
Explaining the triggers of a rheumatoid arthritis flare up and describing the common systemic and joint symptoms.
At Liv Hospital, we know that rheumatoid arthritis (RA) flare-ups are very tough. They cause a lot of pain, swelling, and stiffness in the joints. This makes it hard for patients to do everyday things.
These flare-ups can happen without warning. They turn mild pain into severe pain that keeps patients in bed for days or weeks.
It’s important to know what causes these flare-ups and what symptoms they bring. We work hard to find flare-ups early and create treatment plans that fit each patient. This helps them manage their RA better and live a better life.

RA is an autoimmune disease where the immune system attacks the body’s own tissues. This leads to inflammation and damage, mainly in the joints. Rheumatoid arthritis flare ups are common, causing a lot of pain and disrupting daily life.
The immune system is key in RA. It usually fights off germs. But in RA, it mistakenly attacks the joints’ lining, causing inflammation. Medical Expert, mostly in small joints.
This mistake involves complex immune actions. It includes the movement of certain cells into joints, making symptoms worse. Knowing this helps understand what causes RA flares.
RA mainly hurts the joints, causing swelling, pain, and damage. It can also affect other parts like the skin, eyes, lungs, heart, and blood vessels.
It can cause symptoms like fatigue, fever, and loss of appetite. In severe cases, it can lead to osteoporosis, heart disease, and lung problems.
RA symptoms go through cycles of flares and remission. During flares, symptoms get worse. In remission, they get better or almost disappear. This makes managing RA hard, as flares can happen anytime.
Knowing what triggers these cycles is key to managing RA. By understanding the immune system’s role, patients and doctors can work to reduce flare-ups.
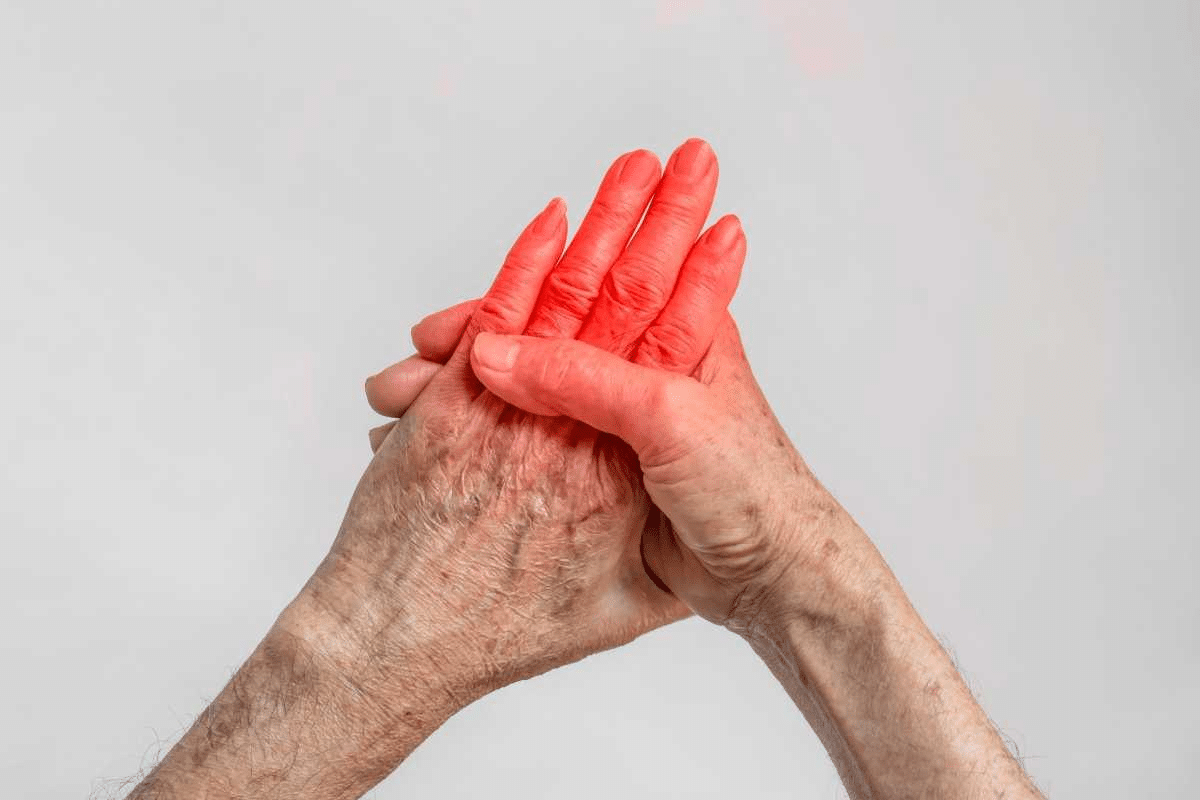
A rheumatoid arthritis flare-up is when the disease gets worse, affecting a person’s life a lot. During a flare, symptoms like intense pain, stiffness, and fatigue get worse. Some people also get fever or rashes, and it can affect their mind too.
