
Rheumatoid arthritis (RA) is a chronic autoimmune condition that affects millions worldwide. It causes pain, swelling, and stiffness in the joints. Knowing how the disease progresses is key to managing it effectively. Comprehensive guide detailing the four stages of ra (Rheumatoid Arthritis) and their corresponding treatment goals.
Rheumatoid arthritis progresses through four distinct stages. These stages range from early inflammation to severe joint damage. Catching it early and acting fast can slow down the disease. This helps keep your joints working well and improves your quality of life.
At Liv Hospital, we offer top-notch rheumatology care. We focus on you, guiding you through every stage of RA.

Rheumatoid arthritis (RA) is a unique challenge in medicine. It requires us to understand its causes and how it works. RA happens when the immune system attacks the lining of the joints, called the synovium. This leads to inflammation, pain, swelling, and can damage the joints over time.
The exact cause of RA is not fully known. But, it’s believed to be a mix of genetics and environment. Genetic predisposition is a big factor, with some genes making you more likely to get RA. Things like smoking and infections can also trigger it in people who are already at risk. Knowing these causes helps us find ways to prevent and treat RA.
RA is different from other arthritis types like osteoarthritis (OA) and gout. RA is an autoimmune disease that can affect many joints at once. It often comes with other symptoms too. Tests for rheumatoid factor and anti-CCP antibodies can help tell RA apart from other arthritis. This is important for getting the right treatment.
Rheumatoid arthritis (RA) is a complex disease that affects more than just the joints. It moves through different stages, impacting various body systems. Knowing how RA progresses is key to managing it well.
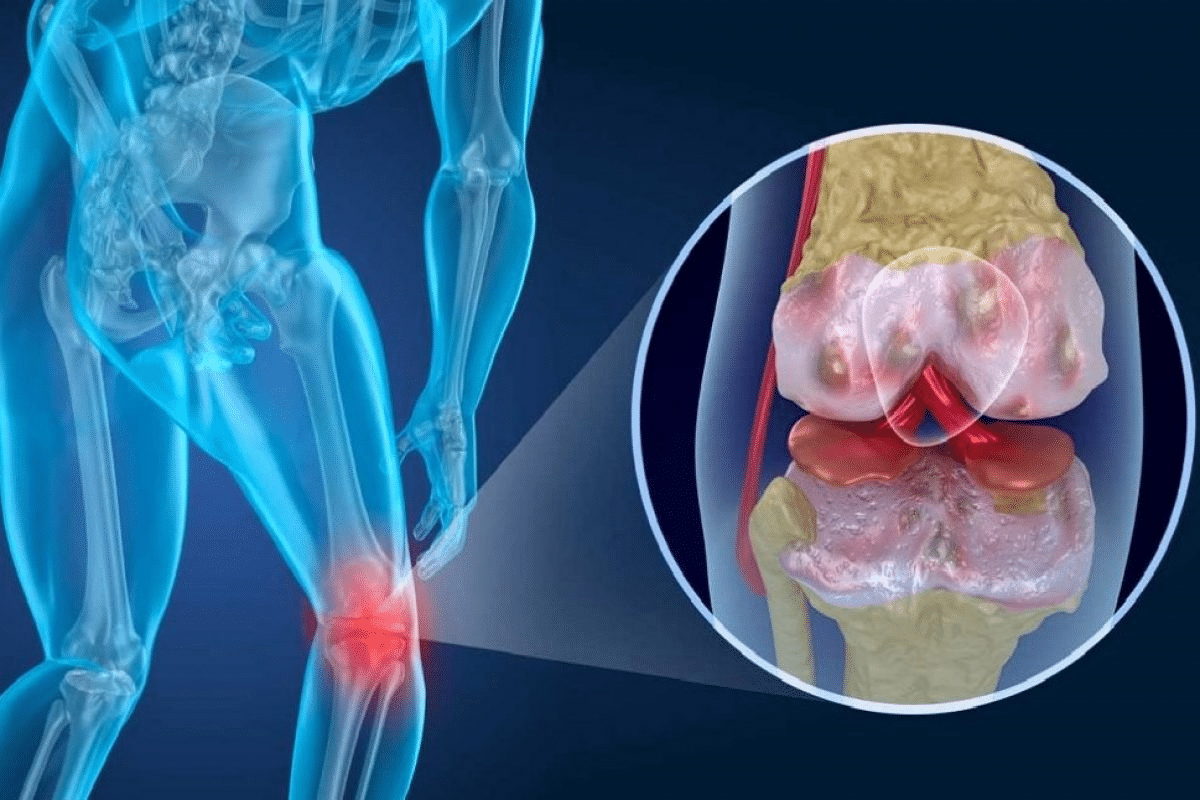
The start of RA involves an autoimmune response that mainly hits the synovium, the joint lining. This leads to swelling, making the synovium thicker and causing damage to the cartilage and bone around it.
