Key benefits of targeted therapies include:
- Reduced damage to healthy cells
- Fewer side effects compared to traditional chemotherapy
- Potential for more effective treatment for specific types of blood cancers
Leukemia-Specific Targeted Treatments
Targeted therapies have shown great promise in leukemia treatment. Tyrosine kinase inhibitors (TKIs) are key in treating Chronic Myeloid Leukemia (CML) and some Acute Lymphoblastic Leukemia (ALL).
Examples of leukemia-specific targeted treatments include:
- Imatinib (Gleevec) for CML
- Rituximab for certain types of ALL and CLL
Effectiveness Compared to Bone Marrow Transplant for Leukemia
Targeted therapies and bone marrow transplants have different benefits and risks. Bone marrow transplants can cure but come with big risks like graft-versus-host disease (GVHD).
Targeted therapies offer effective control with fewer side effects. For some patients, they can match or beat bone marrow transplant results.
Case Studies and Success Stories
Many case studies show targeted therapies’ success in leukemia. Patients with CML treated with TKIs often live long with few side effects.
One patient with CML avoided a bone marrow transplant thanks to imatinib. They achieved a deep molecular response.
Immunotherapy as an Alternative to Stem Cell Transplants Alternative
Immunotherapy has made big strides, giving hope to those needing stem cell transplant alternatives. It uses the immune system to battle cancer. This method is less invasive and targets cancer more precisely than traditional transplants.
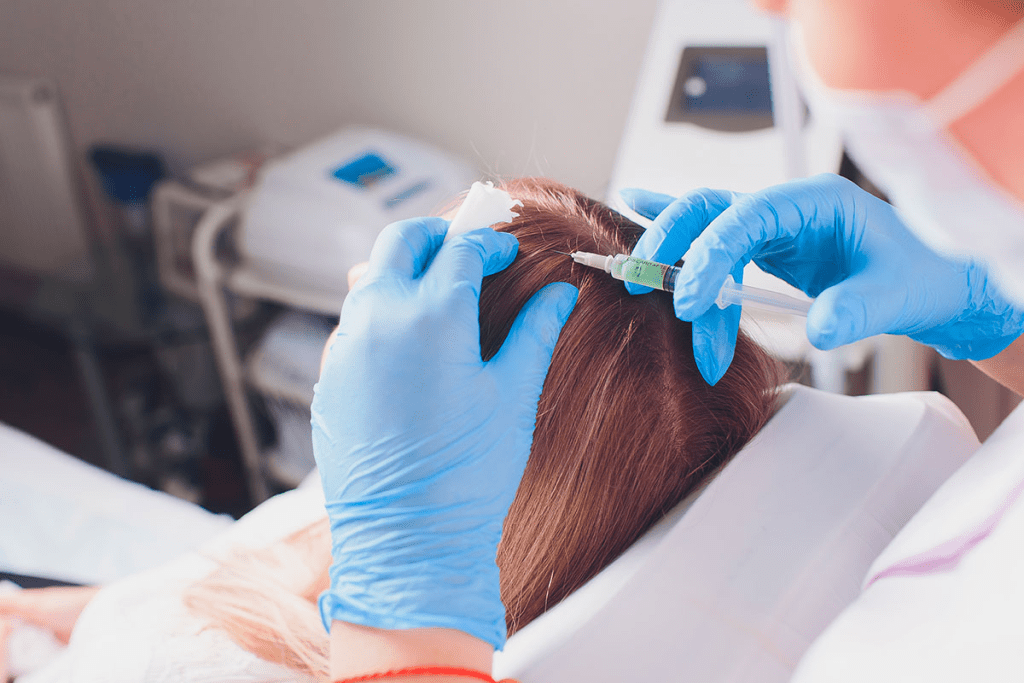
CAR-T Cell Therapy
CAR-T cell therapy is a new immunotherapy method. It takes a patient’s T cells, changes them to attack cancer, and then puts them back in the body. This therapy has shown significant remission rates in patients with relapsed lymphoma, helping those who’ve tried other treatments.
The steps of CAR-T cell therapy are:
- T cell extraction: T cells are taken from the patient’s blood.
- Modification: T cells are made to produce CARs that target cancer cells.
- Expansion: The modified T cells are grown in a lab.
