
Explaining the common biological and environmental factors: what causes arthritis flare ups and joint pain accurately.
Millions with arthritis face unpredictable flare-ups that can hit without warning. These episodes leave joints swollen and painful for days or weeks. Knowing what triggers your flare episodes is key. Untreated flares can speed up joint damage and harm your long-term health.
At Liv Hospital, we focus on you with our patient-centered approach. We use the latest research and tailor flare management plans to help you find your triggers early. Things like stress, weather changes, infections, and medication changes can make arthritis flares worse.

Knowing what an arthritis flare-up is is key to managing it well. An arthritis flare-up is when your joint pain, stiffness, swelling, and tiredness get worse. It’s more severe than usual.
A flare-up means your symptoms get worse. This can happen in different ways, depending on your arthritis type. For example, people with rheumatoid arthritis might feel more joint tenderness and swelling. Those with osteoarthritis might feel more pain when they move.
“Arthritis flare-ups can be triggered by various factors, including physical overexertion, inflammatory triggers, and even stress. Understanding these triggers is key to managing flare-ups effectively.”
Here are some common symptoms of an arthritis flare-up:
How long and how severe flare-ups are can differ a lot. Some might last just a few hours. Others can go on for days or even weeks.
|
Characteristics |
Description |
Variability |
|---|---|---|
|
Duration |
Length of time a flare-up lasts |
Few hours to several weeks |
|
Intensity |
Severity of symptoms during a flare-up |
Mild to severe |
|
Symptoms |
Common symptoms experienced |
Pain, stiffness, swelling, fatigue |
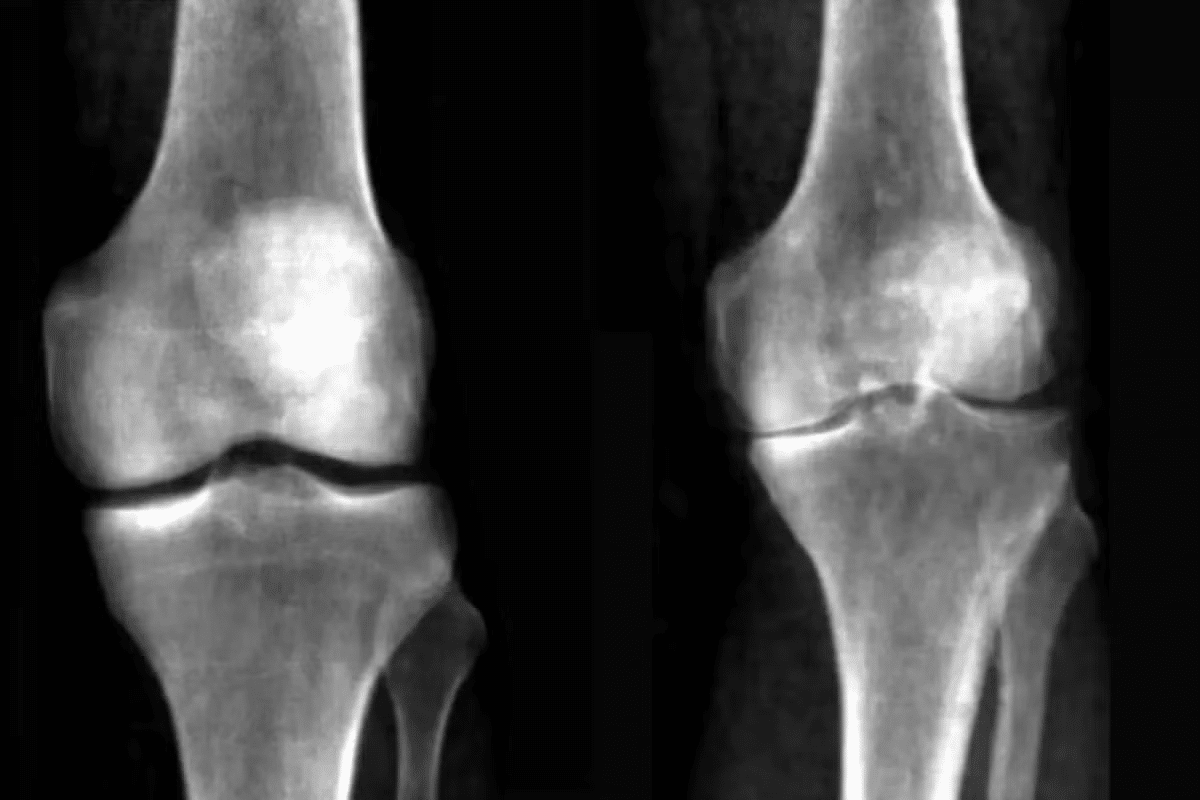
Arthritis is not just one disease but over 100 different conditions. Each has its own flare patterns. Knowing the type of arthritis you have is key to managing symptoms well. We’ll look at the most common types and their flare characteristics.