The immune system in RA creates inflammatory cytokines and activates immune cells like T cells and B cells. These cells are vital in keeping the inflammation and joint harm going in RA.
RA’s effects aren’t just in the joints. It can also impact other parts of the body, like the lungs, heart, and eyes. This widespread inflammation is a big part of RA’s impact.
For example, RA can cause rheumatoid nodules in the lungs or lead to heart disease because of ongoing inflammation. It’s important to understand these effects to give RA patients the best care.
|
Systemic Effects |
Description |
|---|---|
|
Rheumatoid Nodules |
Formation of nodules in organs such as the lungs |
|
Cardiovascular Disease |
Increased risk due to chronic inflammation |
|
Ocular Manifestations |
Inflammation affecting the eyes |
The four stages of rheumatoid arthritis show how the disease gets worse over time. It starts with early symptoms and ends with serious joint damage. Knowing these stages is key to managing the disease well and helping patients.
Rheumatoid arthritis gets worse if not treated right. It starts with inflammation and damage to joints. Then, it gets more painful and stiff.
It can even lead to deformities and loss of function. Early treatment is vital to slow it down and control symptoms.
Getting a diagnosis and starting treatment early is very important. It helps avoid long-term damage. The benefits are:
Understanding the 4 stages of rheumatoid arthritis helps doctors give better care. This leads to better results for patients.
Rheumatoid arthritis often starts with mild symptoms in the small joints of the hands and feet. These early signs might not seem like much at first. We’ll look at what these symptoms are and how hard it can be to figure out if you have RA.
Early RA can cause morning stiffness, swelling, and pain in fingers and wrists. These signs can be easy to miss because they’re not always obvious. The stiffness lasts more than an hour and can make you feel tired.
People might notice their fingers look swollen or are redder than usual. Wrists can hurt, making it hard to do everyday tasks that need gripping or twisting.
The feet and ankle joints are also affected early in RA. Morning pain or stiffness in the toes is common. Walking or standing can be painful because of the soles of the feet.
Swelling around the ankles is another symptom. This swelling can be warm and red, showing inflammation.
Diagnosing RA in stage 1 is tricky because symptoms are mild and can look like other conditions. X-rays might not show damage yet, making diagnosis hard.
We use a mix of clinical checks, patient history, and blood tests to confirm RA. Tests for rheumatoid factor and anti-CCP antibodies are key.
The table below shows symptoms and challenges in diagnosing stage 1 RA:
|
Symptoms |
Commonly Affected Areas |
Diagnostic Challenges |
|---|---|---|
|
Morning stiffness, swelling, pain |
Fingers, wrists, toes, ankles |
Mild symptoms, similar to other conditions |
|
Redness, warmth, fatigue |
Hands, feet |
Limited damage visible on X-rays |
|
Difficulty performing daily activities |
Wrists, hands, feet |
Need for a full clinical check |
RA advancing to Stage 2 brings significant changes that affect a patient’s life. At this point, symptoms worsen, impacting daily life more.
In Stage 2, rheumatoid factor (RF) and other autoantibodies appear in the blood. Rheumatoid factor is an antibody found in RA patients. Its presence aids in diagnosing RA. These antibodies show an active autoimmune fight.
Patients in this stage often test positive for RF. This is a key sign of RA.
Stage 2 RA affects larger joints, not just small ones. Pain, stiffness, and swelling hit wrists, knees, ankles, and elbows. This makes moving and doing daily tasks harder.
Early treatment can help manage symptoms and slow disease progress.
Cartilage damage is a key feature of Stage 2 RA. The autoimmune fight causes inflammation, damaging cartilage. This can lead to joint narrowing and bone-on-bone contact, causing pain and loss of function.
Cartilage damage can’t be reversed. It’s vital to manage RA well to stop further damage.
