We are dedicated to caring for those with rare autoimmune diseases like ANCA-associated vasculitis. This condition causes inflammation in small to medium-sized blood vessels. If not treated, it can lead to serious health problems and even death.
ANCA-associated vasculitis affects about 20 people per million in Europe and North America each year. It is marked by the presence of anti-neutrophil cytoplasmic autoantibodies (ANCA). These antibodies mistakenly attack neutrophils, causing inflammation and damage to blood vessels.c anca positive vasculitisTest for Antibodies: The Ultimate, Simple Guide
Getting the right diagnosis is key. It involves looking at symptoms, running lab tests, and using imaging to see how much blood vessels are affected.
To understand ANCA positive vasculitis, we need to know what it is and how it works. It’s a disease where certain antibodies attack proteins in neutrophils, causing inflammation in blood vessels.
ANCA positive vasculitis is marked by the presence of specific antibodies. These antibodies target proteins in neutrophils, leading to damage in blood vessels. The disease is caused by a mix of genetics, environment, and immune system issues.
The type of ANCA antibody can affect how the disease shows up and how it progresses. For example, PR3-ANCA is often seen in granulomatosis with polyangiitis (GPA). MPO-ANCA is more common in microscopic polyangiitis (MPA) and eosinophilic granulomatosis with polyangiitis (EGPA).
ANCA-associated vasculitis is a rare disease with varying rates worldwide. The epidemiology is influenced by many factors, including where you live, your genes, and your environment. It seems that more cases are being found, possibly because of better testing and awareness.
The main types of ANCA vasculitis are GPA, MPA, and EGPA. Each type has its own symptoms and affects different organs. Knowing about these types is key to catching the disease early and treating it well.
C-ANCA, or cytoplasmic antineutrophil cytoplasmic antibodies, are key in ANCA-associated vasculitis. We’ll look at how these antibodies cause disease and what affects their development.
ANCA antibodies, mainly targeting proteinase 3 (PR3), are central to C-ANCA positive vasculitis. These antibodies activate neutrophils. This leads to the release of harmful substances and causes inflammation and damage to blood vessels.
The activation of neutrophils by ANCA antibodies causes these cells to stick to the blood vessel walls. This leads to the release of pro-inflammatory cytokines and damage to the vessel walls. This is a major part of how ANCA-associated vasculitis works. C-ANCA usually targets PR3, with 75-90 percent of GPA patients testing positive, showing its importance in this type of vasculitis.
Genetic and environmental factors both play a role in ANCA-associated vasculitis. Genetic predisposition is a big factor, with certain HLA alleles and other genetic variants increasing the risk of the disease.
Environmental triggers, like infections and exposure to certain chemicals, can also start ANCA-associated vasculitis in people who are at risk. Knowing these risk factors is key for early diagnosis and treatment.
Understanding how genetics and environment interact helps us grasp the mechanisms behind C-ANCA positive vasculitis. This knowledge can improve our diagnosis and treatment of this complex condition.
It’s important to know the different types of ANCA-associated vasculitis for the right treatment. Each type has its own symptoms and needs a special treatment plan.
Granulomatosis with Polyangiitis, also known as Wegener’s granulomatosis, has granulomatous inflammation. It mainly affects the lungs and kidneys. GPA is linked to C-ANCA, which targets proteinase 3 (PR3-ANCA).
GPA’s symptoms include chronic sinusitis, nasal ulcers, and lung nodules. It also causes kidney damage quickly if not treated.
Microscopic Polyangiitis has necrotizing vasculitis without many immune deposits. It mainly harms small blood vessels. MPA is linked to P-ANCA, which targets myeloperoxidase (MPO-ANCA).
MPA’s symptoms include kidney problems and lung bleeding. It starts quickly compared to GPA.
Eosinophilic Granulomatosis with Polyangiitis, also known as Churg-Strauss syndrome, has eosinophil-rich granulomatous inflammation. It’s different because it often comes with asthma and high eosinophil counts.
EGPA patients have asthma, high eosinophil counts, and vasculitis in various organs. The presence of eosinophils and asthma are key signs of EGPA.
In summary, GPA, MPA, and EGPA are the main types of ANCA-associated vasculitis. Each has its own symptoms and needs a specific treatment. Knowing these differences is key to good patient care.
ANCA-associated vasculitis is a complex condition. It shows up in many ways and can affect different parts of the body. This leads to a variety of symptoms.
People with ANCA-associated vasculitis often feel fever, weight loss, and fatigue. These signs are not specific but show that the body is fighting an infection. The severity of these symptoms can vary and may be accompanied by other signs of illness.
