
Pelvic pain when you poop is a big problem for many people. About 16 out of 100 adults deal with constipation. This number goes up a lot in nursing homes.
At Liv Hospital, we know how tough pelvic pain during bowel movements can be. We offer caring and expert help. Chronic pelvic pain is pain below the belly button and between the hips lasting six months or more. It might be a sign of another disease or a problem on its own.
Explaining the mechanisms by which can constipation cause pelvic pain due to straining and rectal fullness.
Key Takeaways
- Pelvic pain during bowel movements is a significant health concern affecting millions worldwide.
- Constipation is a common issue, with approximately 16 out of 100 adults experiencing symptoms.
- Chronic pelvic pain can be a symptom of an underlying condition or a standalone issue.
- Professional medical attention is key for pelvic discomfort during bowel movements.
- Liv Hospital offers caring and wide treatment options for constipation-related pelvic pain.
The Relationship Between Bowel Movements and Pelvic Pain

It’s important to know how bowel habits and pelvic pain are connected. Constipation can lead to pelvic pain because of the pressure it puts on muscles. This happens when stool builds up and is hard to pass.
The Prevalence of Constipation-Related Pelvic Pain
Women with chronic pelvic pain often have constipation. Studies show that constipation is common in those with pelvic pain. This suggests a strong link between bowel function and pelvic health.
How Bowel Function Affects Pelvic Health
Bowel function is key to pelvic health. Irregular or hard bowel movements can strain the pelvic floor muscles. These muscles support the pelvic organs, and problems with them can cause pain.
Study | Population | Findings |
Study 1 | Women with chronic pelvic pain | Higher rates of functional constipation |
Study 2 | Individuals with constipation | Increased prevalence of pelvic floor dysfunction |
Study 3 | Patients with pelvic pain | Significant improvement in pain with bowel habit normalization |
Understanding how bowel movements impact pelvic health is key. This knowledge helps us find better treatments. It focuses on improving both bowel function and pelvic floor health.
The Anatomy of Your Pelvis and Digestive System
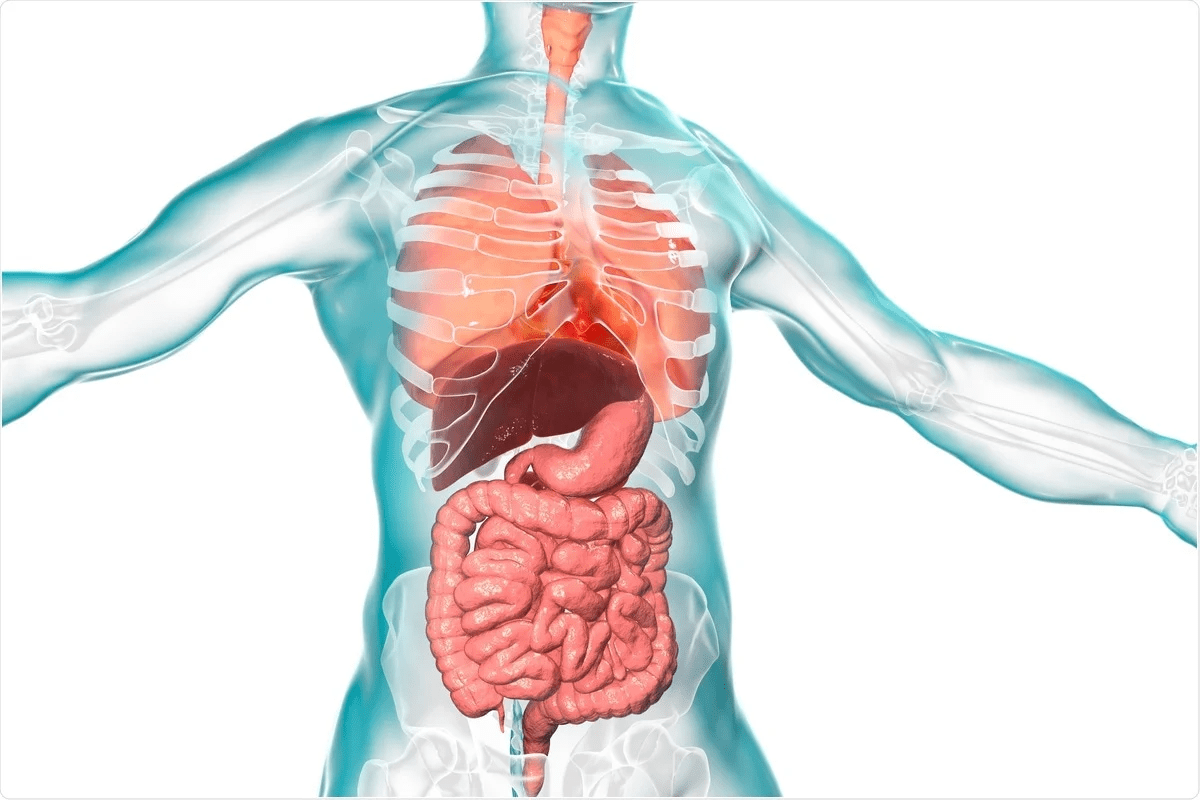
To understand why constipation can cause pelvic pain, we need to look at the anatomy of the pelvis and digestive system. The pelvis is a complex area that holds important organs, including parts of the digestive system.
Pelvic Floor Muscles and Their Function
The pelvic floor muscles are key in supporting the pelvic organs. They stretch from the pubic bone to the coccyx (tailbone) and from one sitting bone to the other. These muscles help control bowel movements and more.
