A comprehensive list of the serious medical conditions, from viral infections to blood disorders, that are the underlying causes thrombocytopenia is provided.
Thrombocytopenia is a condition where you have a low platelet count, usually under 150,000/μL. It can point to several health issues, from infections to autoimmune diseases.
At LivHospital, we know how key it is to find the many causes of thrombocytopenia. This helps us treat it quickly and well. Many things can lead to this condition, like autoimmune diseases, infections, and liver problems.
It’s vital to understand the main causes of thrombocytopenia for top-notch healthcare. We aim to give full care to those with this condition. Our team uses our knowledge to meet their specific needs.
Key Takeaways
- Thrombocytopenia is characterized by a low platelet count.
- Autoimmune disorders, infections, and liver disease can cause thrombocytopenia.
- Identifying the underlying causes is key for effective treatment.
- Liv Hospital offers complete care for patients with thrombocytopenia.
- Quick diagnosis and treatment are vital for managing thrombocytopenia.
Understanding Thrombocytopenia: Definition and Clinical Significance
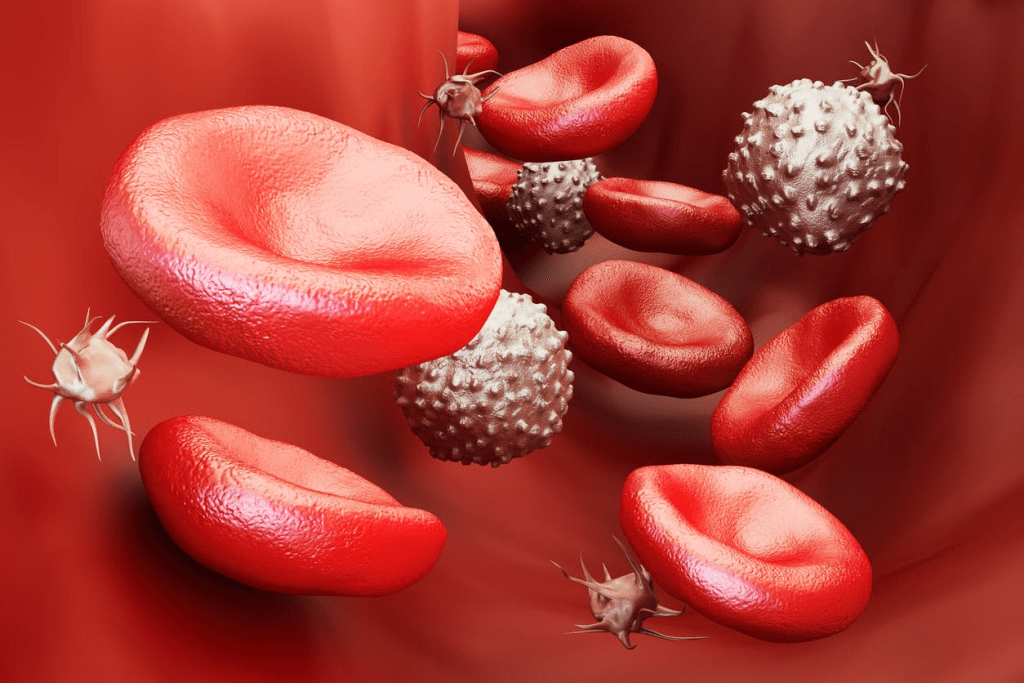
Thrombocytopenia is a condition where you have too few platelets. It’s a serious issue that needs to be understood well. We’ll look into what it is, what a normal platelet count is, and why it matters. This will help you understand this condition better.
What defines a low platelet count?
A low platelet count, or thrombocytopenia, means having less than 150,000 platelets per microliter. Platelets help your blood clot, and not enough can make you bleed more easily. Knowing when you have too few platelets is key for treatment.
Normal platelet values and clinical thresholds
Platelet counts should be between 150,000 and 450,000/μL. This range is usually good for blood clotting. If your count is below 150,000/μL, it might mean you have thrombocytopenia. How bad it is depends on the count. Counts under 50,000/μL are moderate, and under 20,000/μL are severe.
Signs and symptoms of thrombocytopenia
The symptoms of thrombocytopenia can differ based on how bad it is. You might see small red spots on your skin, bigger bruises, or bleeding gums or nosebleeds. Severe cases can be very dangerous. It’s important to notice these signs to get medical help fast.