Rheumatoid arthritis (RA) is an autoimmune disease that causes inflammation in the joints. Flares in RA can be very debilitating, affecting many joints at once. Symptoms include increased joint pain, swelling, and stiffness, along with fatigue and fever.
Osteoarthritis (OA) is the most common arthritis, affecting joints like hips, knees, and hands. OA flares are often caused by overuse or repetitive strain. This leads to more pain and stiffness in the affected joints.
Gout is a form of inflammatory arthritis that causes sudden, severe pain, redness, and tenderness in joints. It often starts at the base of the big toe. Gout flares are triggered by urate crystals in the joint, influenced by diet and other factors.
Psoriatic arthritis (PsA) combines arthritis symptoms with psoriasis. Flares in PsA can involve joint pain and skin lesions. The flare patterns in PsA can be unpredictable and vary a lot from person to person.
To better understand the differences between these types of arthritis and their flare patterns, let’s examine the following table:
|
Type of Arthritis |
Common Triggers for Flares |
Typical Symptoms During Flares |
|---|---|---|
|
Rheumatoid Arthritis |
Stress, infection, hormonal changes |
Joint pain, swelling, stiffness, fatigue |
|
Osteoarthritis |
Overuse, repetitive strain, weather changes |
Joint pain, stiffness, limited mobility |
|
Gout |
Dietary factors (purine-rich foods), dehydration |
Sudden severe joint pain, redness, swelling |
|
Psoriatic Arthritis |
Stress, skin infections, certain medications |
Joint pain, skin lesions, nail changes |
As shown in the table, each type of arthritis has its own triggers and symptoms during flares. Understanding these differences is key to effective management.
Arthritis flare-ups are not random. They are often caused by specific factors that can be managed. Knowing these triggers is key to reducing flare-ups.
Physical overexertion is a major trigger for arthritis flare-ups. It can cause joint strain. This strain can make inflammation and pain worse.
Activities that involve repetitive motions or heavy lifting are bad for people with arthritis. It’s important to balance activity with rest. Gentle exercises like yoga or swimming can help without straining joints. Using the right techniques for physical tasks can also prevent flare-ups.
Certain foods and environmental factors can cause inflammation, leading to flare-ups. Foods high in sugar, salt, and unhealthy fats can trigger inflammation. Pollutants and chemicals can also cause inflammation.
Eating an anti-inflammatory diet can help. This diet includes fruits, vegetables, and omega-3 fatty acids. Avoiding inflammatory triggers and living a healthy lifestyle are important for managing arthritis symptoms.
For those with autoimmune arthritis, like rheumatoid arthritis, the immune system’s response is key. Stress, infections, and hormonal changes can trigger or worsen autoimmune responses.
Managing stress with meditation or deep breathing can help. Staying current with vaccinations and managing health conditions can also prevent infections that may trigger flare-ups.
Stress and emotions play a big role in arthritis flare-ups. Studies show that emotional stress can make arthritis symptoms worse. We’ll look into how stress and emotions affect arthritis and how to manage stress to avoid flares.
Stress makes the body release chemicals like cortisol and adrenaline. These help us deal with stress but can cause inflammation if levels stay high. Inflammation is a big part of arthritis flare-ups. Stress can make inflammation worse, making symptoms more severe.
Feeling anxious or depressed can worsen arthritis symptoms. Bad emotions can make pain feel worse and make it harder to fight inflammation. Also, emotional struggles might make people skip their treatments, making symptoms even worse.
Managing stress is key to avoiding arthritis flare-ups. There are many ways to reduce stress and its effects on arthritis. Good stress management includes mindfulness, meditation, and exercises that fit your abilities.
Understanding how stress and emotions trigger flare-ups helps manage arthritis better. Using stress management techniques can improve overall health and reduce flare-ups.
People with arthritis often feel more pain and stiffness when the weather changes. This is known as “weather pain.” We’ll look at how weather, including pressure, temperature, humidity, and pollution, can make arthritis worse.
Changes in barometric pressure are a big weather trigger for arthritis. When pressure drops, joints can swell, causing pain and stiffness. A patient with rheumatoid arthritis says, “My joint pain gets worse when the weather changes. It’s like my body knows a storm is coming.”
“Changes in barometric pressure can cause the fluid in the joints to expand, putting pressure on the nerves and leading to pain.”
Temperature also affects arthritis symptoms. Some people feel more pain in cold weather, while others find relief. Cold can make muscles and tendons tighten, making joints stiffer and more painful. Warm weather can help by improving blood flow to the joints.
Humidity levels can also impact arthritis symptoms. High humidity makes joints stiffer, while low humidity can cause dryness and irritation. The exact reason is unclear, but it’s thought that humidity changes affect joint pressure.