- Reinfusion: The CAR-T cells are given back to the patient.
Monoclonal Antibodies
Monoclonal antibodies are a promising immunotherapy for cancer treatment. These antibodies are made in labs to target specific proteins on cancer cells. They mark these cells for destruction by the immune system. They can be used alone or with other treatments to boost their effect.
Monoclonal antibodies offer several benefits:
- They target cancer cells, protecting healthy cells.
- They can carry drugs or radioactive isotopes to cancer cells.
- They activate the immune system to fight cancer.
Checkpoint Inhibitors
Checkpoint inhibitors are immunotherapy drugs that let the immune system fight cancer better. They target proteins on immune cells that control the immune response. This helps the immune system attack cancer more effectively.
Checkpoint inhibitors have helped treat many cancers, like melanoma, lung cancer, and bladder cancer. They work by:
- Blocking proteins that slow down the immune response.
- Boosting the immune system’s attack on cancer cells.
- Offering long-lasting benefits for some patients.
In summary, immunotherapy, including CAR-T cell therapy, monoclonal antibodies, and checkpoint inhibitors, is a big step forward in cancer treatment. It offers a good alternative to stem cell transplants for many patients.
Advanced Drug Regimens for Hematological Cancers
The treatment of hematological cancers is changing fast. New drug regimens are key to this change. Thanks to new medicines, we’re seeing big improvements in how these cancers are treated.
Novel Pharmaceutical Approaches
New medicines are being made to target specific traits of hematological cancers. Immunomodulatory drugs are showing great promise in treating multiple myeloma and other cancers. They boost the immune system’s fight against cancer cells.
Lenalidomide and Pomalidomide are examples of these drugs. They have greatly helped patients with multiple myeloma. They are often used with other treatments to make them work better.
Immunomodulators for Multiple Myeloma
Immunomodulators are now a key part of treating multiple myeloma. These drugs not only help patients respond better but also live longer. Immunomodulators are changing how we treat multiple myeloma.
- Improved response rates
- Enhanced overall survival
- Better tolerability profiles
Combination Therapy Strategies
Combining different drugs is becoming more common in treating hematological cancers. This approach helps target cancer cells better and lowers the chance of resistance.
For instance, mixing immunomodulators with proteasome inhibitors has been very effective in treating multiple myeloma. This method attacks cancer cells from all sides.
Personalized Medicine Approaches
Personalized medicine is changing how we treat hematological cancers. Tailoring treatments to each patient’s cancer improves results and cuts down on side effects.
Genetic tests and other tools help find the best treatments for each patient. This approach is the future of treating hematological cancers.
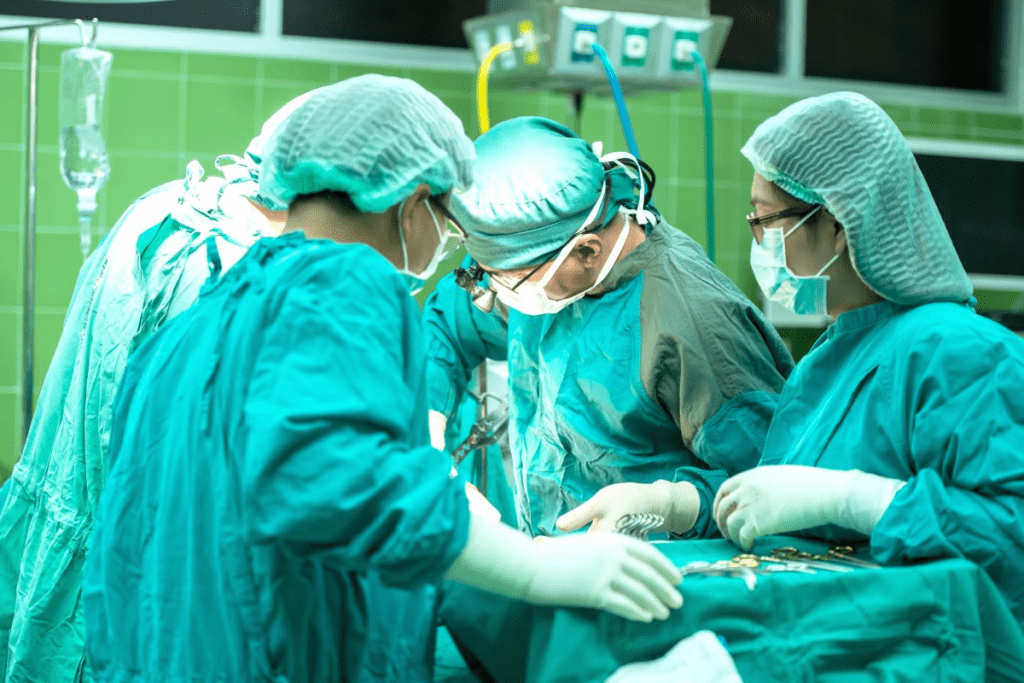
Genetic Therapies and CRISPR Technology
Genetic therapies and CRISPR technology are changing how we treat genetic blood disorders. They offer new hope to patients who had few options before.
