
A prolapsed bladder, also known as cystocele, happens when the bladder bulges into the vagina. This is because the muscles and tissues around it have weakened. It’s more common in women, and even more so for those who have had children.
About half of women who have had children face some form of pelvic organ prolapse. Mild bladder prolapse affects around 34 percent of women. Knowing the symptoms and treatment options is key to improving your life.
Recognizing the symptoms and looking into treatments can greatly enhance your well-being. We’ll help you understand this, providing useful insights and support along the way.
Key Takeaways
- Prolapsed bladder is a common condition among women, specially after childbirth.
- Understanding symptoms and treatment options is key for effective management.
- Nearly half of women who have given birth experience some degree of pelvic organ prolapse.
- Mild cases of bladder prolapse affect about 34 percent of women.
- Recognizing symptoms and exploring treatments can improve quality of life.
Understanding Prolapsed Bladder
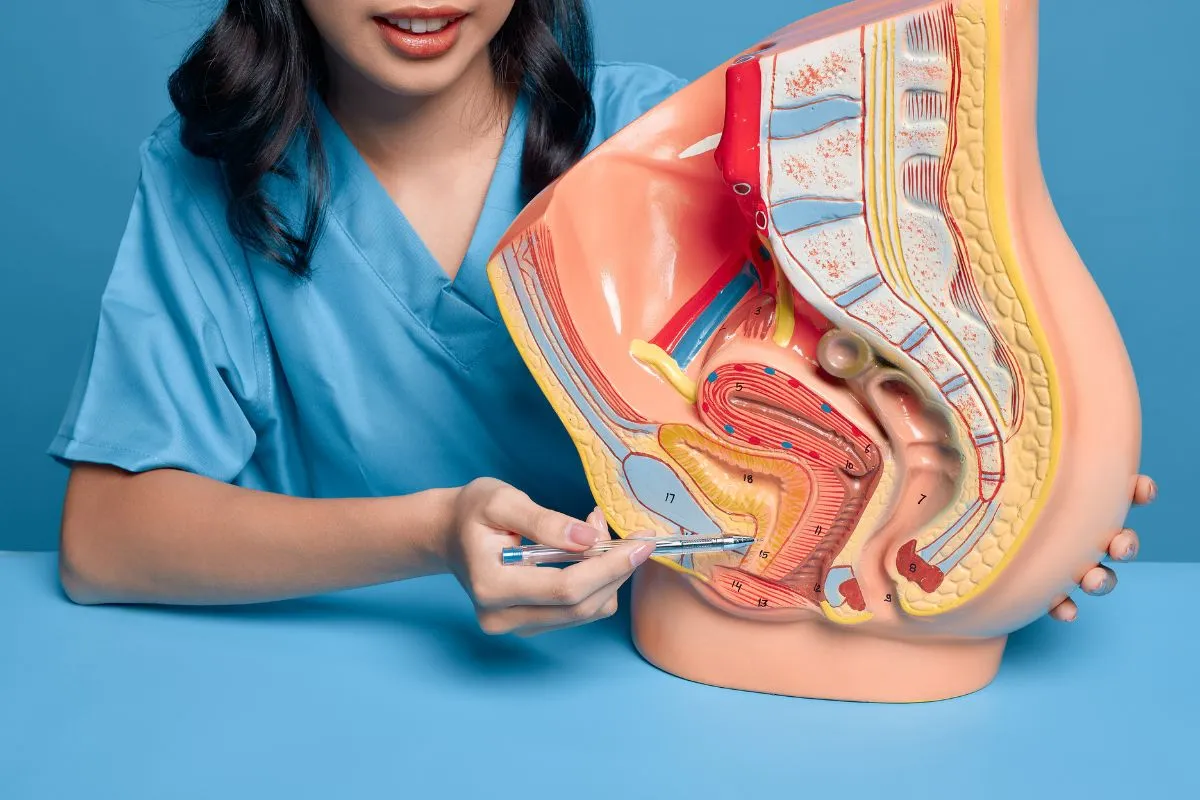
When the wall between a woman’s bladder and her vagina weakens, the bladder may prolapse, or drop, into the vagina. This is called a cystocele. It can happen due to childbirth, age, and hormonal changes.
What is a Cystocele?
A cystocele happens when the tissue between the bladder and vagina stretches or tears. This lets the bladder bulge into the vagina. It’s a type of pelvic organ prolapse and can really affect a woman’s life.
The National Institute of Diabetes and Digestive and Kidney Diseases says it’s a form of pelvic organ prolapse. Knowing about cystocele is key to getting the right treatment and managing symptoms.
