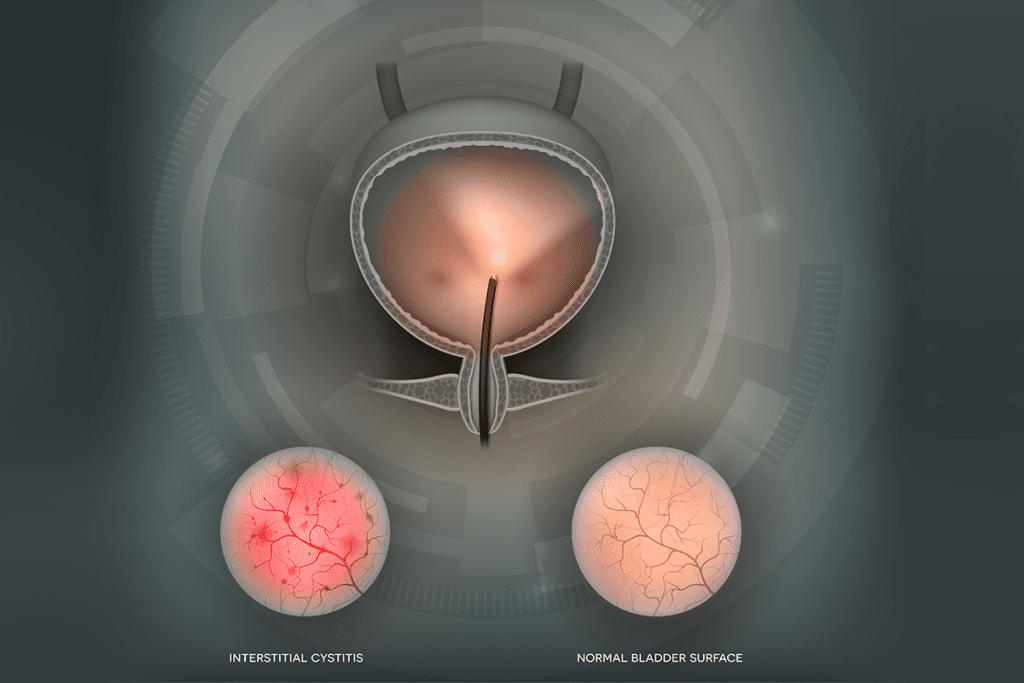
Neurogenic bladder is a condition where the nerves controlling the bladder are damaged. It can greatly affect a person’s quality of life. This chronic condition affects millions worldwide, causing a range of urinary symptoms.
We know that neurogenic bladder includes different types, like hypotonic and hypertonic. Each type has its own characteristics. For example, a hypotonic bladder has a detrusor muscle that is too weak to empty the bladder properly.
Even though it’s a chronic condition, there’s hope for managing symptoms and improving outcomes. New treatments like sacral neuromodulation and robotic-assisted surgery offer new possibilities for patients.
Key Takeaways
- Neurogenic bladder is a chronic condition that affects bladder control.
- Various types of neurogenic bladder exist, including hypotonic and hypertonic variants.
- Symptoms can be managed through lifestyle changes, catheters, and medications.
- Advanced treatments like sacral neuromodulation and robotic-assisted surgery are available.
- Effective management can significantly improve the quality of life.
Understanding Neurogenic Bladder: Causes and Types
It’s important to know about a neurogenic bladder to manage it well. This condition makes it hard to control the bladder. It happens because of problems with the brain, spinal cord, or nerves.
What Causes Neurological Bladder Dysfunction
Neurogenic bladder can be caused by nerve damage. This damage can come from infections, tumors, spinal cord injuries, or diabetes. It can also happen after pelvic surgery or a herniated disk. The damage messes up how the bladder and brain talk to each other, causing bladder problems.
Hypotonic (Flaccid) Neurogenic Bladder
A hypotonic or flaccid neurogenic bladder happens when the bladder muscles lose tone. This is usually because of damage to the sacral spinal cord or nerves. The bladder then can’t empty well, causing urine to stay in the body.
Hypertonic (Reflexive) Neurogenic Bladder
A hypertonic or reflexive neurogenic bladder has overactive bladder muscles. This is often due to damage to the upper motor neurons. It makes the bladder contract too often, leading to urgency and leaks.
