Chronic pelvic pain affects millions of women worldwide. It greatly impacts their quality of life and productivity. We know that 1 in 7 women in the US deal with persistent pelvic pain for over six months. Yet, it’s often overlooked and underdiagnosed in gynecology.
Despite its big impact, women’s health suffers because of unclear diagnosis and treatment plans. We see the need to tackle pelvic pain syndrome fully to help those affected.
We use proven strategies to manage chronic pelvic pain. In this article, we’ll look at five key methods. These have shown promise in helping women manage their symptoms and take back control of their health.
Five proven strategies for managing chronic pelvic pain symptoms and improving a patient’s quality of life.
Key Takeaways
- Understanding the prevalence and impact of chronic pelvic pain in women.
- The importance of a complete approach to managing pelvic pain syndrome.
- Evidence-based strategies for effective chronic pelvic pain management.
- Improving quality of life through targeted interventions.
- Enhancing productivity and overall well-being for women affected by chronic pelvic pain.
Understanding Chronic Pelvic Pain: Definition and Prevalence

Chronic pelvic pain is a serious issue that affects many women. It makes daily life hard and impacts their overall health. It’s a condition that’s both common and debilitating.
What Defines Chronic Pelvic Pain Syndrome
Chronic pelvic pain syndrome lasts more than 6 months. It can feel like sharp, dull, or constant pain. This pain often stays in the pelvic area but can spread to other parts of the body.
A study in a top medical journal says, “Chronic pelvic pain is a complex condition that needs a detailed approach for diagnosis and treatment.”
“The diagnosis of chronic pelvic pain involves a thorough medical history, physical examination, and sometimes, additional diagnostic tests to rule out other conditions.”
Statistical Overview of Women Affected Globally
Many women suffer from chronic pelvic pain. It’s found in 5.7% to 26.6% of women worldwide. The exact number varies based on who’s studied and how pain is defined.
Region | Prevalence Rate |
North America | 14.2% |
Europe | 12.1% |
Asia | 8.5% |
These numbers show we need to know more about chronic pelvic pain. By understanding it, we can help women live better lives. Awareness and effective treatments are key.
The Impact of Chronic Pelvic Pain on Women’s Quality of Life

Chronic pelvic pain can greatly lower a woman’s quality of life. It affects her physical health and her mental state. It also impacts her financial stability.
Physical Limitations and Daily Functioning
Chronic pelvic pain makes everyday tasks hard. Women may struggle with standing, sitting, or doing physical activities. Even simple tasks like grocery shopping or cooking can be tough, affecting their independence.
The pain can also mess with sleep, causing fatigue. This makes the pain worse, creating a cycle. It greatly reduces daily functioning and quality of life.
Psychological and Emotional Effects
The mental effects of chronic pelvic pain are significant. Women often feel anxiety, depression, and isolation. The pain can make them lose their identity and self-esteem.
It can also hurt relationships with family and friends. This makes them feel lonelier and more desperate. It’s important to treat these mental effects as part of the treatment.
Economic Burden and Healthcare Costs
The financial cost of chronic pelvic pain is high. In the U.S., it costs $881.5 million a year for outpatient care. Lost productivity and reduced quality of life add to the financial burden.
It’s key to understand how chronic pelvic pain affects women’s lives. By tackling the physical, mental, and financial sides, healthcare can offer better care. This can improve the lives of women with chronic pelvic pain.
Common Causes and Risk Factors of Chronic Pelvic Pain
It’s important to know what causes chronic pelvic pain to manage it well. This pain can show up in different ways, like during periods, during sex, or at other times. Finding out what causes it and who is at risk is key.
Gynecological Conditions
Gynecological issues are a big reason for chronic pelvic pain in women. Endometriosis is a common cause, where tissue grows outside the uterus. Other issues include adenomyosis and pelvic adhesions, which can also cause pain.
Non-Gynecological Contributors
Other conditions can also lead to chronic pelvic pain. Irritable Bowel Syndrome (IBS) is one, causing pain and changes in bowel habits. Interstitial cystitis is another, leading to bladder pain and sometimes pelvic pain.
Psychosocial Factors
Psychological and social factors can also affect chronic pelvic pain. Stress and anxiety can make pain worse. A history of trauma or abuse can also play a role, showing the need for a complete treatment plan.
Diagnosing Chronic Pelvic Pain: The Path to Proper Management
To manage chronic pelvic pain well, we need to find the right diagnosis. Finding the cause of chronic pelvic pain starts with a detailed check-up and a thorough look at the patient’s medical history.