Prevalence Among Women
About 34 percent of women have mild bladder prolapse. This shows how common it is, making awareness important, even more so for women who have had children.
Studies show that cystocele gets more common with age, mainly during and after menopause. This is because estrogen levels drop, weakening the pelvic muscles and tissues. This can lead to a prolapsed bladder.
Age Group | Prevalence of Cystocele |
20-39 years | 10% |
40-59 years | 25% |
60 years and older | 40% |
This table shows how cystocele gets more common with age. It highlights the need for awareness and prevention across different age groups.
Common Causes of Bladder Prolapse
Several factors contribute to bladder prolapse, including childbirth and age. Understanding these causes is key for prevention and treatment.
Childbirth-Related Damage
Childbirth is a big risk for bladder prolapse. The Medical organization says pregnancy and childbirth can harm the muscles and tissues that support the bladder. This harm can weaken these structures, leading to prolapse.
Women often feel vaginal heaviness due to childbirth. Pelvic floor damage during delivery is common and can cause long-term problems if not treated.
Age and Hormonal Changes
Aging weakens the muscles and tissues that support the pelvic organs. Hormonal changes, like the drop in estrogen during menopause, make this weakening worse.
Hormonal fluctuations can weaken the pelvic floor muscles, making them more prone to prolapse. Women, during and after menopause, should be aware of these changes and take steps to prevent them.
Chronic Straining and Heavy Lifting
Chronic straining and heavy lifting also cause bladder prolapse. Activities like heavy lifting, straining during bowel movements, or chronic strain put extra pressure on the pelvic floor muscles.
- Heavy lifting at work or during exercise
- Chronic coughing or straining during bowel movements
- Obesity, which increases pressure on the pelvic floor
Understanding these causes helps women take steps to lower their risk of bladder prolapse. Medical professionals say knowing the risk factors is the first step in prevention.
“Preventing pelvic organ prolapse involves addressing modifiable risk factors such as obesity and chronic straining.” — American Urogynecologic Society
By tackling these factors and making lifestyle changes, women can lower their risk of bladder prolapse. It’s important to talk to healthcare providers for personalized advice and treatment options.
What Does a Prolapsed Bladder Feel Like?
Women with a prolapsed bladder often feel a heavy or uncomfortable feeling in their pelvic area. This feeling can change in intensity. It’s often described as a dragging or pulling sensation.
The Sensation of Vaginal Heaviness
Many women describe a prolapsed bladder as feeling like their vagina is heavy. This feeling can be there all the time or come and go. It usually gets worse when standing for a long time or doing physical activities.
Some women feel a fullness or pressure in their vagina. This can be uncomfortable and worrying.
Pelvic Pressure and Discomfort
Women with a prolapsed bladder often feel pelvic pressure and discomfort. This can feel like a dull ache or sharp pain, depending on how bad the prolapse is.
The discomfort can be in the pelvic area or spread to the lower back or thighs. Activities that increase pressure inside the body, like coughing or lifting heavy things, can make it worse.
Bulging Tissue in the Vagina
In severe cases, women may see bulging tissue in their vagina. This can feel like a lump or something sticking out. It can make them feel like something is off.
This bulging tissue can cause a lot of distress. It can affect daily activities and sex life.
Symptom | Description | Impact on Daily Life |
Vaginal Heaviness | Feeling of fullness or pressure in the vagina | Discomfort during standing or physical activities |
Pelvic Pressure | Dull ache or sharp pain in the pelvic area | Discomfort during activities that increase intra-abdominal pressure |
Bulging Tissue | Noticeable lump or protrusion in the vagina | Significant distress, impact on daily activities and sexual function |
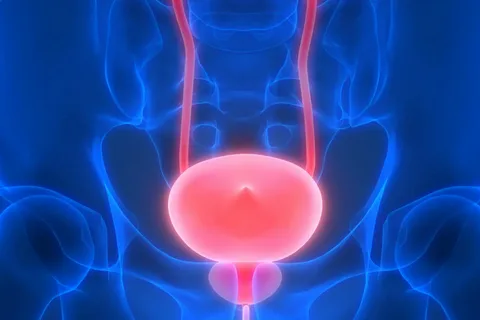
Urinary Symptoms of Prolapsed Bladder
A prolapsed bladder can cause many urinary symptoms that make daily life hard. These symptoms can be mild or severe and affect how well you feel. We will look at common symptoms like trouble emptying the bladder, incontinence, and changes in how often you need to urinate.
Incomplete Bladder Emptying
One big symptom of a prolapsed bladder is feeling like you can’t empty your bladder fully. This happens because the bladder can block the urine flow. It makes it hard to fully empty the bladder.