Rheumatoid arthritis (RA) flare-ups happen when the disease gets more active. This leads to more inflammation and symptoms. A flare is marked by a big increase in joint pain, swelling, and stiffness. It also brings systemic symptoms like fatigue and fever.
A study in the Arthritis Care & Research journal found that flare-ups really hurt daily life. They make symptoms worse, affecting how well someone can do everyday things.
“Patients experiencing a flare often report increased pain, stiffness, and fatigue, which can be debilitating.”
It’s important to know the difference between RA symptoms and a flare. Daily symptoms are ongoing, like chronic pain and stiffness. A flare is when these symptoms get much worse.
|
Characteristics |
Daily Symptoms |
Flare-Up Symptoms |
|---|---|---|
|
Joint Pain |
Mild to Moderate |
Severe |
|
Stiffness |
Manageable |
Debilitating |
|
Fatigue |
Present |
Severe |
|
Systemic Symptoms |
Absent |
Present (e.g., Fever) |
Flares show that the disease is getting worse. They mean the current treatment might not be working well. Watching for flare-ups helps understand how the disease is changing and if treatment needs to be adjusted.
Knowing about RA flare-ups helps doctors and patients plan better. They can work together to manage these episodes. This improves how well the disease is managed and the patient’s quality of life.
RA flares happen when proinflammatory mesenchymal cells move and release cytokines. This complex process causes inflammation and damage to joints, common in RA.
Proinflammatory mesenchymal cells are key in RA flares. They move to the joints’ synovial tissue. There, they help make proinflammatory cytokines and mediators. This movement starts and keeps inflammation going.
A study in a medical journal said, “The migration of mesenchymal cells to the synovium is a critical step in the pathogenesis of RA, leading to joint inflammation and destruction.”
This process shows how immune cells and joint tissues interact during an RA flare.
Cytokine storms are a big part of RA flares. They happen when proinflammatory cytokines like TNF-alpha and IL-6 are released quickly. These cytokines lead to more inflammation and damage to joints.
|
Cytokine |
Role in RA |
Effect on Joints |
|---|---|---|
|
TNF-alpha |
Proinflammatory cytokine |
Increases inflammation and joint damage |
|
IL-6 |
Proinflammatory cytokine |
Contributes to systemic inflammation |
|
IL-1 |
Proinflammatory cytokine |
Enhances local inflammation |
Acute RA flares cause a lot of damage to joint tissues. The release of cytokines and the action of immune cells break down cartilage and erode bone.
Repeated flares can lead to serious joint damage and disability if not managed well. Knowing how RA flares work is key to finding good treatments.
Knowing what triggers rheumatoid arthritis flare-ups is key to managing the condition. Rheumatoid arthritis (RA) is a chronic disease that causes pain and disability. It’s important to understand what causes flare-ups to manage symptoms better.
Too much physical activity and joint stress can trigger RA flare-ups. Heavy lifting or repetitive tasks can make symptoms worse. It’s best to pace yourself and take breaks to avoid overdoing it.
Poor sleep and chronic fatigue are also big triggers. Bad sleep can make inflammation worse and increase symptoms. Try to sleep well and create a calm sleep space to help.
Stress and emotions can also trigger flare-ups. Stress can make symptoms worse. Doing things like meditation or yoga can help manage stress.