Initial Assessment and Medical History
The first step is to take a detailed medical history. We ask about the patient’s symptoms, menstrual cycle, sexual history, and any surgeries or treatments they’ve had. This helps us find possible causes and guides our next steps.
We also ask about the patient’s family history, lifestyle, and any past diagnoses or treatments for pelvic pain. Knowing the patient’s overall health helps us understand their pain better.
Physical Examination Techniques
A physical exam is key in diagnosing chronic pelvic pain. We do a pelvic exam to check the reproductive organs for any issues like tenderness or adhesions. This exam may include a speculum exam or a bimanual exam to check the pelvic floor muscles and find pain spots.
During the exam, we also look for signs of other possible causes of pelvic pain, like muscle or nerve problems. This detailed check helps us make a more accurate diagnosis and decide on further tests or treatments.
Diagnostic Testing and Imaging
Diagnostic tests and imaging are important to find the cause of chronic pelvic pain. We might use ultrasound, MRI, or laparoscopy to see the pelvic organs and find any problems, like endometriosis or fibroids.
We also do blood work or urinalysis to check for infections or other conditions. By combining these test results with the patient’s medical history and physical exam, we can make a precise diagnosis and plan the best treatment.
Strategy 1: Comprehensive Medical Treatment Approaches
Women with chronic pelvic pain need a detailed medical plan. This plan combines treatments that fit each person’s specific needs.
First, a thorough check-up is done to find the pain’s cause. Medical treatment plans are then made to tackle these causes head-on.
Pharmacological Interventions
Pharmacological interventions are key in managing chronic pelvic pain. They include pain relievers, anti-inflammatory drugs, and more. These aim to lessen pain and discomfort.
For mild to moderate pain, over-the-counter drugs like ibuprofen work well. But for severe pain, doctors might prescribe stronger meds.
Hormonal Therapies
Hormonal therapies are vital for conditions like endometriosis. Hormonal changes can make symptoms worse. Treatments like birth control pills or GnRH agonists help balance hormones.
These therapies can greatly reduce pain by stabilizing hormone levels.
Surgical Options When Necessary
In some cases, surgical options are needed to fix chronic pelvic pain’s causes. For example, surgery might remove endometriotic lesions or repair prolapse. It’s for anatomical issues too.
Doctors consider surgery after trying other treatments. They weigh the benefits and risks carefully.
By using a variety of medical treatments, doctors can create a plan that meets each patient’s needs. This improves pain management chances.
Strategy 2: Physical Therapy and Rehabilitation for Chronic Pelvic Pain
Managing chronic pelvic pain often needs a detailed physical therapy plan. We see how important physical therapy is. It offers many ways to lessen pain and boost function.
Pelvic Floor Physical Therapy Techniques
Pelvic floor physical therapy targets the muscles and tissues around the pelvic area. Techniques include manual therapy, biofeedback, and electrical stimulation. These methods aim to cut down pain and better pelvic floor function.
This therapy tackles muscle tightness and weakness. It can greatly lessen chronic pelvic pain. We’ve seen it improve pelvic health and ease symptoms.
Exercise Programs and Movement Therapies
Custom exercise plans are key in managing chronic pelvic pain. Gentle exercises like yoga and Pilates can boost flexibility and strength. They also help avoid putting too much pressure on the pelvic area.
Movement therapies, like aerobic exercises, are also good. They help with blood flow, muscle relaxation, and overall health. It’s wise to talk to a healthcare expert for a tailored exercise plan.
Manual Therapy and Massage Approaches
Manual therapy, including different massage methods, is a great way to handle chronic pelvic pain. Massage therapy can ease muscle spasms, enhance blood flow, and relax the body.
Adding manual therapy and massage to a treatment plan can lessen pain and enhance life quality. It’s vital to work with a skilled therapist for the best outcomes.
Strategy 3: Pain Management Techniques and Interventions
Pain management is key for women with chronic pelvic pain. It helps them live better lives, doing daily tasks without pain.
Nerve Blocks and Injections
Nerve blocks and injections are used to manage chronic pelvic pain. They involve injecting a local anesthetic or steroid into nerves or areas around the pelvis to lessen pain.
Benefits of Nerve Blocks:
- Provides immediate pain relief
- Can be used diagnostically to identify pain sources
- Minimally invasive
Transcutaneous Electrical Nerve Stimulation (TENS)
TENS is a non-invasive method that uses electrical currents to ease pain. It blocks or interrupts pain signals to the brain.