Symptoms to watch out for:
- Feeling like the bladder is not fully empty after urination
- Need to strain or push to urinate
- Weak or slow urine stream
Stress Incontinence During Activities
Stress incontinence is another common problem with a prolapsed bladder. It’s when you leak urine without meaning to, during activities that put pressure on your belly. This can happen when you cough, sneeze, or lift heavy things.
Frequent Urination Problems
Frequent urination can really disrupt your day. Women with a prolapsed bladder might need to go to the bathroom more often. This can be very inconvenient.
Can a Prolapse Cause Smelly Urine?
A prolapsed bladder can lead to urinary tract infections (UTIs). These infections can make your urine smell bad. UTIs happen when bacteria grow in the urine that stays in the bladder.
Symptom | Description | Possible Complications |
Incomplete Bladder Emptying | Feeling like the bladder is not fully empty after urination | Urinary Tract Infections (UTIs) |
Stress Incontinence | Involuntary leakage of urine during physical activities | Embarrassment, Skin Irritation |
Frequent Urination | Urgency to urinate more often than usual | Disruption of Daily Activities, Sleep Disturbances |
It’s important to know about these symptoms to manage and treat a prolapsed bladder well. By recognizing the signs and getting the right medical care, women can feel better and live better lives.
Additional Symptoms and Complications
A prolapsed bladder can lead to many complications that make daily life hard. These symptoms can really lower a woman’s quality of life. They make simple tasks a big challenge.
Painful Sexual Intercourse
Painful sex is a big problem for women with a prolapsed bladder. The bladder’s displacement can cause pain during sex. This can hurt the physical and emotional bond between partners.
Can Bladder Prolapse Cause Constipation?
Yes, a prolapsed bladder can cause constipation. The pressure on the rectum can slow down bowel movements. This makes it hard to fully empty the bowels, leading to constipation.
Impact on Daily Activities
The symptoms of a prolapsed bladder can really affect daily life. Simple actions like lifting or bending can be painful. The fear of leakage or feeling of vaginal heaviness can also limit physical activities.
It’s important to understand these symptoms to manage the condition well. Knowing how a prolapsed bladder affects a woman’s life helps healthcare providers give better care and support.
Recognizing Prolapse Symptoms After Childbirth
It’s important to know the signs of prolapse after having a baby. This is to get help early and manage the condition well. We’ll look at the signs that show a prolapse might be happening.
Immediate Postpartum Signs
Some women feel symptoms of prolapse right after giving birth. They might feel their vagina is heavy or see a bulge. A healthcare provider says, “This can be very upsetting.” These signs mean you might need to see a doctor right away.
Delayed Symptoms That Develop Over Time
Not all symptoms show up right away. Some women might not notice anything until months or years later. Signs can include feeling pressure in the pelvis, pain during sex, or trouble peeing. It’s key to watch your health and tell your doctor about any odd feelings.
Differences Between Normal Recovery and Prolapse
Telling normal recovery from prolapse symptoms can be hard. Some pain is okay after having a baby, but big bulges or trouble holding urine are not. Knowing the difference helps get help fast.
Spotting prolapse symptoms after childbirth is key for new moms’ health. By knowing the signs and getting medical help, women can manage their symptoms well.
How to Know if You Have a Prolapse
It’s important to know the signs of a prolapsed bladder early. A prolapsed bladder, or cystocele, happens when the bladder bulges into the vagina. This can make daily life harder.
Self-Assessment Techniques
Start by noticing any unusual feelings in your pelvic area. Look for any visible bulges in the vagina and feel for pressure or heaviness. You can check by inserting your fingers into your vagina and coughing or bearing down.
Remember, self-checks are not a full diagnosis. If you think you have a prolapsed bladder, see a doctor for a proper check-up.
When to Seek Medical Attention
See a doctor if you have symptoms like pelvic pressure, trouble emptying your bladder, or a bulge in your vagina. Severe symptoms include urine leaks, painful sex, or trouble walking. A doctor can help figure out the best treatment.
- Pelvic pressure or heaviness
- Difficulty starting to urinate or fully emptying the bladder
- Visible bulge in the vagina
- Urinary incontinence
What to Expect During Diagnosis
Your doctor will do a pelvic exam to check the prolapse’s severity. They’ll look for bulging or displacement of the bladder and check your pelvic health. You might be asked to cough or bear down.
They might also suggest tests like urodynamic tests to check your bladder. Knowing how bad your prolapse is helps find the best treatment.
