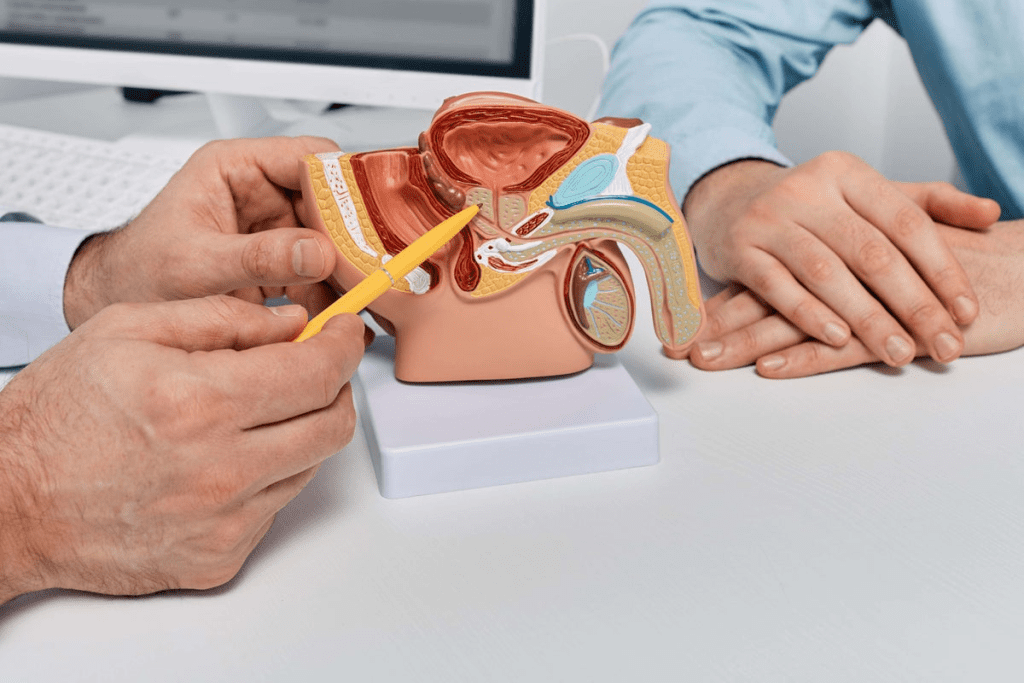
Doctors use a detailed approach to diagnose Peyronie’s disease. This starts with a deep look into your medical history and a physical check-up. We will dive into the methods doctors employ to detect this condition.
Doctors mainly diagnose Peyronie’s disease by reviewing your medical history and doing a physical exam. They can often tell if you have it by examining you physically.
distorted image’
It’s important for patients to understand how doctors diagnose Peyronie’s disease. By explaining the different tests, we hope to clear up how this condition is identified.
Key Takeaways
- Diagnosing Peyronie’s disease involves a thorough medical history and physical examination.
- A physical exam is key in spotting the condition.
- Knowing the diagnostic steps helps patients choose the right treatment.
- Many tests are used to check for Peyronie’s disease.
- Accurate diagnosis is essential for managing the condition.
What is Peyronie’s Disease and Why Testing Matters
At Liv Hospital, we use the latest methods and care from around the world. Peyronie’s disease is when scar tissue forms under the penis skin. This can make the penis curve or bend, causing pain and affecting sex.

distorted image’
Definition and Common Symptoms
Peyronie’s disease is when scar tissue forms under the penis skin. This can make the penis curve or bend. It can also cause pain during erections and make sex hard.
- Penile pain or discomfort
- Curvature or bending of the penis
- Difficulty with sexual intercourse due to pain or curvature
These symptoms can really affect a man’s life. Getting a proper diagnosis is key to find the right treatment.
Importance of Proper Diagnosis
Diagnosing Peyronie’s disease right is very important. We look at your medical history and do a physical check. This helps us know how bad the condition is and how to treat it.
Using advanced tests helps us give care that fits you. We treat not just the physical symptoms but also the emotional ones. Accurate diagnosis lets us offer treatments like Peyronie’s disease treatment. This can include medicine, therapy, or surgery, based on how bad it is.
Comprehensive Medical History Assessment
When diagnosing Peyronie’s disease, understanding a patient’s medical history is key. This step is essential in identifying the condition and its effects on the patient.
We start by asking questions about the patient’s medical background. These questions help us find any factors that might be causing the condition.
Key Questions Doctors Ask
During the medical history assessment, we ask several important questions. These questions help us understand the onset and progression of symptoms. They include:
- When did you first notice the symptoms of Peyronie’s disease?
- Have you experienced any pain or discomfort during erections?