Gene Editing for Sickle Cell Disease and Beta-Thalassemia
CRISPR-Cas9 gene editing is showing great promise in treating sickle cell disease and beta-thalassemia. These diseases are caused by specific gene mutations. Clinical trials have shown it’s safe and effective, leading to big improvements in patients.
Gene editing takes a patient’s stem cells, fixes the faulty gene with CRISPR, and puts them back. This could lead to a functional cure for these diseases.
Current Clinical Trials and Research
Many clinical trials are looking into CRISPR-Cas9 for genetic blood disorders. These trials are key to understanding its long-term effects. Researchers are also looking into using CRISPR for other genetic conditions, expanding its use.
- Trials are checking if CRISPR can fix genetic mutations.
- They’re watching patients for long-term effects and side effects.
- Studies are looking into making CRISPR technology more accessible.
Future of Stem Cell Replacement
The future of genetic therapies, like CRISPR, looks bright for stem cell replacement. As research grows, gene editing will become a better option for genetic blood disorders. CRISPR could cure diseases that were thought to be incurable, and research is finding new ways to use it.
We’re dedicated to keeping up with research and development. We want to make sure patients have access to the best treatments.
Comparing Stem Cell Transplant Alternatives: Efficacy and Risks
When looking at alternatives to stem cell transplants, it’s key to check their effectiveness and risks. Different treatments have come up as possible substitutes, each with its own good and bad points.
Survival Rates Comparison
Survival rates are a big deal when we talk about how well treatments work. Research shows that some treatments, like targeted therapies and immunotherapies, can match or beat stem cell transplants in some cases.
- Targeted Therapies: Show great promise in fighting certain blood cancers, with some studies showing better survival rates than traditional transplants.
- Immunotherapies like CAR-T cell therapy have shown amazing results in some blood cancers, but they come with risks.
- Advanced Drug Regimens: New drug combinations and approaches have led to better results for patients with multiple myeloma and other blood cancers.
Side Effect Profiles
The side effects of stem cell transplant alternatives differ a lot. Some treatments might be less harsh, but others can bring new risks.
For example, targeted therapies might have fewer side effects than old-school chemotherapy, but they can cause big problems too. Immunotherapies, on the other hand, can lead to serious immune reactions.
Quality of Life Considerations
When we look at stem cell transplant alternatives, we must think about how they affect our daily lives. Treatments that might save lives but make everyday tasks hard might not be the best choice for everyone.
We should think about the long-term effects of these treatments, like:
- The need for ongoing treatment and checks
- Possible long-term side effects
- How they affect our physical and mental health
Cost and Accessibility Factors
The cost and how easy it is to get stem cell transplant alternatives are big factors in choosing a treatment. Newer treatments might offer better results, but they can be very expensive.
We need to think about:
- How insurance covers these treatments
- If these treatments are available in different places
- Support services for those going through these treatments
By carefully looking at these points, patients and doctors can make smart choices about the best treatments.
Treatment Approaches for Autoimmune Diseases
Autoimmune diseases are a big challenge in medicine today. We need new ways to treat them, not just stem cell therapy. As we learn more, we’re finding new ways to help patients feel better and live better lives.
Alternatives to Stem Cell Therapy for Autoimmune Conditions
For those who can’t or don’t want stem cell therapy, there are other options. Biologics are a big step forward. They target the immune system to reduce inflammation and slow disease.