Key functions of the pelvic floor muscles include:
- Supporting pelvic organs
- Regulating bowel movements
- Maintaining continence
How the Colon and Rectum Interact with Pelvic Structures
The colon and rectum are part of the large intestine, a key part of the digestive system. They are in the pelvic cavity and work closely with other pelvic structures.
Structure | Function | Interaction with Pelvic Organs |
Sigmoid Colon | Stores and transports feces | Adjacent to pelvic organs, can exert pressure |
Rectum | Stores feces until elimination | Supported by pelvic floor muscles, interacts with nearby nerves |
Nerve Pathways That Connect Digestive and Pelvic Regions
The digestive and pelvic regions are linked by complex nerve pathways. These nerves send pain signals and are vital for controlling pelvic organ functions.
Understanding these structures and their connections is key to diagnosing and treating pelvic pain caused by constipation. By knowing how the pelvis and digestive system work together, healthcare providers can create better treatment plans.
Can Constipation Cause Pelvic Pain? The Scientific Evidence
Recent studies have shown a link between chronic constipation and pelvic pain. It’s clear that our bowel habits affect our pelvic health.
Research Findings on the Constipation-Pelvic Pain Connection
Many studies have looked into the connection between constipation and pelvic pain. They found that almost half of people with chronic constipation also have pelvic floor issues. This means constipation might make pelvic pain worse.
A study in a well-known medical journal found that people with chronic constipation have more pelvic pain. It showed how bowel function and pelvic muscle tension are connected.
Statistical Relationship Between Chronic Constipation and Pelvic Disorders
Studies have found a strong link between chronic constipation and pelvic disorders. People with chronic constipation often have more pelvic pain than others.
Constipation is often linked with pelvic pain syndrome. This shows why treating bowel issues is key to managing pelvic pain.
Gender Differences in Constipation-Related Pelvic Pain
Research has looked into how men and women experience constipation-related pelvic pain differently. Women are more likely to have pelvic pain due to constipation.
This difference might be due to hormones, pelvic anatomy, and childbirth. Knowing these differences helps in creating better treatments.
Mechanisms Behind Constipation-Related Pelvic Pain
To understand constipation-related pelvic pain, we need to look at several key factors. Constipation can cause pelvic pain in many ways. This makes it a complex issue to solve.