Mixed Neurogenic Bladder
Some people have a mixed neurogenic bladder. This is when both upper and lower motor neuron damage happens. It mixes symptoms from both hypotonic and hypertonic neurogenic bladder. Treating a mixed neurogenic bladder is hard because of its complex symptoms.
Knowing the different types of neurogenic bladder helps doctors create the right treatment plan. This plan is made for each person’s specific needs.
Common Symptoms and Diagnosis Methods
Knowing the symptoms and how doctors diagnose neurogenic bladder can really help. This condition affects how we control our bladder, causing different urinary problems.
Primary Symptoms to Recognize
The symptoms of neurogenic bladder depend on the cause and type of bladder issue. Common signs include:
- Urge incontinence: Not being able to hold urine, leading to leaks.
- Obstructive bladder symptoms: Trouble starting to pee or feeling like you’re not emptying your bladder fully.
- Overflow incontinence: Constant leaking of urine because your bladder is too full.
Spotting these symptoms early is key to getting the right treatment.
Urinary Hesitancy and Bladder Spasms
People with neurogenic bladder often face urinary hesitancy and bladder spasms. Hesitancy means trouble starting to pee. Bladder spasms are sudden, unwanted muscle contractions that can cause urgency and pain.
These issues can really affect your life, so getting a diagnosis and treatment quickly is vital.
Diagnostic Tests and Procedures
Doctors use a few methods to diagnose a neurogenic bladder. These include:
| Diagnostic Test | Description |
| Urodynamic Tests | Check how well your bladder holds and empties urine. |
| Ultrasound | Looks at your bladder’s shape and checks for problems like stones or tumors. |
| Electromyography (EMG) | Studies the electrical activity of your bladder muscles to find nerve damage or issues. |
These tests help doctors figure out what’s causing your neurogenic bladder and plan the best treatment.
Understanding Your Diagnosis (ICD-10 Codes)
After finding out you have a neurogenic bladder, you might get an ICD-10 code. The code for this condition is N31.9. Knowing your diagnosis and its code can help you understand your treatment options and insurance.

Is There a Complete Cure for Neurogenic Bladder?
There’s no sure cure for neurogenic bladder yet, but we’re getting better at managing its symptoms. This condition often comes from brain or spinal cord problems. So, treatments are made just for each person.
Current Medical Consensus
Doctors say curing neurogenic bladder is tough, but we can control its symptoms. This makes life better for those affected. They think a mix of medicine, lifestyle changes, and sometimes surgery can really help.
Factors Influencing Treatment Outcomes
Many things affect how well treatments work for a neurogenic bladder. For example, the cause, how bad the symptoms are, and the patient’s health matter a lot. People with spinal cord injuries might have different results than those with multiple sclerosis.
Factors Affecting Treatment Success
- The underlying neurological condition causing the neurogenic bladder
- The severity and duration of symptoms
- The patient’s response to initial treatments
- Presence of any complicating health issues
Realistic Expectations for Symptom Management
Controlling neurogenic bladder symptoms needs a few steps. While a full cure might not be possible, we can reduce symptoms a lot. Patients can see big improvements with the right medicine, lifestyle changes, and sometimes surgery.
It’s key for patients to team up with their doctors to create a treatment plan that fits them best. This way, they can live a better life despite their condition.
Medication Options for Managing Neurological Bladder
Managing a neurogenic bladder needs a full plan, with medicine being key. Medicines can ease symptoms, boost life quality, and stop problems.
Anticholinergics: Tolterodine and Alternatives
Anticholinergics are often used for a neurogenic bladder. Tolterodine relaxes the bladder muscle, cutting down on urgency and frequency. Other options include oxybutynin and trospium chloride.
- Tolterodine reduces urinary frequency and urgency.
- Oxybutynin is good for bladder spasms.
- Trospium chloride helps control bladder symptoms.
Beta-3 Adrenergic Agonists
Beta-3 adrenergic agonists are a new type of medicine for neurogenic bladder. They relax the bladder muscle, increase capacity, and cut down on incontinence. Mirabegron is a beta-3 adrenergic agonist used in treatment.
Mirabegron is effective for neurogenic bladder symptoms. It’s an option for those who don’t do well with anticholinergics.
Solifenacin Succinate and Other Antimuscarinic Agents
Solifenacin succinate is an antimuscarinic agent for neurogenic bladder. It controls bladder contractions, reducing urgency and frequency. Darifenacin and fesoterodine are also used, based on patient response and tolerance.