Infections and illnesses can also trigger flare-ups. Fighting off an infection can make RA symptoms worse. Keeping clean and getting vaccinated can help prevent infections.
By understanding and managing these triggers, people with RA can have fewer and less severe flare-ups. This improves their quality of life.
The link between environmental factors and rheumatoid arthritis flare-ups is complex. Many external factors can make symptoms worse. Knowing these factors helps patients and doctors manage the condition better.
Weather changes often trigger rheumatoid arthritis flare-ups. Studies show that temperature, humidity, and barometric pressure changes can affect joint pain and stiffness. The exact reasons are not known, but pressure changes might irritate nerves and cause pain.
Some studies link cold, damp weather to more symptoms. But, what triggers a flare in one person might not affect another the same way.
Air pollution and toxins can also cause flare-ups. Pollutants like particulate matter, nitrogen dioxide, and ozone can start inflammation, making RA symptoms worse. People living in polluted cities face a higher risk.
It’s hard to avoid these pollutants, but using air purifiers and wearing masks can help. Staying away from polluted areas is also a good idea.
Seasonal changes can also affect rheumatoid arthritis symptoms. While it varies, some people find their symptoms get worse at certain times. Knowing these patterns helps patients prepare and adjust their treatment plans.
By understanding environmental factors, patients and doctors can work together. They can adjust treatments, make lifestyle changes, and use coping strategies during high-risk times.
Lifestyle and diet greatly affect RA symptoms and flare-ups. Knowing how they impact RA can help manage the condition better.
Some foods can make RA symptoms worse. Processed foods, sugars, and saturated fats are common offenders. But, eating foods that fight inflammation like omega-3s, fruits, and veggies can help.
Anti-inflammatory Foods: Fatty fish, nuts, and olive oil are good for reducing inflammation.
|
Food Category |
Examples |
Potential Effect on RA |
|---|---|---|
|
Anti-inflammatory Foods |
Fatty fish, nuts, olive oil |
May reduce inflammation |
|
Pro-inflammatory Foods |
Processed foods, sugars, saturated fats |
May exacerbate symptoms |
Smoking increases the risk of RA and makes the disease worse. Drinking alcohol, even in small amounts, can also harm RA symptoms, mainly if done too much.
Impact of Smoking: Smoking can increase the risk of RA and worsen disease activity.
Rest is key during RA flare-ups, but too much rest can harm. Gentle exercises like yoga or swimming help keep joints moving and healthy without making symptoms worse.
Benefit of Gentle Exercise: Gentle exercises can improve joint mobility and reduce stiffness.
There’s a link between gum disease and RA. Gum disease bacteria might trigger or worsen RA symptoms. So, keeping your teeth and gums clean is vital for your health.
Hormonal changes, mainly in women, can make RA symptoms worse. We know RA hits women more often than men. Hormonal shifts are a big reason for this difference.
Women with RA often see their symptoms change with their menstrual cycle. Hormonal changes can mess with the immune system, causing flare-ups. Some women feel their symptoms get worse right before or during their period.
Pregnancy can have a mixed effect on RA symptoms. Some women see their symptoms improve, while others stay the same or get worse. The time after giving birth is often when symptoms can flare up again.
As people get older, their immune systems change, which can affect RA symptoms. It’s important to understand these changes to manage RA well over a person’s lifetime.
Older adults with RA may have different flare patterns than younger people. Things like other health issues, how medicines work together, and overall health can make managing RA harder with age.
When rheumatoid arthritis flares up, patients face intense symptoms that affect daily life. These symptoms vary in severity and impact different health aspects.
Intense joint pain is a key symptom of a flare. Joints become swollen, warm, and tender, making movement painful.
This pain isn’t just in the joints. It can also affect surrounding tissues. This leads to reduced mobility and functionality.
Morning stiffness is common in rheumatoid arthritis, but flares make it worse. It can last for several hours. This stiffness makes everyday activities hard.
Stiffness isn’t just in the morning. It can last all day, getting worse after rest.
During a flare, some patients feel flu-like symptoms. These include fatigue, fever, and feeling unwell. These symptoms are part of the disease’s systemic inflammation.
These symptoms can be very debilitating. They make it hard to do daily tasks and stay active.