Air pollution is another environmental factor that can make arthritis worse. Pollutants like particulate matter, nitrogen dioxide, and ozone can trigger or worsen joint inflammation. Staying indoors on polluted days or using air purifiers can help.
Knowing how weather and environmental factors affect arthritis can help manage symptoms. By understanding these triggers, patients can take steps to reduce their impact and improve their life quality.
Diet and nutrition play a big role in managing arthritis flare-ups. What we eat can make symptoms better or worse. It’s important to know how different foods affect our joints.
Some foods can make inflammation worse, which is a big part of arthritis flare-ups. These include processed foods, sugary snacks, and foods with a lot of saturated and trans fats. Avoiding these foods can help lessen flare-ups.
Here are some foods to limit or avoid:
Eating foods that fight inflammation can help manage arthritis symptoms. These foods are full of antioxidants, omega-3 fatty acids, and other nutrients that fight inflammation.
Some good diet approaches include:
Gout, a type of arthritis, is affected by what we eat. Some foods can make gout worse by raising uric acid levels in the body.
|
Foods to Limit |
Reason |
|---|---|
|
Organ meats (liver, kidney) |
High purine content |
|
Certain seafood (anchovies, sardines) |
High purine content |
|
Alcohol (especialy beer) |
Increases uric acid production |
Drinking enough water is key for healthy joints. Water keeps joints lubricated and helps cartilage stay healthy.
Staying hydrated can also reduce stiffness and fatigue from arthritis. Drink plenty of water all day, and before and after working out.
Poor sleep can really affect how our body handles inflammation, leading to more arthritis flare-ups. When we don’t sleep well, our body’s natural healing processes get messed up. This makes it harder to deal with pain and swelling.
Sleep is key in controlling inflammation in our body. During sleep, our body makes cytokines, which fight off infections and swelling. Poor sleep means our body makes fewer cytokines, making it harder to fight inflammation.
A study in the journal Sleep showed sleep loss increases inflammatory markers in the body. This is bad news for arthritis patients, as more inflammation can make symptoms worse and lead to more flare-ups.
Arthritis patients often face sleep disorders because of their condition. Common ones include:
These disorders can make sleep worse, which in turn makes arthritis symptoms worse. It’s important to tackle these sleep disorders to manage arthritis well.
|
Sleep Disorder |
Prevalence in Arthritis Patients |
Impact on Arthritis Symptoms |
|---|---|---|
|
Insomnia |
High |
Increased pain and fatigue |
|
Sleep Apnea |
Moderate |
Increased inflammation and pain |
|
Restless Leg Syndrome |
Moderate |
Disrupted sleep and increased discomfort |
Improving sleep is key to managing arthritis symptoms. Here are some tips to help:
“Good sleep is not just a luxury, it’s a necessity for managing chronic conditions like arthritis. By prioritizing sleep, patients can take a significant step towards reducing their symptoms and improving their quality of life.”
— Medical Expert, Rheumatologist
By tackling sleep issues and improving sleep quality, arthritis patients can better manage their symptoms. This is a vital part of caring for arthritis that should not be ignored.
Medication issues are a big worry for people with arthritis. They can make flare-ups more common and severe. It’s important to know how medicines affect arthritis.
Stopping or cutting back on arthritis meds can lead to more flare-ups. If patients stop their meds without talking to their doctor, symptoms can get worse. This is called a rebound effect.
There are many reasons why people might stop taking their meds. Some include:
But, stopping meds without a doctor’s okay can cause problems. These include:
Medication resistance is when the body gets less responsive to a drug over time. Tachyphylaxis is when the body quickly stops responding to a drug after repeated doses.
Things that can lead to resistance include:
To fight resistance, doctors might:
Drug interactions can also be a big problem. They can change how arthritis meds work and might cause flare-ups. These interactions can happen between arthritis meds and other drugs, like over-the-counter meds and supplements.
Some common interactions are:
|
Interacting Drug |
Arthritis Medication |
Potential Effect |
|---|---|---|
|
NSAIDs |
Methotrexate |
Increased risk of side effects |
|
Corticosteroids |
Biologics |
Altered immune response |
|
Antibiotics |
DMARDs |
Variable effects on drug levels |
To avoid risks, tell your doctor about all meds and supplements you’re taking.
It’s important to understand how hormonal changes affect arthritis symptoms. Hormonal shifts, mainly in women, can make arthritis worse. We’ll look into how these changes impact symptoms.
The menstrual cycle brings big changes in hormones, which can affect arthritis. Some women feel more joint pain and stiffness at certain times. The drop in estrogen before menstruation might be why.
Estrogen’s role in the immune system and its anti-inflammatory effects are being studied. Knowing this can help manage arthritis flares tied to the menstrual cycle.
Menopause brings big hormonal changes, including a drop in estrogen. This can affect arthritis symptoms in different ways. Some women might feel better, while others might feel worse.