TENS Therapy Benefits:
- Non-pharmacological pain relief
- Portable and easy to use
- Can be adjusted according to individual needs
Advanced Pain Management Procedures
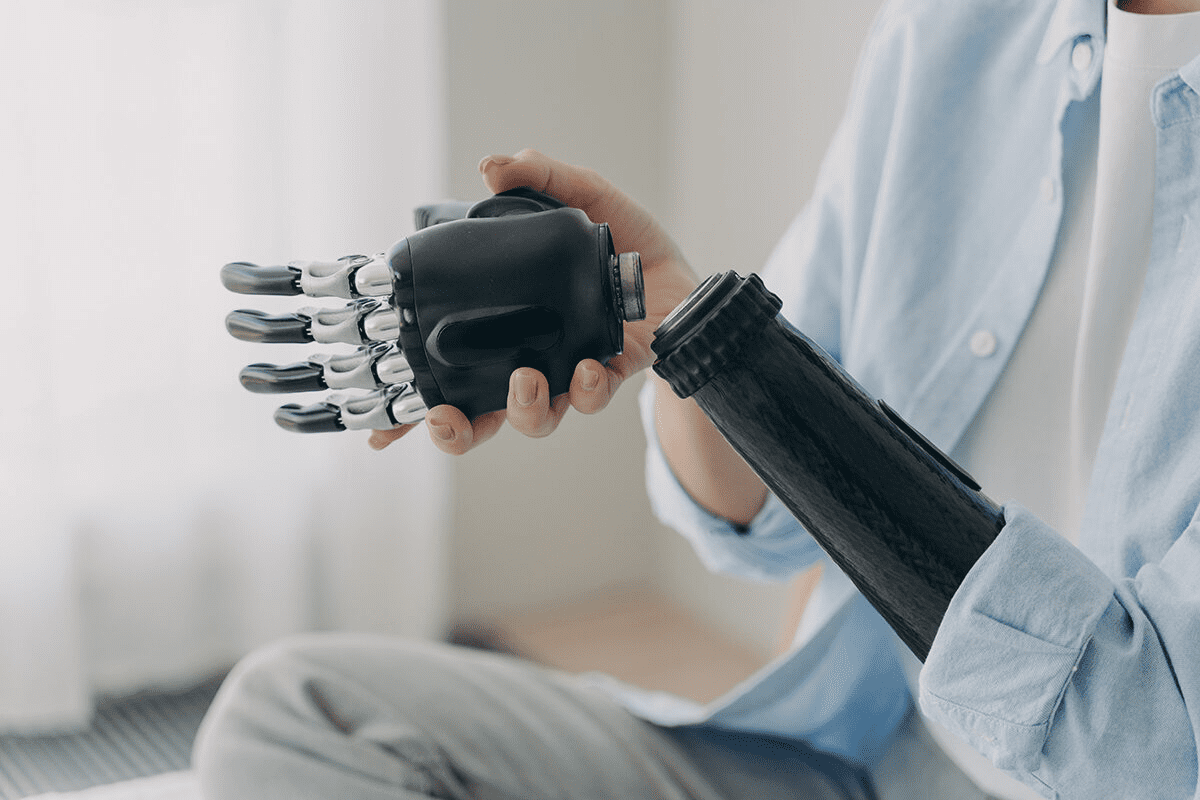
For some, advanced procedures are needed to manage chronic pelvic pain. These include spinal cord stimulation, intrathecal drug delivery systems, and other interventional techniques.
Procedure | Description | Benefits |
Spinal Cord Stimulation | Involves implanting a device that sends electrical impulses to the spinal cord | Significant pain reduction, improved quality of life |
Intrathecal Drug Delivery | Delivers medication directly into the spinal fluid | Targeted pain relief, reduced systemic side effects |
Healthcare providers can create a detailed treatment plan for women with chronic pelvic pain. This plan includes various pain management techniques and interventions.
Strategy 4: Integrative and Complementary Approaches
Integrative and complementary therapies offer a holistic way to tackle chronic pelvic pain. They can add benefits when paired with traditional treatments. This helps improve overall well-being and pain control.
Acupuncture and Traditional Chinese Medicine
Acupuncture, a part of Traditional Chinese Medicine, is gaining attention for managing chronic pelvic pain. It works by stimulating certain body points. This can lessen pain and enhance life quality.
“Acupuncture has been shown to decrease pain intensity and improve quality of life in women with chronic pelvic pain.”
A study in the Journal of Pain Research showed acupuncture cuts pain in chronic pelvic pain syndrome. The exact how is unclear, but it’s thought to involve neurotransmitters and pain perception changes.
Mindfulness and Meditation Practices
Mindfulness and meditation are recognized for pain management. They help people better understand their body and emotions. This makes coping with pain easier.