Pressure from Stool Buildup on Surrounding Organs
Stool buildup in the intestines puts pressure on nearby organs. This pressure can cause pain in the pelvic area. The rectum’s fullness can press against muscles and organs, leading to discomfort.
Effects of Straining on Pelvic Floor Muscles
Straining during bowel movements can hurt the pelvic muscles and nerves. This strain adds pressure on the pelvic floor, leading to muscle fatigue and pain. Over time, this can cause chronic pain in the pelvic area.
Referred Pain Patterns in the Pelvis
Constipation can also cause referred pain in the pelvis. The nerves that supply the rectum and pelvic organs can send pain signals to other areas. This can make diagnosis tricky because the pain might feel like it’s coming from somewhere else.
Inflammatory Responses to Chronic Constipation
Chronic constipation can cause inflammation in the pelvic area. The long-term presence of stool can lead to inflammation of the rectal mucosa and surrounding tissues. This inflammation can cause pain and discomfort in the pelvic region.
Mechanism | Description | Effect on Pelvic Region |
Pressure from Stool Buildup | Stool accumulation in intestines | Pressure on pelvic floor muscles, bladder, and reproductive organs |
Effects of Straining | Straining during bowel movements | Muscle fatigue and pain in pelvic floor |
Referred Pain | Nerve referral patterns | Pain in lower back or thighs |
Inflammatory Responses | Prolonged stool presence | Inflammation of rectal mucosa and surrounding tissues |
Why Does My Pelvis Hurt When I Poop? Common Causes
Pelvic pain when you poop is common and can have many causes. Knowing what causes it is key to finding relief. We’ll look at why it happens, including constipation, pelvic floor issues, bowel diseases, and structural problems.
Functional Constipation
Functional constipation means you have hard stools and trouble passing them. This can cause pelvic pain because of the strain. Eating more fiber, drinking water, and having a regular bowel schedule can help.
Pelvic Floor Dysfunction
Pelvic floor dysfunction happens when the pelvic muscles are weak or damaged. This makes bowel movements hard and painful. Physical therapy and exercises can help manage this.
Inflammatory Bowel Conditions
Diseases like Crohn’s and ulcerative colitis can cause pain in the pelvis. This is because of inflammation in the bowel. Medicines to reduce inflammation and suppress the immune system are often used.
One study says, “Inflammatory bowel disease is a chronic condition that needs long-term care to prevent problems and improve life quality.”
“The management of IBD involves a combination of medical therapy, lifestyle modifications, and sometimes surgery.”
Structural Abnormalities Affecting Bowel Movements
Issues like rectal prolapse, rectocele, or anal fissures can also cause pain. Surgery might be needed to fix these problems and ease symptoms.
Specific Types of Pelvic Pain During Bowel Movements
Different people feel different kinds of pelvic pain when they have a bowel movement. This pain can range from a little discomfort to very severe pain. Knowing what kind of pain you have is key to figuring out why and how to feel better.
Dull Aching Pain in the Lower Abdomen
A dull ache in the lower belly is common for those with pelvic pain during bowel movements. This pain feels like a constant, annoying ache that can happen before or after you go. It might just be in one spot or spread out across your lower belly.
Sharp Pain During Straining
Sharp pain when you strain is another kind of pelvic pain. This pain is sharp and stabbing, happening when you push hard during a bowel movement. It can be scary and make you worry about what’s going on.
Fullness and Pressure Sensations
Some people feel full or pressurized in their pelvis during bowel movements. This feeling is uncomfortable and might make you feel like you’re not done. The pressure can change and might be because of stool or other issues with your pelvic muscles.
Radiating Pain to the Lower Back and Thighs
Pelvic pain can also spread to your lower back and thighs. This happens because nerves in your pelvis connect to these areas. Knowing where the pain goes can help doctors figure out what’s causing it.
It’s important to know the different kinds of pelvic pain during bowel movements. This helps you get the right medical help and treatment. By describing your pain well, you can get a better diagnosis and treatment plan.
