Last Updated on November 13, 2025 by
Managing pain well is key during sickle cell disease episodes. It greatly affects how sick a patient gets and their quality of life. We see pain control as more than just easing pain right away. It’s about making a big difference in a patient’s long-term health. Vaso-occlusive sickle cell crisis is a big problem in sickle cell disease, causing significant suffering. Our pain management plan is to understand this condition well. We use sickle cell crisis pain management protocols that help with both physical and emotional pain.
By focusing on good pain management, we can greatly improve patients’ lives during vaso-occlusive sickle cell crises. This approach not only helps with pain right away. It also helps patients stay well in the long run.
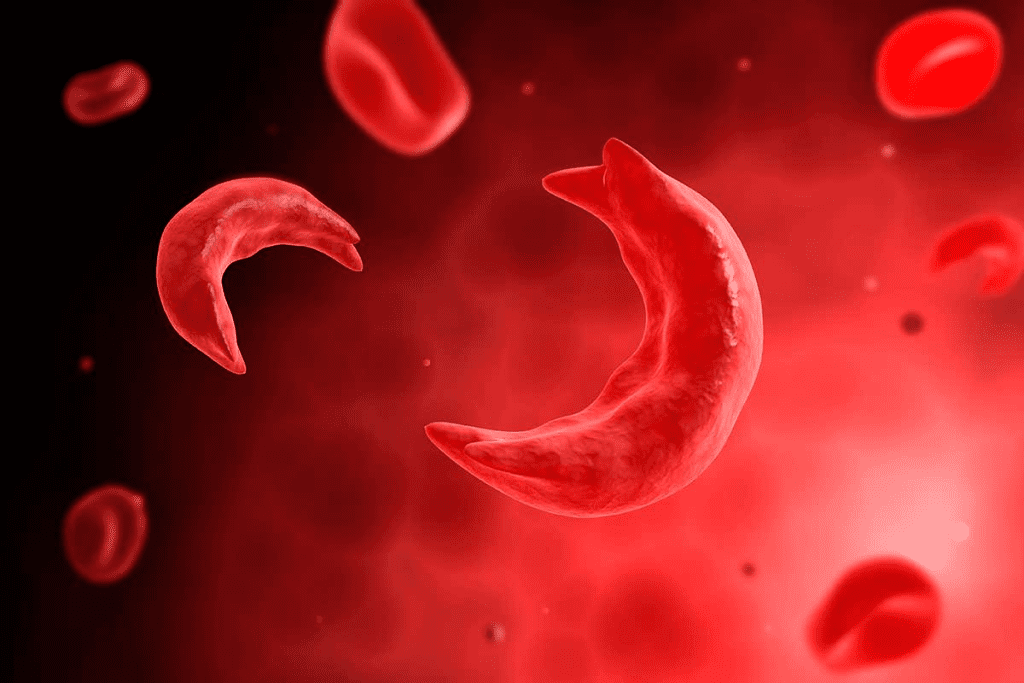
Vaso-occlusive episodes in sickle cell disease cause severe pain. This makes managing pain a key part of caring for patients. Sickle cell disease is a genetic disorder that leads to abnormal hemoglobin production. This results in red blood cells sickling and blocking blood vessels, causing pain.
The pain from sickle cell disease comes from vaso-occlusive crises. Sickled red blood cells block blood vessels. This blockage causes tissue ischemia and severe pain.
Understanding the pain mechanisms in sickle cell disease is key to effective pain management. The pain can be so bad it affects daily life and quality of life.
Sickle cell disease affects millions worldwide, with about 300,000 children born with it each year. The pain from sickle cell crises is a big health issue, affecting healthcare systems a lot.
Research shows patients with sickle cell disease often have recurring pain. Some need to go to the hospital often. The severity and frequency of these episodes highlight the need for good pain management.
Knowing the pain statistics helps healthcare providers create better pain management plans for sickle cell disease patients.