Combination Therapy Approaches
In some cases, combination therapy is suggested. This means using two or more medicines together for better control. For example, mixing an anticholinergic with a beta-3 adrenergic agonist can work better for some.
It’s vital to talk to a healthcare provider to find the right mix of medicines. Everyone reacts differently to medicines.
Breakthrough Treatments for Hypotonic Neurogenic Bladder
Recent years have brought big changes in treating hypotonic neurogenic bladder. New medical tech and research have led to better treatments. These advancements help improve symptoms and life quality for those affected.
Sacral Neuromodulation Success Rates
Sacral neuromodulation (SNM) is a top treatment for hypotonic neurogenic bladder. It uses electrical stimulation on the sacral nerves to control the bladder. Studies show it greatly improves bladder symptoms in patients.
According to the PMC, SNM boosts the quality of life for many. It works by fixing the neural pathways that control the bladder. This reduces symptoms like urinary retention and incontinence.
The SCONE Device and CONTINENCE Trial Results
The SCONE device is a new implant for sacral neuromodulation therapy. The CONTINENCE trial showed it’s effective for neurogenic bladder. It greatly improves bladder control and reduces symptoms.
The CONTINENCE trial showed the SCONE device could change neurogenic bladder treatment. Its design and neuromodulation make it a promising new option for patients.
Robotic-Assisted Surgical Interventions
Robotic-assisted surgery is now used for many urological issues, including neurogenic bladder. It’s precise and minimally invasive, leading to faster recovery and better results.
It’s used for procedures like bladder augmentation or implanting sacral neuromodulation devices. Robotic systems allow for more accurate and complex surgeries, making treatments more effective.
Emerging Therapies in Clinical Trials
New treatments for neurogenic bladder are being tested in clinical trials. These aim to tackle the root causes and manage symptoms better.
These include new drugs, advanced neuromodulation, and regenerative medicine. As research continues, these therapies could greatly improve treatment options for hypotonic neurogenic bladder patients.
Non-Surgical Management Strategies
For those with a neurogenic bladder, non-surgical methods can greatly improve life quality. These strategies aim to improve bladder control, lessen symptoms, and boost overall health.
Pelvic Floor Physical Therapy
Pelvic floor physical therapy is key for managing neurogenic bladder without surgery. It uses exercises and methods to strengthen the pelvic floor. This helps control the bladder and reduces symptoms.
Benefits of Pelvic Floor Physical Therapy:
- Improved bladder control
- Less frequent incontinence episodes
- Stronger pelvic floor muscles
Intermittent Catheterization Techniques
Intermittent catheterization empties the bladder at set times. It helps manage urine retention and lowers the risk of complications from neurogenic bladder.
Key aspects of intermittent catheterization include:
- Using sterile or clean technique to lower infection risk
- Catheterizing at regular times to avoid overdistension
- Watching urine output to check bladder function
Behavioral Modifications
Behavioral changes are vital in managing a neurogenic bladder. These adjustments help control the bladder and lessen symptoms.
| Behavioral Modification | Description | Benefit |
| Bladder Training | Gradually increasing the interval between voiding | Improved bladder capacity |
| Fluid Management | Regulating fluid intake to manage urine output | Reduced frequency of catheterization |
| Dietary Changes | Avoiding irritants like caffeine and spicy foods | Reduced bladder irritation |
Supportive Devices and Products
Many supportive devices and products help manage a neurogenic bladder. These include catheters, protective garments, and bladder diaries.
Examples of Supportive Devices:
- Hydrophilic catheters for easier insertion
- Protective undergarments for managing incontinence
- Bladder diaries for tracking symptoms and progress
Living with Neurogenic Bladder: Quality of Life Considerations
Neurogenic bladder affects more than just the body. It can change how you feel about life. Finding ways to manage it well is key to a good life.
Managing Detrusor Muscle Dysfunction
The detrusor muscle is very important for bladder health. Problems with this muscle can cause many urinary issues. We will look at ways to handle these issues.
Medicine is one way to manage detrusor muscle problems. Anticholinergic and beta-3 adrenergic agonists are often used. They help with symptoms like needing to urinate too often.
- Anticholinergics: Effective in reducing urinary urgency and frequency.
- Beta-3 adrenergic agonists: Help in relaxing the detrusor muscle, improving bladder capacity.