When Pelvic Pain Affects Specific Organs
Pelvic pain can show up in many ways, hitting different organs in the pelvic area. It’s not just a minor ache; it might signal a bigger issue that needs doctor’s care. We’ll look at how pelvic pain can tie to specific organs, like the uterus, ovaries, and bladder.
Why Your Uterus Might Hurt When Pooping
Feeling pain in the uterus when you poop can be scary. Issues like endometriosis and fibroids might be the cause. Endometriosis happens when tissue like the uterus lining grows outside the uterus, causing pain. Fibroids, which are non-cancerous growths in the uterus, can also cause pain during bowel movements.
Other possible causes include:
- Adenomyosis, where tissue like the uterus lining grows into the muscular walls of the uterus.
- Pelvic inflammatory disease (PID), an infection of the female reproductive organs.
Ovarian Pain Related to Constipation
Ovarian pain can sometimes be linked to constipation. When stool builds up in the colon, it can press on the ovaries, causing pain. This is more common with severe constipation where the stool is hard and hard to pass.
It’s essential to note that ovarian pain can also be caused by other conditions such as ovarian cysts or torsion. If you’re experiencing persistent or severe ovarian pain, it’s vital to see a healthcare provider.
One-Sided Pelvic Pain During Bowel Movements
One-sided pelvic pain during bowel movements can have many causes. It might be related to the colon or rectum, like diverticulitis or an anal fissure. Or, it could be related to the reproductive organs, like an ovarian cyst on one side.
To figure out the cause, a healthcare provider might do a physical exam, ask for your medical history, and possibly order imaging tests.
Bladder Pressure and Urinary Symptoms
Bladder pressure and urinary symptoms often go hand in hand with pelvic pain. Constipation can put pressure on the bladder, leading to symptoms like needing to pee a lot or feeling like you didn’t empty your bladder fully.
In some cases, pelvic pain and urinary symptoms can be linked to conditions like interstitial cystitis, a chronic condition causing bladder pressure and pain.
Understanding the link between pelvic pain and specific organs is key for the right diagnosis and treatment. If you’re dealing with persistent or severe pelvic pain, it’s important to see a healthcare provider to find out the cause and get the right treatment.
Diagnosing the Cause of Pelvic Pain During Bowel Movements
Finding the right cause of pelvic pain is key. Doctors use many steps to figure this out. They look at your medical history, do a physical check, and run tests.
Medical History and Physical Examination
Knowing your medical history is very important. Doctors want to know about your pain, how long it lasts, and your bowel habits. They also check your pelvic area to see if there are any problems.
Diagnostic Tests and Procedures
There are many tests to find out why you have pelvic pain. These include:
- Imaging studies: Like X-rays and MRI to see inside your body.
- Endoscopy: This lets doctors look inside your colon and rectum.
- Anorectal manometry: It checks how well your muscles work.
- Ultrasound: This test looks at your pelvic organs.
These tests help doctors find the cause of your pain. Then, they can plan the best treatment.
Differential Diagnosis: When It’s Not Just Constipation
Constipation is a common reason for pelvic pain. But, other things can cause it too. These include:
- Pelvic floor dysfunction: Weak or tight muscles in the pelvic area.
- Inflammatory bowel disease: Conditions like Crohn’s disease or ulcerative colitis.
- Endometriosis: When endometrial tissue grows outside the uterus.
- Structural abnormalities: Issues like rectal prolapse or anal fissures.
By doing a detailed check, doctors can find out what’s really causing your pain.
The Role of Pelvic Floor Assessment
Checking the pelvic floor is very important. Doctors look at the strength and how well the muscles work. They might use a digital rectal exam or other tests. This helps them find the right treatment for you.
Doctors use your medical history, physical check, tests, and pelvic floor assessment to find the cause of your pain. Then, they can make a treatment plan that works for you.