We’ve covered what thrombocytopenia is, its normal platelet count, and its symptoms. Knowing these details is important for diagnosing and treating thrombocytopenia.
The Underlying Causes of Thrombocytopenia: Pathophysiological Mechanisms
Thrombocytopenia can stem from several causes. These include less platelet production, more platelet destruction, and splenic sequestration. Knowing these causes is key to diagnosing and treating the condition well.
Decreased Platelet Production Mechanisms
When the bone marrow doesn’t make enough platelets, thrombocytopenia can happen. This can be due to:
- Bone marrow failure: Conditions like aplastic anemia, where the bone marrow fails to produce blood cells.
- Leukemia or lymphoma: Cancers that infiltrate the bone marrow, disrupting normal blood cell production.
- Myelodysplastic syndromes: Disorders characterized by ineffective hematopoiesis, leading to reduced platelet production.
- Nutritional deficiencies: Lack of essential nutrients like vitamin B12 or folate, which are vital for platelet production.
Increased Platelet Destruction Pathways
Thrombocytopenia can also be caused by more platelet destruction. This can happen through:
- Immune-mediated destruction: Autoantibodies against platelets, as seen in Immune Thrombocytopenia (ITP).
- Drug-induced thrombocytopenia: Certain medications can induce immune-mediated platelet destruction.
- Infections: Viral infections like HIV, hepatitis C, and dengue fever can lead to increased platelet destruction.
Splenic Sequestration and Platelet Pooling
Splenic sequestration happens when an enlarged spleen holds onto platelets. This reduces the number of platelets in the blood. This can be caused by:
- Liver disease: Cirrhosis and portal hypertension can lead to splenomegaly and subsequent platelet sequestration.
- Myeloproliferative disorders: Conditions like myelofibrosis can cause splenic enlargement.
Understanding these mechanisms is vital for treating thrombocytopenia. By knowing the cause, doctors can create a treatment plan that targets the specific problem.
Immune Thrombocytopenia (ITP): Primary Autoimmune Destruction
Immune thrombocytopenia (ITP) is a complex autoimmune disorder. It causes low platelet counts because of immune destruction. Knowing how it works is key to diagnosing and treating it.
Pathophysiology of Autoantibody Production
ITP is marked by autoantibodies against platelets. These autoantibodies tell the spleen to destroy platelets. This process involves T cells and B cells working together to make antibodies against platelet antigens.
Key mechanisms include:
- Molecular mimicry triggering autoimmunity
- Dysregulation of immune checkpoints
- Activation of autoreactive lymphocytes
Primary vs. Secondary ITP Differentiation
ITP can be either primary or secondary. Primary ITP has no other cause and just low platelets. Secondary ITP happens with other diseases or infections.
Differentiation is key for the right treatment. Secondary ITP might need treatment for the underlying condition, plus treatments for low platelets.
Diagnostic Criteria and Clinical Presentation
Diagnosing ITP involves looking at symptoms and lab results. Symptoms include:
- Petechiae or purpura
- Mucocutaneous bleeding
- Easy bruising
Tests like a complete blood count (CBC) and peripheral blood smear are used. Bone marrow exams might also be done to check platelet production.
Understanding ITP’s pathophysiology and symptoms is vital for doctors. It helps them make better decisions for diagnosis and treatment. This way, we can improve care and outcomes for patients.
Viral Infections as Triggers for Low Platelet Counts
Viral infections can lead to low platelet counts in several ways. They can directly harm megakaryocytes, destroy platelets through the immune system, or trap them in the spleen.
HIV-associated thrombocytopenia mechanisms
HIV can cause low platelet counts in many ways. It can infect megakaryocytes, which are key to making platelets. HIV also triggers the immune system to attack platelets, marking them for destruction.
Immune thrombocytopenia (ITP) often occurs in people with HIV. This condition happens when the body makes antibodies against platelet proteins. These antibodies help the spleen clear out platelets.
Hepatitis C and platelet dysfunction
Hepatitis C virus (HCV) is another major cause of low platelet counts. It can cause chronic liver disease, leading to spleen problems and high blood pressure in the liver. These issues can trap platelets and lower their count.
HCV also directly affects how platelets are made and how they work. This can further reduce the number of platelets in the blood.