The psychological impact of a flare should not be ignored. Chronic pain and discomfort can cause frustration, anxiety, and depression.
It’s important for patients to recognize these emotional changes. They should seek support from healthcare providers, family, and friends to manage flare-related emotions.
Knowing how long and when rheumatoid arthritis flares happen is key to managing the condition. RA is a long-term illness with ups and downs. It’s hard to predict when a flare will happen, so understanding them is important.
About 79 percent of flares get better in three days, but some last longer. How long a flare lasts can vary a lot. Some people get symptoms quickly, while others notice them slowly.
Factors that can affect how long a flare lasts include:
Research shows that how often and how long RA flares last can differ a lot. Some people have many flares, while others have long stretches without symptoms. Knowing these patterns helps tailor treatment to each person’s needs.
Recent studies have looked into what predicts how long a flare will last. They’ve looked at clinical signs and what patients say. This research aims to make RA care more personal and effective.
Many people notice signs before a flare starts. These can be feeling tired, stiff joints, or just not feeling right. Spotting these signs early can help manage the condition better.
By understanding RA flares, patients and doctors can work better together. They can adjust treatments, find and avoid triggers, and improve life quality.
RA flares can cause lasting damage to joints and overall health. These episodes not only harm joints but also affect a patient’s health in many ways.
Frequent RA flares can cause a lot of joint damage. This damage is seen on X-rays. It happens because of long-term inflammation that wears down bone and cartilage.
Table: Progression of Joint Damage in RA Patients
|
Duration of RA |
Percentage of Patients with Joint Damage |
Average Number of Joints Affected |
|---|---|---|
|
0-2 years |
30% |
5 |
|
2-5 years |
60% |
10 |
|
More than 5 years |
80% |
15 |
People with frequent RA flares face a higher risk of heart disease. The ongoing inflammation in RA can lead to heart problems like atherosclerosis.
It’s vital for doctors to manage RA well to lower these risks.
Frequent RA flares greatly reduce a patient’s quality of life. They make it hard to do everyday tasks and keep independence. The pain and stiffness from flares can be very limiting.
RA and its flares can deeply affect mental health. They can cause anxiety, depression, and stress. It’s key to manage RA well to keep both body and mind healthy.
We believe in treating RA in a way that looks at the whole person. We focus on both the physical symptoms and the mental effects of the disease.
Knowing what causes RA flare-ups and spotting the signs of a flare is key to managing RA. We’ve looked into how RA, an autoimmune disease, impacts the body. We’ve also talked about what can trigger flare-ups, like too much activity, environmental factors, and hormonal shifts.
To manage RA well, a mix of treatments is needed. This includes medicines, making lifestyle changes, and managing stress. Eating right, staying away from foods that cause inflammation, and doing gentle exercises can help lessen flare-ups.
Understanding and managing RA flare-ups can greatly improve life. It’s important to know the signs of a flare, like more pain and stiffness in joints. Taking action quickly when these symptoms appear can help manage the condition better.
A rheumatoid arthritis flare-up is when symptoms get worse. This includes more joint pain, stiffness, and swelling.
Many things can trigger a flare-up. This includes too much physical activity, stress, infections, and changes in weather or air quality.
A flare-up brings intense pain and stiffness in the joints. It also causes flu-like symptoms. These can really affect your daily life and how well you can move.
Flare-ups can last different lengths of time. They often start with warning signs before getting worse. Then, they slowly get better.
Yes, making healthy choices can help. Avoiding foods that cause inflammation, staying at a healthy weight, and exercising regularly can reduce symptoms and flare-ups.
Hormonal changes can affect symptoms. This includes during menstrual cycles, pregnancy, and menopause. Some people notice their symptoms change during these times.
Frequent flares can cause lasting damage to joints. They also increase the risk of heart problems. This can lower your quality of life and how well you can function.
Predicting flares is hard. But knowing what triggers them and watching your symptoms can help. This way, you and your doctor can prepare for them.
Managing flares requires sticking to your treatment plan and making healthy choices. Knowing what triggers them can also help lessen their impact.
Government Health Resource. Evidence-Based Medical Guidance. Retrieved from https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(16)30173-8/fulltext
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!