For those with sickle cell disease, managing pain is key. It helps reduce complications and makes daily life better. Good pain management covers many areas of care.
Most hospital visits by sickle cell patients are due to pain. By managing pain well, we can lower hospital stays. This improves health and saves money for healthcare.
Poor pain control can lead to more hospital visits and worse health. Good pain management stops long-term problems. It reduces pain episodes and lowers the risk of organ damage.
Pain management is more than just easing pain. It makes life better for sickle cell patients. Effective pain care lets patients do more, work, and live better.
Good pain management cuts healthcare costs. It lowers hospital stays and reduces expensive treatments. This helps patients and makes healthcare more affordable.
Healthcare providers need to understand these points. They should create detailed pain management plans for sickle cell patients. Our goal is to give personalized care that improves lives and outcomes.
Inadequate pain management in vaso-occlusive crises has severe effects. Patients with Sickle Cell Disease (SCD) face both acute and chronic pain. Acute pain comes from unpredictable and recurring crises. If pain is not managed well, it can lead to more hospital visits and worse health outcomes.
Poor pain control often means more hospital stays for SCD patients. These frequent visits can disrupt a patient’s life and strain healthcare systems. Research shows that those with unmanaged pain are more likely to be readmitted. This highlights the need for better pain control strategies.
Also, poor pain management can cause chronic pain syndromes. Chronic pain makes daily tasks hard and lowers quality of life. Moving from acute to chronic pain makes treatment harder. This shows why early and effective pain management is key.
Knowing these effects stresses the need for detailed pain management plans. These plans should cover both acute and chronic pain in SCD. This way, we can improve patient outcomes and lessen the healthcare costs of SCD.