- Is there a history of penile trauma or injury?
- Have you noticed any changes in the curvature or shape of your penis?
- How has Peyronie’s disease affected your erectile function?
These questions help us grasp the patient’s condition and its progression over time.
Documenting Symptom Progression
Tracking the progression of symptoms is vital. It helps us understand the severity of Peyronie’s disease and its impact on the patient’s life. We monitor changes in symptoms, including any increases in curvature or pain during erections.
By understanding the patient’s symptom progression, we can choose the best treatment options. This information is also key for tracking the success of any treatments.

Our aim is to fully understand the patient’s condition. This enables us to offer effective care for Peyronie’s disease. By combining a detailed medical history with other diagnostic tools, we create a personalized treatment plan. This plan addresses the patient’s specific needs.
Physical Examination Techniques for Peyronie’s Disease
Physical exams are key in diagnosing Peyronie’s disease. They give doctors insights into how severe the condition is. These exams help find out how big and curved the penis is.
Palpation of Penile Plaques
A urologist can feel plaques in the penis during an exam. Palpation involves gently feeling the penis to identify scar tissue, which is a hallmark of Peyronie’s disease. This helps doctors know the size, location, and how tender the plaques are.
“The palpation of penile plaques is a vital step in diagnosing Peyronie’s disease,” medical experts highlight. It helps doctors get a clear picture of how severe the condition is.
Measuring Curvature and Deformity
Measuring the penis’s curve and shape is also important. This assessment can be done visually or through the use of specialized tools that measure the degree of curvature. Knowing how curved the penis is helps decide the best treatment.
Erection Assessment Methods
In some cases, a medicine is injected to make an erection. This procedure provides valuable information about the extent of penile curvature and deformity during an erection. It helps in diagnosing and planning treatment.
Using erection assessment methods, like induced erections, helps doctors understand the condition better. This helps them create an effective treatment plan.
Advanced Imaging Tests
Healthcare providers use advanced imaging tests to understand Peyronie’s Disease. These tests help confirm the diagnosis and assess the condition’s severity.
High-Resolution Ultrasound Procedure
High-resolution ultrasound is the top choice for seeing penile plaques and calcifications in Peyronie’s Disease. This non-invasive test uses sound waves to create detailed images of the soft tissues inside the penis. Doctors can then measure the size and location of plaques accurately.
A technician or doctor applies gel to the penis during the procedure. They use a transducer to capture images. The high-resolution images help doctors plan the best treatment.
MRI for Complex Peyronie’s Cases
In complex cases of Peyronie’s Disease, Magnetic Resonance Imaging (MRI) might be suggested. MRI gives detailed images of the penile anatomy. It helps identify the extent of fibrosis and plaque formation.
MRI is key when there’s a suspicion of more extensive tissue damage or when surgery is considered. It provides a detailed view that helps in surgical planning.
Interpreting Imaging Results
Interpreting imaging test results needs expertise in urology and radiology. Specialists analyze the images to assess the size, location, and characteristics of penile plaques. They also look at any associated curvature or deformity.
The information from these tests is critical for creating an effective treatment plan. By understanding the extent and nature of Peyronie’s Disease, healthcare providers can offer the best care.
Laboratory Blood Tests and Analysis
Laboratory blood tests are key in diagnosing and managing Peyronie’s disease. They don’t directly diagnose Peyronie’s but help find related health issues. These issues might be causing or affecting the disease.
We screen for conditions linked to Peyronie’s with blood tests. For example, diabetes is often connected to Peyronie’s. Blood glucose tests can spot undiagnosed diabetes or check current diabetes care. We also test for hypogonadism, a condition that can impact sexual health and Peyronie’s.
Screening for Related Conditions
Screening for related conditions is a big part of our diagnosis. Finding conditions like diabetes or vascular disease helps us understand Peyronie’s better. This info is key for a treatment plan that tackles Peyronie’s symptoms and possible causes.
Some important tests we use are:
- Blood glucose tests to check for diabetes
- Lipid profiles to assess cardiovascular health
- Hormone level tests to evaluate for hypogonadism or other endocrine disorders
Hormonal and Metabolic Evaluations
Hormonal and metabolic tests give us insights into a patient’s health and Peyronie’s factors. They help us see hormone and metabolic imbalances that might be causing the disease. This info is vital for making a treatment plan that fits the patient’s needs.
For instance, hormonal tests can show if low testosterone is a problem. This might be linked to or worsen Peyronie’s disease. Metabolic tests can reveal issues like insulin resistance or high cholesterol. These are important for heart health and can affect Peyronie’s treatment.