Epstein-Barr virus effects on megakaryocytes
The Epstein-Barr virus (EBV) can infect megakaryocytes and other bone marrow cells. This disrupts platelet production. EBV can also trigger the immune system to destroy platelets.
In some cases, EBV-related low platelet counts can be very severe. They may need special treatments.
Dengue fever and acute thrombocytopenia
Dengue fever, caused by the dengue virus, leads to sudden drops in platelet counts. The virus can slow down bone marrow, reducing platelet production. It can also cause blood vessels to leak and affect blood clotting, adding to the low platelet count.
It’s important to understand how different viruses cause low platelet counts. This knowledge helps in finding better treatments.
Bone Marrow Suppression and Malignancy-Related Causes
The link between bone marrow suppression and thrombocytopenia is complex. It involves many mechanisms. Bone marrow suppression, often from chemotherapy or radiation, can greatly reduce platelet production, causing thrombocytopenia.
Chemotherapy-Induced Thrombocytopenia
Chemotherapy is a major reason for thrombocytopenia in cancer patients. Chemotherapy-induced thrombocytopenia happens because chemotherapy agents harm the bone marrow. This affects the production of megakaryocytes, which are the precursors to platelets. As a result, the platelet count drops significantly.
“The management of chemotherapy-induced thrombocytopenia is key to avoid bleeding and keep cancer treatment going,” says the importance of watching closely and taking the right steps.
Radiation Effects on Megakaryocyte Production
Radiation therapy, when aimed at the bones or pelvis, can harm the bone marrow. This makes it hard for the marrow to produce platelets. The damage’s extent depends on the radiation dose and area. Radiation-induced bone marrow suppression can be short-term or permanent, based on the treatment’s intensity.
Leukemia and Myelodysplastic Syndromes
Leukemia and myelodysplastic syndromes directly harm the bone marrow’s ability to make blood cells, including platelets. Leukemia can cause thrombocytopenia by filling the bone marrow with cancer cells, pushing out normal cells. Myelodysplastic syndromes, with their ineffective blood cell production, also lower platelet counts.
Bone Marrow Infiltration by Malignant Cells
Cancer cells in the bone marrow can disrupt normal blood cell production. This can lead to thrombocytopenia because cancer cells replace normal marrow elements. Treating the underlying cancer is essential in such cases.
Chronic Liver Disease and Cirrhosis-Associated Thrombocytopenia
Thrombocytopenia, or low platelet count, is common in chronic liver disease and cirrhosis. It affects how these patients are managed and their outlook.
Cirrhosis and chronic liver disease cause thrombocytopenia in several ways. We will look at these ways and their effects on patients.
Portal Hypertension and Splenic Sequestration
Portal hypertension is a key factor. It happens when blood flow through the liver is blocked. This blockage makes the spleen bigger and holds more platelets, reducing their number in the blood.
Key factors contributing to portal hypertension include:
- Liver fibrosis and cirrhosis
- Increased resistance to hepatic sinusoids
- Splenic enlargement
The spleen plays a big role in holding platelets. When it gets bigger, it keeps more platelets, lowering their count in the blood.
Thrombopoietin Production Deficiency
Thrombopoietin is a hormone made by the liver that helps make platelets. In chronic liver disease, the liver can’t make enough thrombopoietin. This leads to fewer platelets.
The less thrombopoietin there is, the more severe the low platelet count. This makes the situation more complex.
Prevalence and Severity in Cirrhosis Patients
Thrombocytopenia is common in cirrhosis patients. It affects their treatment and management. The severity of thrombocytopenia often matches the liver disease stage.
The clinical implications include:
- Increased risk of bleeding
- Limitations in treatment options for underlying liver disease
- Potential need for platelet transfusions or other interventions
Understanding thrombocytopenia in chronic liver disease and cirrhosis is key to good patient care. We must consider these factors when planning treatment.
Systemic Autoimmune Diseases Affecting Platelet Counts
Systemic autoimmune diseases can lead to thrombocytopenia, a condition with low platelet counts. These diseases make the body’s immune system attack its own tissues. This can harm various organs, including those that make blood cells.
Mechanisms in Systemic Lupus Erythematosus
Systemic lupus erythematosus (SLE) is a key autoimmune disease that can cause low platelet counts. Autoantibodies in SLE target platelets for destruction. This is a main reason why SLE leads to low platelet counts.