Managing vaso-occlusive sickle cell crisis is key to easing patient pain and achieving better outcomes. Places like Liv Hospital use the newest research and team efforts for pain care.
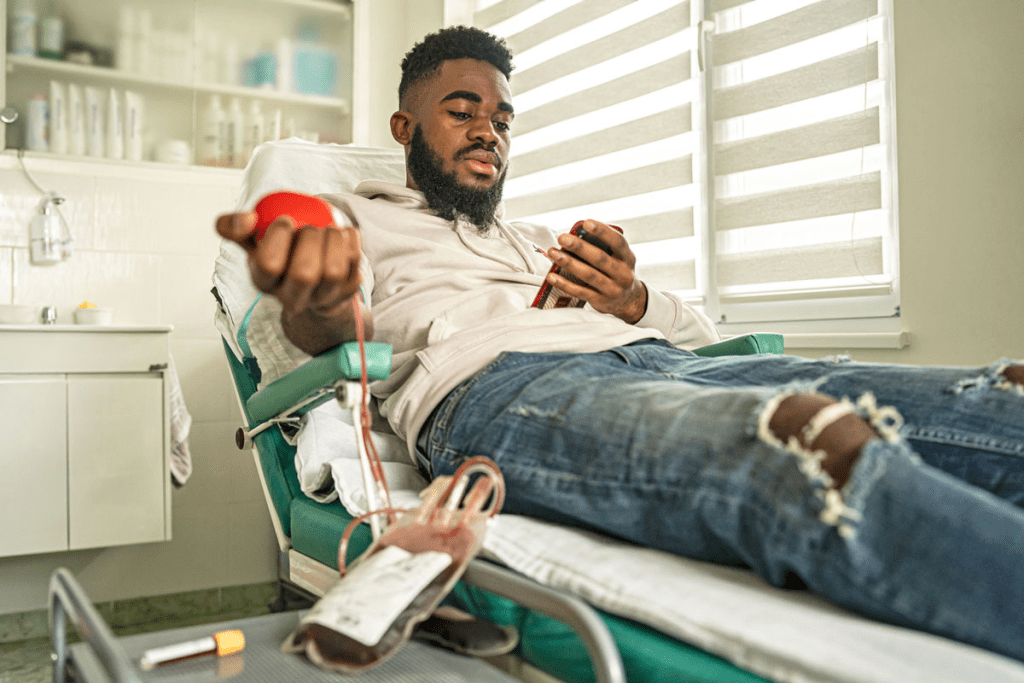
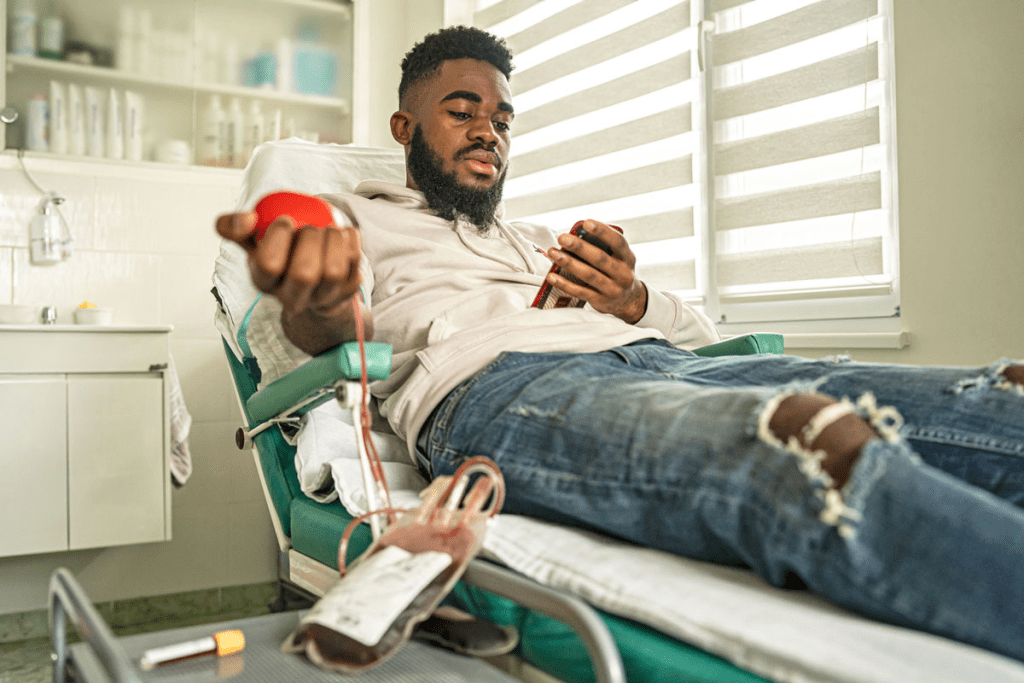
The National Heart, Lung and Blood Institute suggests strong opioid use for VOC pain. In the emergency room, we quickly check the patient’s pain and start the right pain relief.
Rapid assessment is vital. We use pain scales to measure pain levels. Aggressive opioid therapy is then adjusted for each patient, based on their health history and past pain responses.
In the hospital, we use many ways to manage pain. This includes medicines and non-medical methods to control pain well.
Our detailed pain management plan helps patients recover faster and feel better. Our methods are flexible, so we can change them as needed for each patient.
Getting the right pain relief for a sickle cell crisis is hard. Many obstacles stand in the way. We need to know these challenges to help patients better.
There are big differences in how sickle cell disease is managed across regions. These differences can cause patients to suffer more. For example, rural areas often lack access to the care they need.
Doctors might be biased against patients with sickle cell disease. They worry more about opioid addiction in these patients. This can mean patients don’t get the pain relief they need. It’s key to educate doctors to ensure fair treatment.
The opioid crisis has made doctors more careful with pain meds. But, this caution can sometimes mean not treating pain enough. We need to find a balance in how we prescribe opioids.
Many doctors don’t know enough about sickle cell disease and how to manage its pain. This lack of knowledge can lead to poor care. Training programs can help doctors provide better care.