Preventing Complications and Infections
Neurogenic bladder can cause serious problems like UTIs and kidney damage. It’s important to prevent these issues.
Using an intermittent catheter is a good way to manage a neurogenic bladder. It helps empty the bladder fully, lowering UTI risk.
| Preventive Measure | Benefit |
| Intermittent Catheterization | Reduces risk of UTIs and kidney damage |
| Fluid Management | Helps in maintaining optimal bladder volume |
| Regular Follow-Ups | Ensures timely detection of possible complications |
Psychological Impact and Coping Strategies
Neurogenic bladder can also affect your mind. Many people feel anxious, depressed, or stressed.
Using cognitive-behavioral therapy (CBT) and joining support groups can help. These tools help deal with the emotional side of the condition.
Support groups are great for sharing experiences and learning from others. They offer a sense of community and understanding.
Resources and Support Groups
Having access to resources and support groups is very important. They provide emotional support and practical tips for managing the condition.
Groups like the National Kidney Foundation and the Interstitial Cystitis Association are great resources. They offer support and advice for patients.
Conclusion: The Future of Neurogenic Bladder Treatment
The future of treating neurogenic bladder is looking bright. New discoveries in sacral neuromodulation and robotic surgery are making treatments better. These advancements are leading to more tailored and effective care plans.
Today, we focus on managing symptoms and improving life quality for those with neurogenic bladder. New therapies in trials promise fresh ways to treat this condition. We expect to see a mix of new and old treatments, like sacral neuromodulation and pelvic floor therapy.
We’re excited about the ongoing research and its promise for better treatments. Our aim is to offer the most effective and caring care to our patients. By keeping up with the latest in neurogenic bladder treatment, we hope to improve outcomes for everyone.
FAQ
What is a neurogenic bladder?
Neurogenic bladder is a condition where a person has trouble with bladder control. This trouble comes from a brain, spinal cord, or nerve problem.
What are the different types of neurogenic bladder?
There are three main types: hypotonic (flaccid), hypertonic (reflexive), and mixed neurogenic bladder. Each type has its own characteristics and effects on health.
What are the primary symptoms of neurogenic bladder?
The main symptoms include urinary hesitancy and bladder spasms. These symptoms can greatly affect a person’s quality of life.
How is a neurogenic bladder diagnosed?
Doctors use tests and procedures like urodynamic studies to diagnose neurogenic bladder. These help figure out the cause of symptoms.
Can a neurogenic bladder be cured?
While a complete cure is rare, new treatments offer better symptom management. This improves a person’s quality of life.
What medications are used to manage neurogenic bladder symptoms?
Doctors use anticholinergics like tolterodine and beta-3 adrenergic agonists. Solifenacin succinate is also used. These are often combined for better results.
What is sacral neuromodulation, and how does it help?
Sacral neuromodulation stimulates the sacral nerves to improve bladder control. It shows great promise in treating hypotonic neurogenic bladder.
How can pelvic floor physical therapy help with a neurogenic bladder?
Pelvic floor physical therapy strengthens muscles that support bladder control. This can improve symptoms and urinary health.
What is intermittent catheterization, and why is it used?
Intermittent catheterization drains the bladder at set times. It helps prevent complications and manage symptoms of neurogenic bladder.
How can I manage detrusor muscle dysfunction?
Managing detrusor muscle dysfunction requires a mix of medications, lifestyle changes, and treatments. Each approach is tailored to the individual’s needs.
What are the benefits of behavioral modifications for neurogenic bladder?
Behavioral changes like timed voiding and fluid management can improve bladder control. They can also reduce symptoms.
Where can I find resources and support groups for living with a neurogenic bladder?
Many organizations and online platforms offer resources and support groups. They provide valuable information and a community for those with a neurogenic bladder.
References
- Akpala, A., Lezama, T., Jinadu, K., Belal, M., & King, T. (2024). A five-year retrospective study on the clinical outcomes of sacral nerve stimulation therapy for refractory functional bladder abnormalities. PMC. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC11645166/
- Topoliova, K., Harsanyi, S., Danisovic, L., & Ziaran, S. (2023). Tissue Engineering and Stem Cell Therapy in Neurogenic Bladder Dysfunction: Current and Future Perspectives. Medicina, 59(8), 1416. Retrieved from https://www.mdpi.com/1648-9144/59/8/1416