Antiphospholipid Syndrome and Platelet Activation
Antiphospholipid syndrome (APS) also causes thrombocytopenia. APS has antibodies that activate platelets, leading to their destruction. This results in low platelet counts. APS is known for causing blood clots even with low platelet counts.
Immune Dysregulation in Rheumatoid Arthritis
Rheumatoid arthritis (RA) mainly affects joints but can also lower platelet counts. The chronic inflammation and immune complexes in RA can harm platelet production and survival.
Vasculitis-Associated Thrombocytopenia
Vasculitis, or inflammation of blood vessels, can also lower platelet counts in some autoimmune diseases. The inflammation can damage blood vessels, affecting platelet counts. This can happen through direct damage or through immune mechanisms.
It’s important to understand how systemic autoimmune diseases affect platelet counts. We need to look at how immune dysregulation, autoantibodies, and direct effects on platelet production and survival work together.
Sepsis, Metabolic Disorders, and Nutritional Deficiencies
It’s important to understand how sepsis, metabolic disorders, and nutritional deficiencies affect platelet production. These factors can lead to thrombocytopenia, a condition where there are not enough platelets in the blood.
Sepsis-Induced Coagulopathy and Platelet Consumption
Sepsis is a serious condition that can cause thrombocytopenia. It happens because the body’s inflammatory response can lead to blood clots in small vessels. This consumes platelets, causing a drop in their numbers.
Sepsis-induced coagulopathy involves both pro-coagulant and anti-coagulant pathways. This makes it a complex issue.
- Activation of the coagulation cascade
- Release of pro-inflammatory cytokines
- Endothelial damage
Vitamin B12 and Folate Deficiency Effects
Vitamin B12 and folate are key for making platelets. Without enough of these vitamins, the bone marrow can’t produce platelets properly. This leads to thrombocytopenia.
Metabolic Disorders Impacting Thrombopoiesis
Metabolic disorders can harm platelet production. Conditions like diabetes and obesity cause chronic inflammation and oxidative stress. This can damage the bone marrow’s ability to make platelets.
Understanding the metabolic underpinnings of thrombocytopenia is key to finding new treatments.
- Chronic inflammation
- Oxidative stress
- Impaired megakaryocyte function
Alcohol-related Thrombocytopenia
Drinking alcohol can also cause thrombocytopenia. Alcohol can lower platelet production and lead to nutritional deficiencies. This makes thrombocytopenia worse.
Alcohol-related thrombocytopenia can improve with stopping drinking and getting the right nutrients.
Drug-Induced Thrombocytopenia: Mechanisms and Common Medications
Thrombocytopenia, or low platelet count, can be caused by many drugs. This includes heparin, certain antibiotics, and chemotherapeutic agents. Drug-induced thrombocytopenia is a big worry in healthcare because it can lead to bleeding problems.
Heparin-Induced Thrombocytopenia: Incidence and Pathophysiology
Heparin-induced thrombocytopenia (HIT) is a serious issue for some patients on heparin. It happens when antibodies form against heparin and platelet factor 4 (PF4) complexes. This causes platelet activation and clotting. The chance of HIT changes based on the heparin type and the patient group.
A study in the Journal of Thrombosis and Haemostasis found HIT is more common with unfractionated heparin than low molecular weight heparin.
“Heparin-induced thrombocytopenia is a prothrombotic disorder caused by antibodies that recognize complexes of heparin and platelet factor 4.”
Antibiotics Associated with Immune-Mediated Destruction
Some antibiotics, like vancomycin and sulfonamides, can lead to immune-mediated thrombocytopenia. This happens when drug-dependent antibodies mark platelets for destruction.
- Vancomycin: A glycopeptide antibiotic known to cause immune-mediated thrombocytopenia.
- Sulfonamides: A class of antimicrobials that can induce thrombocytopenia through immune mechanisms.
Chemotherapeutic Agents and Direct Toxicity
Chemotherapy drugs can harm megakaryocytes, the bone marrow cells that make platelets. Drugs like gemcitabine and linezolid are linked to low platelet counts.
- Gemcitabine: A nucleoside analog used in cancer chemotherapy that can cause thrombocytopenia.
- Linezolid: An antibiotic that can cause thrombocytopenia, mainly with long-term use.