When to Seek Medical Help for Pelvic Pain and Constipation
Knowing when to get medical help is key for managing pelvic pain and constipation. While some discomfort is normal, certain signs mean you should see a doctor.
Warning Signs That Require Immediate Attention
Some symptoms are serious and need immediate care. These include:
- Severe pain that makes it hard to do daily tasks or comes with vomiting, fever, or bleeding.
- Bleeding from the rectum, which could mean a serious issue like a fissure or hemorrhoids.
- Changes in bowel habits that last, like constant constipation or diarrhea.
- Unexplained weight loss, which might show a problem with bowel function.
Chronic Symptoms That Warrant Medical Evaluation
If you have ongoing pelvic pain and constipation, see a doctor. These symptoms can point to serious issues like:
- Pelvic floor dysfunction, where the muscles around the pelvic organs are weak or don’t work right.
- Irritable Bowel Syndrome (IBS), marked by stomach pain and bowel changes.
- Endometriosis, where tissue like the uterus lining grows outside, causing pain.
Getting a diagnosis early can greatly improve your life. A doctor can help manage symptoms and find the cause.
Finding the Right Healthcare Provider
It’s important to find a doctor who knows about pelvic pain and constipation. Look for:
- A primary care doctor for first checks and referrals.
- A gastroenterologist for digestive issues.
- A urogynecologist or pelvic medicine specialist for pelvic floor problems.
If you’re not feeling heard, get a second opinion. Your doctor should listen, explain things clearly, and help create a treatment plan with you.
Treatment Options for Constipation-Related Pelvic Pain
Managing constipation-related pelvic pain requires a detailed plan. It’s important to tackle both physical and lifestyle factors. This approach helps improve pelvic health.
Dietary and Lifestyle Changes
Changing your diet is key in managing constipation and pelvic pain. Eating more fiber from fruits, veggies, and whole grains softens stool. Drinking enough water also helps prevent constipation. Regular exercise and a set bowel routine can also help manage symptoms.
A healthcare expert says, “A high-fiber diet can help reduce symptoms of constipation and alleviate pelvic pain.”
“A well-balanced diet rich in fiber, along with regular physical activity, can significantly improve bowel function and reduce pelvic discomfort.”
Medications and Supplements
If diet changes don’t work, medications and supplements can help. Over-the-counter laxatives and stool softeners can ease constipation. Some medications can also help with bloating and discomfort. Always talk to a doctor before starting new medications or supplements.
- Bulk-forming laxatives
- Osmotic laxatives
- Stool softeners
- Lubricant laxatives
Physical Therapy for Pelvic Floor Dysfunction
Physical therapy is great for pelvic floor issues linked to constipation. A physical therapist can teach exercises to strengthen the pelvic floor. This helps improve bowel function.
Biofeedback and Relaxation Techniques
Biofeedback and relaxation methods can also help with pelvic pain. Biofeedback helps control pelvic muscles. Techniques like deep breathing and progressive muscle relaxation reduce stress and help with bowel regularity.
By using these treatments, people can manage constipation-related pelvic pain better. This improves their overall quality of life.
Preventing Pelvic Pain Associated with Bowel Movements
To prevent pelvic pain, it’s important to know what causes it. By making healthy choices and adopting good habits, you can lower your risk of pelvic pain. This is true for pain during bowel movements.
Dietary Strategies for Regular Bowel Movements
Eating a balanced diet is key to regular bowel movements and avoiding pelvic pain. Increasing fiber from fruits, veggies, and whole grains softens stool. This makes it easier to pass without straining. Also, drinking enough water helps prevent constipation by keeping stool soft.
Be careful of foods that might make pelvic pain worse. Foods like spicy or high-fat ones can upset your stomach and cause pain.
Proper Toilet Posture and Habits
Using the right toilet posture and habits can help prevent pelvic pain. Relax your body while on the toilet, with your feet flat or on a footstool. This reduces straining. Also, don’t delay bowel movements to avoid constipation and pelvic floor pressure.