Kidney problems are common in ANCA-associated vasculitis. This often shows up as rapidly progressive glomerulonephritis (RPGN). If not treated quickly, RPGN can cause kidney failure. Kidney issues can range from mild to severe, needing immediate medical care.
The respiratory system is often affected by ANCA-associated vasculitis. Symptoms can include chronic sinusitis, lung nodules, and alveolar hemorrhage. These symptoms can greatly affect a person’s quality of life and need careful management.
Other parts of the body can also be affected. Patients may have skin rashes, joint pain, and neurological symptoms. The different ways the disease can affect the body highlight the need for a detailed diagnosis.
In summary, ANCA-associated vasculitis shows a wide range of symptoms and manifestations. Understanding these is key to early diagnosis and effective treatment.
Diagnosing ANCA-associated vasculitis mainly uses lab tests, like ANCA testing. ANCA (Anti-Neutrophil Cytoplasmic Antibodies) tests are key. They help tell this condition apart from other vasculitis types.
There are two main ways to do ANCA testing: indirect immunofluorescence (IIF) and enzyme-linked immunosorbent assay (ELISA). IIF finds ANCA antibodies. ELISA measures how much of these antibodies are against specific things, like proteinase 3 (PR3) and myeloperoxidase (MPO).
When looking at ANCA test results, it’s important to think about the whole picture. A positive test helps confirm ANCA-associated vasculitis. But, it’s not enough on its own. You also need to consider symptoms, imaging, and other lab tests for a correct diagnosis.
ANCA antibodies can be split into two types based on IIF: C-ANCA and P-ANCA. C-ANCA usually targets PR3, while P-ANCA targets MPO. Knowing this is important because C-ANCA is often linked to Granulomatosis with Polyangiitis (GPA). P-ANCA is more common in Microscopic Polyangiitis (MPA) and Eosinophilic Granulomatosis with Polyangiitis (EGPA).
|
ANCA Pattern |
Target Antigen |
Common Clinical Association |
|---|---|---|
|
C-ANCA |
PR3 |
GPA |
|
P-ANCA |
MPO |
MPA, EGPA |
Other blood tests are also helpful. They help see how the disease is doing and if treatment is working. These include:
“The combination of clinical assessment, ANCA testing, and other laboratory tests is essential for the accurate diagnosis and management of ANCA-associated vasculitis.”
We stress the need for a full diagnostic plan. This includes both doctor’s checks and lab tests to manage ANCA vasculitis well.
Advanced diagnostic procedures are key in diagnosing and managing ANCA Positive Vasculitis. They help doctors confirm vasculitis, see how much organs are involved, and track the disease’s progress.
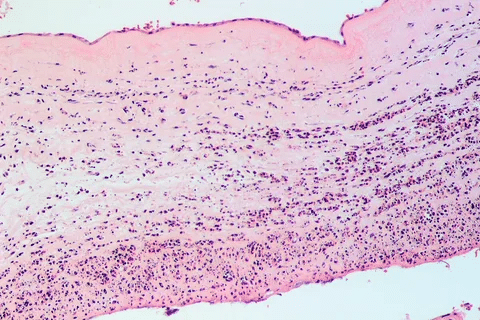
A tissue biopsy is a vital tool for diagnosing vasculitis. It shows necrotizing vasculitis, a key sign of ANCA-associated vasculitis. This helps doctors know which type of vasculitis it is and how to treat it.
“The biopsy is a critical diagnostic tool, giving a direct look at vasculitis’s inflammation and damage,” says Medical Expert, a top rheumatologist. This quote shows how important biopsy is for diagnosing vasculitis.
Imaging studies like CT scans and MRIs are key for seeing how much organs are affected and how the disease is progressing. They can spot damage in organs like the kidneys, lungs, and sinuses, which are often hit by ANCA Positive Vasculitis.
For example, a CT scan of the chest can show lung nodules, cavities, or infiltrates. An MRI can check how much the kidneys are damaged. These findings are vital for making treatment plans and checking how well treatment is working.
Diagnosing ANCA Positive Vasculitis involves clinical findings, lab tests, and imaging studies. The Chapel Hill Consensus Conference criteria are often used to classify ANCA-associated vasculitis. These criteria look at ANCA antibodies, symptoms, and biopsy results.
Getting the diagnosis and classification right is key for choosing the right treatment and improving patient outcomes. By using clinical evaluation and advanced diagnostic methods, doctors can give personalized care to patients with ANCA Positive Vasculitis.
ANCA-associated vasculitis treatment is a mix of strategies to fight inflammation and stop it from coming back. It’s all about finding the right plan for each patient, based on their specific needs and how severe their disease is.