The protective effect of estrogen on joints is interesting. Research shows that lower estrogen levels during menopause can cause more joint pain and inflammation in some women.
Thyroid problems, like hypothyroidism and hyperthyroidism, can also affect arthritis symptoms. Thyroid hormones help control metabolism and inflammation. Imbalances can cause musculoskeletal symptoms.
For people with arthritis, thyroid dysfunction can make symptoms worse. It’s key to diagnose and manage thyroid disorders to control symptoms.
Infections and illnesses can make arthritis symptoms worse. When the body finds an infection, it starts an immune response. This can make arthritis symptoms worse. Knowing this helps manage arthritis better.
Viral infections can cause arthritis flare-ups. Some viruses attack the joints, causing pain and swelling. For example, parvovirus B19 and rubella can cause arthritic symptoms.
The body’s immune response to viruses can make arthritis symptoms worse. This is because it produces pro-inflammatory cytokines.
Some key points to consider about viral infections and arthritis include:
Bacterial infections can also cause arthritis flare-ups, like septic arthritis. Septic arthritis happens when bacteria infect the joint, causing severe inflammation and pain. It needs quick medical care to avoid joint damage.
Bacterial infections can lead to:
The immune response is key in how infections affect arthritis. When the body finds an infection, it fights it with an immune response. This response releases cytokines and inflammatory mediators, which can make arthritis symptoms worse. Managing this response is important to stop flare-ups.
Key aspects of the immune response connection include:
Untreated arthritis flares can cause serious problems. These include joint damage and health issues that affect the whole body. If not treated, these flare-ups can greatly reduce a person’s quality of life and health.
One major issue with untreated arthritis flares is joint damage. Inflammation can wear down cartilage and bone, causing pain and mobility issues. Early treatment is key to avoiding lasting damage.
Arthritis is more than just joint pain. It can also harm the body’s overall health. This can lead to osteoporosis, infections, and other autoimmune diseases. Managing arthritis is important for overall health.
Untreated arthritis flares can greatly lower a person’s quality of life. Chronic pain and mobility issues can limit daily activities. They can also affect mental health and relationships. Effective arthritis management is vital for a good life.
People with rheumatoid arthritis face extra heart risks. Research shows they are more likely to have heart attacks and strokes. Controlling rheumatoid arthritis is key to heart health.
In summary, untreated arthritis flares have serious effects. They harm joints and overall health, and lower quality of life. It’s critical for those with arthritis to work with their doctors to manage their condition. This helps prevent long-term problems.
Knowing what causes arthritis flare-ups is key to managing them. By finding out what triggers them for you and using prevention methods, you can lessen flare-ups. This helps you feel better overall.
Handling arthritis flare-ups means making lifestyle changes, sticking to your treatment plan, and managing stress. To prevent flare-ups, eat foods that fight inflammation, exercise regularly, and get enough sleep.
Every person’s arthritis is different, so there’s no single way to manage it. It’s important to work with your doctor to create a plan that fits you. This plan should help keep your joints healthy.
By taking charge of your arthritis, you can reduce the effects of flare-ups and live a better life. Using the right prevention and management strategies can cut down on pain and improve your function. This leads to a better quality of life.
An arthritis flare-up is when symptoms get worse suddenly. This includes more pain, swelling, stiffness, and feeling tired.
Symptoms include joint pain, stiffness, swelling, and feeling very tired. Knowing these symptoms helps manage flare-ups better.
Rheumatoid arthritis, osteoarthritis, gout, and psoriatic arthritis often have flare-ups. Each has its own signs and causes.
Too much physical activity can strain joints. This can cause inflammation and make arthritis symptoms worse.
Yes, stress can make arthritis symptoms worse. It can increase inflammation and affect the immune system.
Weather changes can make arthritis symptoms worse. Changes in pressure, temperature, and humidity can affect joints and cause pain.
Eating foods that cause inflammation, not drinking enough water, and certain foods for gout can trigger flare-ups.
Poor sleep can increase inflammation. This can make arthritis symptoms worse and even trigger flare-ups.
Yes, stopping medication, not responding to it, or drug interactions can lead to flare-ups.
Hormonal changes, like during the menstrual cycle or menopause, can affect arthritis symptoms. They might even trigger flare-ups.
Yes, infections can trigger flare-ups. They can stimulate the immune system and increase inflammation.
Untreated flare-ups can cause permanent joint damage. They can also lead to health problems, lower quality of life, and increase heart disease risks.
Knowing what triggers flare-ups and using preventive measures can help. This can reduce how often and how severe flare-ups are, improving overall health.
Drinking enough water is key for joint health. It can also help reduce the severity of flare-ups.
Yes, air pollution can increase inflammation. This can trigger arthritis flare-ups.
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5053080/
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!