Stage 3 rheumatoid arthritis is very severe. It causes a lot of inflammation and damage to bones and cartilage. This stage has a big impact on a person’s life, making symptoms worse.
In Stage 3 RA, inflammation damages cartilage and bone a lot. This damage leads to pain, swelling, and less mobility. It also makes the body produce harmful substances that worsen the condition.
Key effects of inflammation on bone and cartilage include:
Rheumatoid nodules are common in Stage 3 RA. They are firm lumps under the skin, near joints. They are not painful but can be ugly. They also show how severe the disease is.
The inflammation and damage can cause physical deformities. For example, hands can bend in an unusual way. These changes make managing RA harder, affecting both looks and function.
|
Characteristics |
Impact on Patients |
|---|---|
|
Rheumatoid Nodules |
Unsightly lumps under the skin, potentially indicating severe disease |
|
Physical Deformities |
Joint deformities affecting functionality and appearance |
Stage 3 RA makes moving around very hard. The damage and inflammation cause a lot of pain and stiffness. It’s hard to do simple things.
Pain management strategies may include:
End-stage rheumatoid arthritis, or Stage 4 RA, is a serious condition. It causes a lot of joint damage and makes it hard to move. This stage greatly affects a person’s quality of life.
In Stage 4 RA, joints often fuse together. This means bones in the joint grow together, leading to less mobility and flexibility. Such fusion can cause significant deformities and disabilities, making simple tasks hard.
Key implications of joint fusion include:
Thanks to better treatments, Stage 4 RA is happening less often. Early diagnosis and aggressive treatment have helped slow down the disease. This means fewer people are reaching this advanced stage.
Modern treatment approaches have transformed the management of RA, giving patients new hope by potentially preventing Stage 4.
For those with Stage 4 RA, keeping a good quality of life is key. This involves managing pain, adapting to physical limitations, and sometimes surgery to improve joint function or reduce pain. Support from healthcare providers, family, and support groups is vital in coping with end-stage RA.
Strategies to enhance quality of life include:
Diagnosing RA needs a detailed plan that uses several important tools. Finding out if someone has rheumatoid arthritis (RA) is complex. It involves checking for the disease’s signs and how far it has spread.
Blood tests are key in spotting RA. They look for specific signs in the blood that show the disease.
These tests are vital for confirming RA and seeing how active the disease is.
Imaging tests are important for checking joint damage and how the disease is progressing.
|
Imaging Technique |
Use in RA Diagnosis |
|---|---|
|
X-rays |
Look at joint damage and bone erosion. |
|
MRI |
Shows detailed images of joints and soft tissues, spotting early RA signs. |
|
Ultrasound |
Checks for joint inflammation and early damage. |
A detailed physical check is key for seeing how much the joints are involved and how active the disease is. Doctors look at symptoms like joint tenderness, swelling, and stiffness to figure out how severe RA is.
By using all these methods together, doctors can accurately diagnose RA. They can then create a treatment plan that fits the patient’s needs.
RA’s progression requires a treatment plan that changes with the disease. It’s important to know how to use different treatments at each stage of RA.
Medications are key in managing RA. Disease-Modifying Antirheumatic Drugs (DMARDs) are the main treatment. Drugs like methotrexate slow down the disease and protect joints and other body parts from damage.
Biologics target specific parts of the immune system that cause inflammation and damage. Examples include etanercept and adalimumab. Targeted therapies, like tofacitinib, work differently to control the immune system.
|
Medication Type |
Examples |
Primary Use in RA |
|---|---|---|
|
Conventional DMARDs |
Methotrexate, Hydroxychloroquine |
Slow disease progression, reduce joint damage |
|
Biologic DMARDs |
Etanercept, Adalimumab |
Target specific proteins involved in inflammation |
|
Targeted Therapies |
Tofacitinib |
Modulate the immune system’s response |
Physical and occupational therapy are key in managing RA. They help keep joints moving and working well. Physical therapy improves flexibility and strength. Occupational therapy helps adapt daily activities to physical limitations.
In advanced RA, surgery may be needed to fix or replace damaged joints. Surgical options include removing inflamed tissue, repairing tendons, fusing joints, and replacing joints entirely.
Using these treatments at the right time can greatly improve RA outcomes. It helps patients live better and more active lives.