In summary, fixing the pain relief issues in sickle cell crisis needs a wide-ranging solution. We must tackle regional care gaps, doctor bias, opioid worries, and knowledge gaps. This way, we can improve care and outcomes for patients.
New strategies are changing how we handle pain in sickle cell disease. Advances in treatments and pain management are making life better for patients. Now, care is more complete and tailored to each person’s needs.
Cognitive Behavioural Therapy (CBT) is helping patients with sickle cell disease. It teaches them how to manage stress and pain. This way, CBT reduces pain episodes and improves mental health.
CBT also helps with the emotional side of chronic illness. It’s a key part of treating vaso occlusive crisis. Healthcare providers use it to help patients feel better overall.
Looking for safer pain meds than morphine is a big focus. New drugs like crizanlizumab and L-glutamine are being tested. They might prevent pain crises in sickle cell patients.
These new meds could make life better for patients. They offer hope for less pain and fewer hospital visits. This is a big step forward in treating sickle cell disease.
Teams of experts are key in treating vaso occlusive crisis. They include doctors, pain specialists, and psychologists. This team approach ensures patients get care that fits their needs.
These teams improve communication and care coordination. They help address all aspects of a patient’s health. This is very important for patients with sickle cell disease.
Patient-Controlled Analgesia (PCA) systems are a big step forward. They let patients control their pain relief. This has been shown to reduce pain and hospital stays.
PCA systems give patients more control over their pain. This makes them happier and leads to better outcomes. It also lets doctors tailor care to each patient’s needs.
Patients with sickle cell disease can greatly improve their lives by managing their condition. By taking charge of their care, they can lead healthier lives. This approach helps manage crisis pain more effectively.
It’s important to spot the early signs of a crisis. Patients should watch for pain, fatigue, or other symptoms. Catching these signs early can help prevent or lessen a crisis.
Drinking enough water is key to avoiding crises. Dehydration can make a crisis worse. Patients should also avoid extreme temperatures, manage stress, and exercise regularly.
Managing pain at home is vital for sickle cell patients. They can use medication, heat or cold packs, and relaxation techniques. Techniques like deep breathing or meditation can help reduce pain and stress.
Relaxation techniques can help reduce stress and alleviate pain. Patients are encouraged to explore different methods to find what works best for them.
Managing pain in sickle cell disease needs a team effort. We must understand the disease, current treatments, and barriers to care. This way, we can make life better for those affected.
The Helping to End Addiction Long-term Initiative (HEAL) is working hard to find new pain treatments. This is a big step towards better care for sickle cell crisis. We promise to give top-notch healthcare to patients from around the world.
We must keep looking for new ways to tackle the sickle cell crisis. By working together, we can improve care and find effective solutions. This will help those living with this condition.
A vaso-occlusive crisis is a sudden pain episode. It happens when sickled red blood cells block blood vessels. This leads to tissue ischemia and pain.
Sickle cell disease causes pain through vaso-occlusive crises. Sickled red blood cells block blood vessels. This causes tissue ischemia and pain.
Effective pain management is key in sickle cell disease. It lowers hospital admission rates and prevents long-term complications. It also improves daily life and reduces healthcare costs.
Inadequate pain control can lead to more hospital readmissions. It can also cause chronic pain syndromes.
Current protocols include emergency department approaches and inpatient pain management strategies.
Barriers include regional disparities in care and provider bias. Opioid prescribing concerns and a lack of specialized knowledge also exist.
Innovative approaches include cognitive behavioural therapy and alternative medications to morphine. Multidisciplinary pain management teams and patient-controlled analgesia systems are also used.
Patients can recognize early warning signs and adopt hydration and preventive measures. They can also use home pain management techniques to prevent crises and improve their quality of life.
Pain management is critical. It directly affects patient outcomes. Effective pain management strategies are essential for improving patient outcomes and quality of life.
Effective pain management can reduce hospital admission rates. It prevents severe pain episodes that require hospitalization.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!