Take your time to completely empty your bowels. Rushing can lead to pain. And, don’t strain or push during bowel movements to avoid hurting your pelvic floor muscles.
Pelvic Floor Exercises for Prevention
Pelvic floor exercises, like Kegels, strengthen muscles that support your pelvic organs. They improve bowel function. These exercises help tone the muscles and lower pain risk.
Doing these exercises regularly improves pelvic floor function. This reduces dysfunction and pain risk.
Stress Management and Its Impact on Bowel Function
Managing stress is vital in preventing pelvic pain from bowel movements. Stress can worsen bowel issues and cause pain. Activities like meditation, yoga, or deep breathing can help reduce stress.
By following these tips, you can lower your risk of pelvic pain during bowel movements. This improves your overall well-being.
Conclusion: Taking Control of Your Pelvic Health and Bowel Function
Understanding how bowel movements and pelvic pain are connected is key to managing your pelvic health. Knowing the causes and treatments for constipation-related pelvic pain helps you make better choices for your care.
Managing pelvic pain and constipation needs a full plan, including lifestyle changes and medical treatments. We’ve looked at how constipation can cause pelvic pain, from pressure to inflammation.
By changing your diet, using the right toilet posture, and doing pelvic floor exercises, you can avoid pelvic pain from bowel issues. Stress management also plays a big role in keeping your bowel function healthy.
Improving pelvic health and bowel function requires a team effort. Working with healthcare providers and making smart lifestyle choices can help ease symptoms and enhance your life quality. We urge readers to take charge of their pelvic health and seek medical help when necessary.
FAQ
Can constipation cause uterus pain?
Yes, constipation can cause uterus pain. The pressure from stool buildup in the rectum can put pressure on the uterus, leading to discomfort or pain.
Why does my pelvic hurt when I poop?
Pelvic pain during bowel movements can be caused by several factors. These include constipation, pelvic floor dysfunction, or inflammatory bowel conditions. The straining associated with constipation can put additional pressure on the pelvic floor muscles, leading to pain.
Can constipation cause pelvic pain on one side?
Yes, constipation can cause pelvic pain on one side. The pain can be referred to one side of the pelvis due to the anatomical relationship between the rectum, sigmoid colon, and surrounding pelvic structures.
Why does my uterus hurt when I poop?
Uterus pain during bowel movements can be related to constipation, endometriosis, or other conditions that affect the pelvic organs. The pressure from stool buildup or the hormonal changes associated with menstruation can contribute to uterus pain.
Can constipation cause pain in the ovaries?
While constipation is not a direct cause of ovarian pain, it can contribute to discomfort in the pelvic region. This discomfort may be felt in the ovaries. The proximity of the ovaries to the rectum and sigmoid colon can lead to referred pain.
Does constipation cause pelvic pain?
Yes, constipation can cause pelvic pain. The mechanisms behind this include pressure from stool buildup, effects of straining on pelvic floor muscles, and referred pain patterns.
What are the common causes of pelvic pain during bowel movements?
Common causes include functional constipation, pelvic floor dysfunction, inflammatory bowel conditions, and structural abnormalities affecting bowel movements.
How is pelvic pain during bowel movements diagnosed?
Diagnosis involves a medical history, physical examination, diagnostic tests (such as imaging studies or endoscopy), and pelvic floor assessment. This helps determine the underlying cause of the pain.
What are the treatment options for constipation-related pelvic pain?
Treatment options include dietary and lifestyle changes, medications and supplements, physical therapy for pelvic floor dysfunction, and biofeedback and relaxation techniques.
How can I prevent pelvic pain associated with bowel movements?
Prevention strategies include dietary changes to promote regular bowel movements, proper toilet posture and habits, pelvic floor exercises, and stress management techniques.
When should I seek medical help for pelvic pain and constipation?
You should seek medical help if you experience warning signs that require immediate attention. This includes severe pain or bleeding. Also, if you have chronic symptoms that warrant medical evaluation.
References
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1120267/