How to Fix a Prolapsed Bladder: Conservative Treatments
Many women find relief from prolapsed bladder symptoms through non-surgical treatments. These methods can ease symptoms and enhance quality of life. We’ll look at exercises, devices, and lifestyle changes that help.
Pelvic Floor Muscle Exercises
Kegel exercises are key in managing prolapsed bladder symptoms. They strengthen the muscles that support the bladder. This helps reduce the feeling of prolapse.
To do Kegel exercises right:
- Find the right muscles by stopping urine flow mid-stream.
- Contract these muscles for 5-10 seconds, then release for the same time.
- Do this 10-15 times, three times a day.
Regular practice is vital for Kegel exercises to work best. It’s important to identify the pelvic floor muscles correctly to avoid straining other muscles.
Pessaries and Support Devices
Pessaries are devices inserted into the vagina to support the bladder. They come in different shapes and sizes. A healthcare provider can help find the right one for you. Pessaries are great for those who don’t want surgery or can’t have it.
Using pessaries has several benefits:
- They provide immediate relief from symptoms.
- They are non-surgical and can be removed.
- They can be used with other treatments.
It’s important to see a healthcare provider regularly. This ensures the pessary fits well and checks for any problems.
Lifestyle Modifications That Help
Changing your lifestyle can also help with prolapse symptoms. These changes include:
- Keeping a healthy weight to reduce pelvic floor pressure.
- Avoiding heavy lifting and straining.
- Doing gentle exercise to improve pelvic health.
- Managing chronic coughing or constipation, which can make symptoms worse.
By making these changes, many women see a decrease in symptoms and an improvement in their well-being. It’s important to talk to a healthcare provider to find the best treatment for you.
Medical Interventions for Prolapsed Bladder
Medical treatments are key in managing a prolapsed bladder. The right treatment depends on how severe the symptoms are and how much the bladder has prolapsed.
Hormone Replacement Therapy
Hormone replacement therapy (HRT) is often used for women with a prolapsed bladder, mainly during menopause. It helps make vaginal tissues stronger and improves pelvic floor health.
Benefits of HRT:
- Improves vaginal tissue elasticity
- Enhances pelvic floor strength
- Reduces symptoms of prolapse
Medications for Symptom Management
There are medicines to help with symptoms of a prolapsed bladder, like urinary incontinence.
Medication Type | Purpose | Benefits |
Anticholinergics | Reduce bladder muscle contractions | Decreases frequency of urination |
Beta-3 adrenergic agonists | Relax bladder muscle | Increases bladder capacity |
Physical Therapy Approaches
Physical therapy is also a good option for managing a prolapsed bladder. Pelvic floor exercises can greatly help symptoms.
With these medical treatments, women can find relief from a prolapsed bladder’s symptoms. This improves their quality of life.
Surgical Solutions for Fixing Prolapsed Bladder
When other treatments don’t work, surgery is a good option for a prolapsed bladder. It can fix the problem and make you feel better. Surgery aims to fix the pelvic area and ease symptoms.
Transvaginal Repair Procedures
Transvaginal repair fixes the prolapse through the vagina. It’s less invasive than other surgeries and leads to quicker healing. The methods include:
- Anterior colporrhaphy for repairing the vaginal wall
- Use of mesh or grafts to support weakened tissues
Doctors choose the right method based on how bad the prolapse is and your health.
Abdominal Surgical Approaches
For some, an abdominal surgery is better. This can include:
- Sacral colpopexy, where the vagina is suspended from the sacrum using mesh
- Other procedures that involve lifting and securing the prolapsed bladder to a stable structure
Abdominal surgery is often chosen for more severe cases or when a bigger repair is needed.
Minimally Invasive Techniques
Minimally invasive surgeries, like laparoscopy, have small cuts, less pain, and quick healing. They’re becoming more common for fixing prolapsed bladders.
Surgical Approach | Key Benefits | Considerations |
Transvaginal Repair | Less invasive, quicker recovery | May not be suitable for severe prolapse |
Abdominal Surgery | Comprehensive repair, suitable for severe cases | Longer recovery time, more invasive |
Minimally Invasive Techniques | Smaller incisions, less pain, faster recovery | Requires specialized skill, may have higher costs |
A study says, “The choice of surgical technique depends on the patient’s specific condition, the surgeon’s expertise, and the patient’s preferences regarding recovery time and possible complications”
“The goal of surgical treatment is to restore normal anatomy and function while minimizing risks and improving quality of life.”
Preventing Bladder Prolapse and Recurrence
Keeping the pelvic area healthy is key to avoiding bladder prolapse. We’ll look at ways to lower the risk of this condition.