Recognition and Management Approaches
Spotting drug-induced thrombocytopenia needs a detailed medical history and lab tests to find the drug causing it. Treatment includes stopping the drug and sometimes using other treatments to help platelet counts.
We suggest a team effort to manage drug-induced thrombocytopenia. This team should include hematologists, pharmacologists, and other healthcare experts for the best care.
Pregnancy-Related and Genetic Causes of Thrombocytopenia
Understanding thrombocytopenia during pregnancy is key. It can range from mild to severe. Low platelet count can come from many pregnancy factors.
Gestational Thrombocytopenia: Prevalence and Outcomes
Gestational thrombocytopenia is common in pregnancy. It usually has a mild effect. About 5-8% of pregnancies are affected.
Key aspects of gestational thrombocytopenia include:
- Mild thrombocytopenia, often with platelet counts above 70,000/μL
- No significant risk to the fetus
- Typically resolves postpartum
HELLP Syndrome and Preeclampsia Mechanisms
HELLP syndrome and preeclampsia are serious pregnancy issues. HELLP syndrome has Hemolysis, Elevated Liver enzymes, and Low Platelet count. The exact causes are not known, but endothelial dysfunction and imbalance in angiogenic factors are thought to be involved.
Inherited Thrombocytopenia Disorders
Inherited thrombocytopenia disorders are caused by genetic mutations. They can vary in severity. Some increase the risk of bleeding, while others have little effect.
Distinguishing Benign from Pathological Causes in Pregnancy
It’s important to tell the difference between mild and serious thrombocytopenia in pregnancy. Clinical features, lab results, and overall health must be considered for an accurate diagnosis.
Factors to consider include:
- Severity of thrombocytopenia
- Presence of other clinical abnormalities
- Gestational age at diagnosis
Conclusion: Diagnostic Approach and Treatment Considerations
It’s key to know why someone has low platelet counts. We’ve talked about many reasons, like immune problems, viruses, and diseases. These can all affect how many platelets are in the blood.
Finding out what’s causing low platelets is the first step. Doctors use a detailed approach. This includes looking at the patient’s history, doing tests, and sometimes taking a bone marrow sample. This helps doctors find the right treatment.
At LivHospital, we focus on treating each patient as an individual. Our hematologists work with patients to create the best treatment plans. We use the newest ways to manage thrombocytopenia. Our goal is to make patients’ lives better and their health improve.
FAQ
What is thrombocytopenia?
Thrombocytopenia is when you have too few platelets in your blood. Platelets help your blood clot. Without enough, you might bleed a lot.
What is a normal platelet count?
A normal count is between 150,000 to 450,000 platelets per microliter. If it’s lower, you might have thrombocytopenia.
What are the signs and symptoms of thrombocytopenia?
You might notice bruising, small red spots on your skin, nosebleeds, or bleeding that won’t stop.
What causes thrombocytopenia?
It can happen for many reasons. This includes making fewer platelets, destroying more, or taking certain medicines.
What is immune thrombocytopenia (ITP)?
ITP is when your immune system attacks your platelets. This makes your platelet count drop.
Can viral infections cause thrombocytopenia?
Yes, some viruses like HIV and hepatitis C can affect your platelets. This can lead to thrombocytopenia.
How does chemotherapy affect platelet count?
Chemotherapy can slow down your bone marrow. This means you make fewer platelets, which can cause thrombocytopenia.
What is the relationship between chronic liver disease and thrombocytopenia?
Liver disease, like cirrhosis, can cause thrombocytopenia. This is because of high blood pressure in the liver and other issues.
Can systemic autoimmune diseases cause thrombocytopenia?
Yes, diseases like lupus and rheumatoid arthritis can lead to thrombocytopenia. They affect how your immune system works.
How do certain medications cause thrombocytopenia?
Some medicines, like heparin, can destroy platelets. This is why they can cause thrombocytopenia.
Can thrombocytopenia occur during pregnancy?
Yes, pregnancy can cause thrombocytopenia. It’s important to know if it’s safe or not.
What is the treatment approach for thrombocytopenia?
Treatment depends on why you have it. It might involve fixing the cause, stopping certain medicines, or helping your body make more platelets.
References
- Hildenbrand, A. K., et al. (2014). A mixed methods assessment of coping with pediatric cancer. Journal of Psychosocial Oncology, 32(4), 400-422. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3929263/