Studies show biologics work well for diseases like rheumatoid arthritis and lupus. For example, a study on the National Center for Biotechnology Information website shows their success.
Biologics and Targeted Immunosuppression
Biologics focus on specific parts of the inflammatory process. This reduces the immune system’s attack on the body. Targeted immunosuppression is also important. It helps control the immune response better, with fewer side effects.
- Monoclonal antibodies that target specific immune cells or cytokines
- Small molecule inhibitors that block key pathways in the inflammatory process
- Immunomodulators that adjust the immune response to reduce disease activity
Novel Treatment Protocols
New treatment plans are always being developed. This is because we’re learning more about autoimmune diseases and the immune system. Researchers are looking into new ways, like combining different treatments for better results.
“The future of autoimmune disease treatment lies in personalized medicine, where therapies are tailored to the individual patient’s needs and disease profile.” – Autoimmune Disease Specialist
Comparative Effectiveness Research
As new treatments come along, it’s important to study how they compare. This helps doctors and patients make the best choices. It’s about finding the right balance between how well a treatment works, its safety, and how it affects quality of life.
By keeping up with new research and treatments, we can make life better for people with autoimmune diseases.
Conclusion: The Future of Alternatives to Stem Cell Transplantation
The future of cancer treatment is looking bright. New therapies like targeted treatments, immunotherapy, and genetic fixes are on the horizon. These options offer hope for those who can’t have traditional stem cell transplants.
Therapies like CAR-T cell therapy and gene editing are showing great promise. They’re not just improving survival rates but also making life better for patients. This shift towards personalized care is a big step forward.
Research and clinical trials are driving these advancements. We can expect even better treatments for blood cancers and other diseases. This will lead to better care and outcomes for patients.
FAQ
What is a stem cell transplant?
A stem cell transplant replaces damaged or diseased stem cells with healthy ones. It helps treat blood cancers and autoimmune diseases.
Who is eligible for a stem cell transplant?
Eligibility for a stem cell transplant depends on several factors. These include the type and stage of the disease, overall health, and the availability of a compatible donor.
What are the alternatives to stem cell transplantation?
Alternatives include targeted therapies, immunotherapy, advanced drug regimens, and genetic therapies. These can treat blood cancers and autoimmune diseases.
How do targeted therapies work?
Targeted therapies identify and attack specific cancer cells or proteins. This reduces harm to healthy cells and minimizes side effects.
What is CAR-T cell therapy?
CAR-T cell therapy removes T cells from the blood. It modifies them to recognize cancer cells and then reinfuses them to attack the cancer.
Can stem cell transplants cure leukemia?
Stem cell transplants can be an effective treatment for leukemia. They offer a cure for some patients, mainly those with certain types of leukemia.
What are the risks associated with stem cell transplants?
Risks include graft-versus-host disease, infection, and organ damage. These are among the complications of stem cell transplants.
How do I know if I’m a match for a bone marrow transplant?
A compatibility test is performed to check if you’re a match. It looks at the human leukocyte antigen (HLA) typing between the donor and recipient.
What is the difference between autologous and allogeneic stem cell transplants?
Autologous stem cell transplants use the patient’s own stem cells. Allogeneic stem cell transplants use stem cells from a donor.
Can genetic therapies replace stem cell transplants?
Genetic therapies, like CRISPR technology, may treat genetic blood disorders. They could potentially replace stem cell transplants in the future.
What are the benefits of immunotherapy compared to stem cell transplants?
Immunotherapy offers benefits like reduced risk of graft-versus-host disease. It may also have fewer side effects than stem cell transplants.
Are there alternative treatments for autoimmune diseases?
Yes, treatments include biologics, targeted immunosuppression, and novel protocols. These can manage symptoms and improve quality of life.
How do advanced drug regimens work for hematological cancers?
Advanced drug regimens for hematological cancers use novel pharmaceutical approaches. They include immunomodulators and combination therapy strategies to target cancer cells and improve outcomes.
References
- Jung, S. M., et al. (2022). Targeted immunotherapy for autoimmune diseases. Nature Communications, 13, 834. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8901705
- Dana-Farber Cancer Institute. (2024). How immunotherapy can treat cancer and autoimmune diseases. https://www.yalemedicine.org/news/how-immunotherapy-can-treat-cancer-and-autoimmune