Risk Reduction Strategies
To stop bladder prolapse, knowing and lessening risk factors is important. Keeping a healthy weight is vital, as extra weight strains pelvic muscles. Also, avoid heavy lifting and bending to keep these muscles strong.
Managing chronic coughing and constipation is also important. These can weaken the pelvic floor. By treating these issues, you can lower your risk of bladder prolapse.
Postpartum Care to Prevent Prolapse
Postpartum care is key, mainly for women who gave birth vaginally. Pelvic floor exercises, like Kegels, help strengthen these muscles.
Importance of Pelvic Floor Exercises
Pelvic floor exercises are a simple yet powerful way to keep the pelvic area healthy. They help strengthen the muscles that support the bladder. Start these exercises early after giving birth and keep doing them.
- Do Kegel exercises every day to strengthen pelvic floor muscles.
- Avoid heavy lifting and bending to reduce strain on the pelvic floor.
- Manage chronic coughing and constipation through medical treatment and lifestyle changes.
Long-term Pelvic Health Maintenance
Keeping the pelvic area healthy long-term is essential to avoid bladder prolapse coming back. This means keeping up with pelvic floor exercises, living a healthy lifestyle, and seeing your healthcare provider regularly.
By sticking to these tips, you can greatly lower your risk of bladder prolapse and keep your pelvic area healthy.
Conclusion
Understanding and managing a prolapsed bladder is key to a better life. It involves using both conservative and medical treatments, as well as surgery. This approach helps manage symptoms effectively.
Exercises for the pelvic floor, pessaries, and support devices can help a lot. Making lifestyle changes also plays a big role. Hormone therapy, medications, and physical therapy can offer more relief.
To prevent bladder prolapse, it’s important to keep pelvic health in check. Adopting preventive measures and caring for your body after childbirth are essential. This way, you can lower your risk of prolapse.
We urge everyone to take care of their pelvic health. Seek medical help when needed and use preventive measures. Managing a prolapsed bladder well is vital for a better quality of life and overall health.
FAQ
What does a prolapsed bladder feel like?
A prolapsed bladder can feel like your vagina is heavy or your pelvis is under pressure. You might also notice a bulge or lump in your vagina. The feeling can vary in intensity.
What are the symptoms of prolapse after childbirth?
After childbirth, symptoms of prolapse include feeling your vagina is heavy or your pelvis is under pressure. You might see a bulge in your vagina. You could also have trouble fully emptying your bladder or leak urine when you cough or laugh.
Can a prolapse cause smelly urine?
A prolapse itself might not make your urine smell. But, it can cause you to hold urine or not empty your bladder fully. This can lead to infections, which can make your urine smell bad.
How do I know if I have a prolapse?
To know if you have a prolapse, watch for signs like feeling your vagina is heavy or your pelvis is under pressure. If you notice a bulge in your vagina, see a doctor. They can check if you have a prolapse.
Can bladder prolapse cause constipation?
Yes, a bladder prolapse can make it harder to go to the bathroom. This is because the pressure on your rectum can affect your bowel movements. It’s more common with rectal prolapse, but it can happen with bladder prolapse too.
What are the treatment options for a prolapsed bladder?
Treatment for a prolapsed bladder includes exercises to strengthen your pelvic floor and making lifestyle changes. You might also use pessaries or support devices. Doctors can prescribe hormones, medications, or physical therapy. Sometimes, surgery is needed.
How can I prevent bladder prolapse?
To prevent bladder prolapse, keep your pelvic floor strong with exercises like Kegels. Avoid heavy lifting and manage chronic coughing. Stay at a healthy weight. Good postpartum care and paying attention to your pelvic health during and after pregnancy also help.
Is it normal to feel vaginal heaviness after childbirth?
Some discomfort or pressure in your pelvis after childbirth is normal. But, if you feel persistent or severe vaginal heaviness, it’s not normal. You should talk to your healthcare provider, as it could be a sign of a prolapse.
Can a prolapse cause painful sexual intercourse?
Yes, a prolapse can make sex uncomfortable or painful. This is because the displaced pelvic organs and strained vaginal tissues can cause discomfort.
What is the role of pelvic floor exercises in preventing prolapse?
Pelvic floor exercises, like Kegels, are key in preventing prolapse. They strengthen the muscles that support your pelvic organs. This reduces the risk of prolapse and improves your pelvic health.
References
National Health Service (NHS). Evidence-Based Medical Guidance. Retrieved from https://www.nhs.uk/conditions/pelvic-organ-prolapse/