Early and effective treatment is key to stopping Rheumatoid Arthritis from getting worse. Starting treatment early can greatly reduce the risk of lasting damage and disability. It’s vital to get medical help quickly to manage RA well.
Studies show there’s a window of opportunity to treat RA. This is when starting therapy can lead to better results. It’s usually in the first few months after symptoms appear.
Prompt diagnosis and treatment during this time can greatly help. It can lead to less inflammation and slower disease progress.
Early treatment aims to prevent joint damage and disability. Starting treatment early can lower the risk of severe joint damage. This is a big problem in advanced RA.
It improves patients’ quality of life and cuts down on the need for expensive treatments later.
Effective early treatment includes medicines like DMARDs and biologics. It also includes physical therapy and changes in lifestyle. These steps together can greatly improve RA patients’ outcomes.
Managing rheumatoid arthritis means making big changes in your life. We’ll look at how to adapt your lifestyle to live better with RA. This includes diet, exercise, using assistive devices, and taking care of your mental health.
Eating the right foods can help control RA symptoms. Foods like salmon and sardines are good because they have omega-3 fatty acids. Also, eating fruits, vegetables, and whole grains can help fight inflammation.
Exercise is also key in managing RA. Gentle activities like yoga, swimming, and cycling help keep your joints moving. Always talk to your doctor before starting any new exercise plan.
Using assistive devices can make everyday tasks easier for people with RA. Tools like jar openers and walking aids can help. Also, making your home safer and more accessible can be very helpful.
RA can affect your mental health. It’s important to take care of your emotional well-being. Seek help from doctors, support groups, and friends. Stress-reducing activities like meditation can also help.
“The psychological impact of chronic illness should not be underestimated. Supporting mental health is as important as managing physical symptoms.”
By making these lifestyle changes, people with RA can manage their condition better. This can improve their overall quality of life.
Managing rheumatoid arthritis is a journey that needs ongoing support and treatment changes. Understanding the stages of RA and the treatments available helps patients navigate their condition better. This improves their quality of life.
RA goes through four stages, each with its own challenges. Early diagnosis and treatment are key to preventing joint damage and disability. A good treatment plan, including medicines, physical therapy, and lifestyle changes, can help manage symptoms and slow the disease.
We stress the need for a team effort in managing RA. Patients, healthcare providers, and support systems must work together. This way, people with RA can stay independent, reduce pain, and improve their overall well-being at every stage of their condition.
The 4 stages of rheumatoid arthritis are: Stage 1: Early Rheumatoid Arthritis, Stage 2: Moderate Rheumatoid Arthritis, Stage 3: Severe Rheumatoid Arthritis, and Stage 4: End-Stage Rheumatoid Arthritis.
Rheumatoid arthritis starts with an autoimmune response. This causes inflammation in the joints. It leads to damage in cartilage and bone. Eventually, it can cause joints to fuse and result in loss of function.
Stage 1 rheumatoid arthritis symptoms start in fingers and wrists. They also appear in feet and ankle joints. It’s hard to diagnose because it looks like other types of arthritis.
Doctors use blood tests and biomarkers to diagnose rheumatoid arthritis. They also use imaging like X-rays, MRI, and ultrasound. Physical exams and symptom checks are part of the diagnosis too.
Treatments include medications like DMARDs, biologics, and targeted therapies. Physical and occupational therapy are also options. For advanced stages, surgery might be considered.
Early treatment is key because it can stop joint damage and disability. It gives a chance to manage the disease before it gets worse.
Making lifestyle changes helps manage rheumatoid arthritis. This includes following a healthy diet and exercising. Using assistive devices and making home modifications also helps. Supporting mental health and emotional well-being is important too.
Rheumatoid arthritis can greatly affect quality of life, mainly in advanced stages. It causes joint fusion, loss of function, and mobility issues.
There’s no cure for rheumatoid arthritis. But, modern treatments can manage the disease and prevent joint damage.
Rheumatoid arthritis is an autoimmune disease. It’s different from other arthritis types like osteoarthritis because of its causes and how it progresses.
Rheumatoid nodules are a complication of rheumatoid arthritis. They are firm lumps under the skin, often near affected joints.
National Center for Biotechnology Information. Rheumatoid Arthritis Pain Relief: Treatments and Disease Management. Retrieved from https://pubmed.ncbi.nlm.nih.gov/26545940/
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!