Understanding Peyronie’s Disease Demographics
Knowing the demographics of Peyronie’s disease is key. It helps us spot risk factors and see how common it is in different age groups. This info is important for understanding the condition and its effects on people.
Prevalence Rates Across Different Populations
Studies worldwide show Peyronie’s disease affects 0.3% to 20% of men. In the U.S., about 1 in 100 men over 18 have it. This wide range shows how tricky it is to diagnose and report this condition.
Prevalence rates vary a lot across different groups. For example, men with diabetes or past penile injuries are more likely to get Peyronie’s disease. TheNational Institute of Diabetes and Digestive and Kidney says knowing these risks is key for early treatment.
Age Distribution and Risk Factor Assessment
Peyronie’s disease is most common in men aged 50-59. As men get older, the chance of getting Peyronie’s disease goes up. Studies link age to how severe the symptoms are.
Risk factors are big in Peyronie’s disease. These include past penile injuries, diabetes, and genetics. “The exact cause of Peyronie’s disease is unknown,” but it’s thought to be from genes, environment, and lifestyle, says medical research. Knowing these risks helps in making treatment plans and maybe even fixing the penis curve at home.
- Age: The condition is most prevalent in men aged 50-59.
- Medical History: Conditions like diabetes increase the risk.
- Penile Trauma: A history of penile injury is a significant risk factor.
- Genetic Predisposition: Family history may play a role in the development of Peyronie’s disease.
By grasping the demographics of Peyronie’s disease, we can tackle diagnosis and treatment better. This info is vital for doctors and patients to make smart care choices.
Conclusion: What to Expect During Your Diagnostic Journey
Diagnosing Peyronie’s disease is a detailed process. It includes looking at your medical history, a physical exam, and imaging tests. Knowing what to expect can help you make better choices about your treatment.
Liv Hospital’s personnel aims to give top-notch care to those with Peyronie’s disease. We use the newest methods in diagnosis and treatment to help you get the best results. The treatment you need depends on how bad your symptoms are and the stage of the disease. We’re here to help you find the best treatment for you.
Choosing Liv Hospital means you’re in safe hands during your diagnosis. We’re committed to providing world-class healthcare. We also offer full support for international patients, making sure you get the care and support you need to manage Peyronie’s disease well.
FAQ
What is Peyronie’s disease?
Peyronie’s disease is a condition where scar tissue forms under the penis skin. This leads to bending or curvature. Symptoms include pain during erections, penile bending, and trouble with sex.
How is Peyronie’s disease diagnosed?
Doctors use a detailed approach to diagnose Peyronie’s disease. They start with a medical history and physical exam. Then, they use high-resolution ultrasound and MRI for imaging. Blood tests also help check for related conditions.
What happens during a medical history assessment for Peyronie’s disease?
Doctors ask important questions during a medical history assessment. They want to know when symptoms started, how they’ve changed, and if there’s been any penile injury.
What is the role of physical examination in diagnosing Peyronie’s disease?
Physical exams are key in diagnosing Peyronie’s disease. Doctors check for plaques, measure curvature, and assess erections. This helps them understand the disease’s severity.
What imaging tests are used to diagnose Peyronie’s disease?
High-resolution ultrasound is the top choice for seeing plaques and calcifications. MRI might be used in complex cases for more details.
Why are laboratory blood tests necessary for Peyronie’s disease diagnosis?
Blood tests help find related conditions like diabetes or hormonal imbalances. They also give insights into the patient’s overall health.
What are the risk factors for developing Peyronie’s disease?
Risk factors include penile trauma, diabetes, and genetic predispositions. The disease is most common in men aged 50-59.
How can I prepare for a diagnostic test for Peyronie’s disease?
To prepare, discuss your medical history, symptoms, and any past treatments or conditions. This helps doctors understand your situation better.
What treatment options are available for Peyronie’s disease?
Treatment depends on the disease’s severity. Options include medications, injections, or surgery. It’s best to talk to a healthcare provider to find the right treatment.
Can Peyronie’s disease be cured?
There’s no guaranteed cure, but treatments can help manage symptoms. Working with a healthcare provider is key to finding effective treatments.
References
- Kim, D. S., et al. (2025). Diagnosis and management of Peyronie’s disease. World Journal of Men’s Health. Advance online publication.World Journal of Men’s Health
- Howell, S., et al. (2025). Current insights and future directions in Peyronie’s disease. Urology Practice, [volume(issue)], pages.Wiley Online Library
- Paulis, G., De Giorgio, G., & Paulis, A. (2024). Clinical presentation of Peyronie’s Disease: A retrospective study of 564 cases. Diagnostics, 14(11), 1125.MDPI



