- Mindfulness-Based Stress Reduction (MBSR) programs have been shown to reduce chronic pain symptoms.
- Meditation can decrease the emotional reactivity to pain, improving overall well-being.
Studies suggest regular mindfulness can alter brain areas linked to pain. This supports its use as a complementary therapy for chronic pelvic pain.
Dietary Modifications and Nutritional Support
Diet is key in managing chronic pelvic pain. Some foods can make symptoms worse or better. Making dietary changes is vital for a full treatment plan.
Dietary Approach | Potential Benefits |
Anti-inflammatory diet | Reduces inflammation, potentially decreasing pain |
Nutritional supplements (e.g., omega-3 fatty acids) | Supports overall health and may reduce pain symptoms |
By adding integrative and complementary methods to their treatment, women with chronic pelvic pain can see better pain management. This can also improve their quality of life.
Strategy 5: Psychological Support and Behavioral Interventions
The fifth strategy for managing chronic pelvic pain is to offer strong psychological support and teach effective behaviors. This approach sees chronic pelvic pain as more than just physical. It also involves psychological and emotional aspects.
Cognitive Behavioral Therapy for Pain Management
Cognitive Behavioral Therapy (CBT) is a key tool for managing chronic pelvic pain. It helps women change negative thoughts and behaviors that make their pain worse. By learning new strategies, women can live better lives.
Studies show CBT can lessen pain and improve function in women with chronic pelvic pain. A Journal of Pain Research study found CBT reduced pain and improved mood in participants. This was more than standard care.
“Cognitive-behavioral therapy is effective in reducing chronic pain and improving mood in women with chronic pelvic pain.”
Stress Reduction Techniques
Stress can make chronic pelvic pain worse. So, reducing stress is key to managing pain. Mindfulness meditation, deep breathing, and muscle relaxation can help.
A study on mindfulness-based stress reduction (MBSR) for chronic pelvic pain showed big improvements. MBSR helps by focusing on the present without judgment, reducing pain’s emotional impact.
Stress Reduction Technique | Description | Benefits |
Mindfulness Meditation | Focusing on the present moment without judgment | Reduces stress, improves pain coping |
Deep Breathing Exercises | Slow, deliberate breathing to calm the nervous system | Decreases anxiety, promotes relaxation |
Progressive Muscle Relaxation | Systematically tensing and relaxing muscle groups | Reduces muscle tension, promotes relaxation |
Support Groups and Community Resources
Support groups and community resources are vital for women with chronic pelvic pain. They offer emotional support and practical advice. Connecting with others who understand can be very empowering.
Support groups are safe spaces for sharing experiences and learning from others. Many organizations provide resources like educational materials, counseling, and advocacy.
By adding psychological support and behavioral interventions to their treatment, women with chronic pelvic pain can see big improvements. Their symptoms and quality of life can greatly improve.
Creating a Multidisciplinary Treatment Plan for Chronic Pelvic Pain Management
A multidisciplinary treatment plan is key for managing chronic pelvic pain in women. It looks at all parts of a patient’s condition. This way, every aspect is managed well.
Assembling Your Healthcare Team
Starting with a diverse healthcare team is the first step. This team should include gynecologists, pain management specialists, physical therapists, and psychologists. Each expert adds their knowledge to create a full treatment plan.
A gynecologist can tackle gynecological issues. A pain management specialist offers pain relief options. Physical therapists work on pelvic floor function. Psychologists help with mental health and coping.
Coordinating Care Across Specialties
It’s important to coordinate care across specialties. Regular talks among team members ensure treatments work together. This avoids conflicting treatments and improves patient care.
Good coordination comes from team meetings, shared records, and clear communication. This teamwork helps make informed decisions and adjust treatments as needed.
Specialty | Role in Treatment Plan | Example Interventions |
Gynecology | Address underlying gynecological conditions | Hormonal therapies, surgical interventions |
Pain Management | Provide pain relief options | Nerve blocks, medication management |
Physical Therapy | Improve pelvic floor function | Pelvic floor exercises, manual therapy |
Tracking Progress and Adjusting Treatments
It’s vital to track patient progress and adjust treatments. Regular checks help see if treatments are working. They also show where changes are needed.
Patients should keep a pain diary. This tracks symptoms and treatment responses. Regular check-ups and feedback from the team allow for timely treatment changes.
With a multidisciplinary plan, women with chronic pelvic pain can see big improvements. This approach tackles the complex nature of chronic pelvic pain. It offers relief and support across health areas.