Induction therapy is the first step to tackle the disease’s acute inflammation and get it into remission. We use a mix of corticosteroids and immunosuppressive agents, like cyclophosphamide or rituximab, to quickly lower disease activity.
“The goal of induction therapy is to induce remission and prevent organ damage,” as emphasized in clinical guidelines. The choice of therapy depends on how severe the disease is, the patient’s health, and possible side effects.
After achieving remission, we start maintenance therapy to keep the disease under control and prevent it from coming back. We often use azathioprine or methotrexate for this, as they help prevent relapses.
There’s always new research into better treatments for ANCA-associated vasculitis. We’re looking at targeted therapies and biologic agents. These new options aim to be more effective, have fewer side effects, and offer choices for those who don’t respond to usual treatments.
“The development of new treatments for ANCA-associated vasculitis is critical, as it brings hope for better patient outcomes and quality of life.”
Expert Opinion
We keep working on improving treatment options for ANCA-associated vasculitis. Our goal is to make sure patients get the best care tailored just for them.
Living with ANCA vasculitis can be tough, but with the right care, patients can stay active. We know managing this condition needs a full plan, not just treatment.
Regular checks and follow-ups are key to managing ANCA vasculitis well. This means:
One patient said, “Regular visits with my doctor have helped me manage my condition and avoid relapses.”
“The key to managing ANCA vasculitis is early detection and treatment of relapses. Regular follow-up appointments help us catch any issues before they become severe.”
People with ANCA vasculitis can face complications like kidney damage, breathing problems, and infections. To manage these, we focus on:
|
Complication/Comorbidity |
Management Strategy |
|---|---|
|
Kidney Damage |
Regular kidney function tests, medication to reduce proteinuria |
|
Respiratory Issues |
Pulmonary function tests, bronchodilators, and corticosteroids |
|
Infections |
Prophylactic antibiotics, vaccinations, and prompt treatment of infections |
Support and lifestyle changes are key to a better life for patients with ANCA vasculitis. This includes:
By using a full management plan that includes long-term monitoring, managing complications, and support, patients with ANCA vasculitis can live fulfilling lives.
ANCA-positive vasculitis is a complex condition that needs a detailed approach for diagnosis and treatment. We’ve covered its clinical signs, how to diagnose it, and treatment choices.
Understanding ANCA-associated vasculitis well is key for better patient care. Recognizing symptoms, using the right tests, and effective treatments help manage the disease. This way, we can lessen its effects on patients.
Managing ANCA-positive vasculitis is an ongoing task. It’s vital to keep an eye on patients, handle complications, and offer support. As we learn more, we can find better ways to treat it and care for patients.
Our talk on vasculitis anca c shows how ANCA antibodies cause inflammation in blood vessels. A detailed look at ANCA-positive vasculitis shows we need a broad approach to handle it.
ANCA positive vasculitis is a rare autoimmune disease. It causes inflammation in blood vessels. Conditions like Granulomatosis with Polyangiitis (GPA), Microscopic Polyangiitis (MPA), and Eosinophilic Granulomatosis with Polyangiitis (EGPA) fall under this category.
Symptoms vary based on the affected organs. They can include fever, weight loss, and fatigue. Kidney issues, lung problems, and skin, eye, or nervous system issues are also common.
Diagnosis involves clinical evaluation, lab tests, and imaging studies. ANCA testing is key. A tissue biopsy can confirm the disease.
C-ANCA targets proteinase 3 (PR3) and is linked to GPA. P-ANCA targets myeloperoxidase (MPO) and is seen in MPA and EGPA.
Treatment includes corticosteroids and immunosuppressants like cyclophosphamide or rituximab. This aims to control inflammation and induce remission. Maintenance therapy with azathioprine or methotrexate helps prevent relapses.
There’s no cure, but treatment can manage the disease. The goal is to keep the disease in remission and improve quality of life.
Genetics and environmental factors, like infections or chemicals, play a role in developing ANCA-associated vasculitis.
Monitoring includes checking symptoms, lab tests, and imaging studies. This helps assess organ involvement and treatment response.
Untreated or poorly managed, complications can include kidney and lung failure, and cardiovascular disease.
Yes, support includes patient organizations, counseling, and lifestyle advice. These resources help manage the condition and improve quality of life.
Prognosis depends on disease severity, treatment response, and complications. With proper treatment, many patients can achieve remission and live active lives.
National Center for Biotechnology Information. Positive ANCA Test: Meaning and Implications for Patient Health. Retrieved from
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3750501/
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!