Living Well Despite Chronic Pelvic Pain: Lifestyle Adaptations
Managing chronic pelvic pain requires both medical treatment and lifestyle changes. By adjusting daily habits and environments, women can greatly improve their life quality. This is true even with this condition.
Workplace Accommodations and Ergonomics
Chronic pelvic pain can make work hard for many women. Simple changes at work can help a lot. These might include ergonomic setups, flexible hours, and breaks to stretch.
Good ergonomics can ease discomfort. For example, the right chair height, monitor level, and breaks to stand can help the pelvic area. This reduces strain.
Workplace Accommodation | Benefit |
Ergonomic seating | Reduces strain on the lower back and pelvis |
Flexible working hours | Allows for managing pain on tough days |
Regular breaks | Reduces sitting or standing for too long |
Sexual Health and Intimacy Considerations
Chronic pelvic pain can also affect a woman’s sex life and closeness. It’s key to talk openly with partners about pain. Trying different positions, using lubricants, and going slow can make sex more comfortable.
Emotional aspects of intimacy are also important. Counseling or therapy can help keep a relationship strong despite pain challenges.
Daily Activity Modifications for Pain Reduction
Changing daily activities can lessen pain. This might mean doing chores differently, using tools that ease pelvic strain, and prioritizing tasks. This avoids overdoing it.
For example, using a vacuum with a long handle can cut down on bending. Doing laundry in smaller loads avoids heavy lifting.
Daily Activity | Modification | Benefit |
Household chores | Using ergonomic tools | Reduces strain on muscles and joints |
Laundry | Doing smaller loads | Avoids heavy lifting |
Gardening | Using raised beds or long-handled tools | Minimizes bending and straining |
By making these lifestyle changes, women with chronic pelvic pain can see big improvements in their life quality. It’s about finding balance and being proactive in managing pain.
Conclusion: Empowering Women in Managing Chronic Pelvic Pain
It’s key to empower women with knowledge and support for managing chronic pelvic pain. Understanding the condition helps women take charge of their health. This improves their quality of life.
We’ve shared important strategies for dealing with chronic pelvic pain. These include medical treatments, physical therapy, pain management, and psychological support. A team approach is vital for meeting the complex needs of women with this condition.
Research shows that education and support are critical in managing chronic pelvic pain. Giving women the right tools and resources helps them understand and manage their condition. This way, they can make better decisions about their care.
Managing chronic pelvic pain is a team effort between healthcare providers and patients. By working together and empowering women, we can better treat this condition. This improves the well-being of women dealing with it.
FAQ
What is chronic pelvic pain syndrome in women?
Chronic pelvic pain syndrome is long-lasting pain in the pelvic area. It lasts more than six months and often has no clear cause. This condition can greatly affect a woman’s life quality.
How common is chronic pelvic pain among women globally?
Chronic pelvic pain is common worldwide. Studies show it affects many women. It needs a full management plan.
What are the common causes of chronic pelvic pain in women?
Chronic pelvic pain can come from many sources. These include gynecological issues, other health problems, and mental health factors. We aim to find the root cause for effective treatment.
How is chronic pelvic pain diagnosed?
Diagnosing chronic pelvic pain starts with a detailed check-up. It includes looking at medical history, physical exams, and tests like imaging. We use a detailed approach to find the cause.
What are the treatment options for managing chronic pelvic pain?
Treatments range from medical care to physical therapy and pain management. We also offer integrative methods and psychological support. Each plan is made for the patient’s specific needs.
How can physical therapy help in managing chronic pelvic pain?
Physical therapy, like pelvic floor therapy, can be very helpful. We help patients create personalized exercise plans to manage pain.
What role do lifestyle adaptations play in managing chronic pelvic pain?
Making lifestyle changes can greatly help. This includes work adjustments, sexual health, and daily habits. We help patients make these changes.
Can chronic pelvic pain be managed without surgery?
Yes, many women manage chronic pelvic pain without surgery. A mix of medical care, physical therapy, and lifestyle changes can work. We look at all options for each patient.
How can I find support for managing chronic pelvic pain?
Finding support is key. We offer psychological help and group support. This includes cognitive behavioral therapy and support groups for holistic care.
What is the importance of a multidisciplinary treatment plan for chronic pelvic pain?
A team approach is vital for managing chronic pelvic pain. We help patients build their healthcare team. This ensures coordinated care and progress tracking.
Are there any complementary therapies that can help manage chronic pelvic pain?
Yes, therapies like acupuncture and mindfulness can help. We discuss these options as part of a full treatment plan.
References
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://pubmed.ncbi.nlm.nih.gov/8595986/