Last Updated on November 25, 2025 by
Men with prostate cancer might need to have their prostate gland removed. This surgery is a key treatment. The prostate gland is vital for men’s health, but removing it can save lives when cancer is present.
Thinking about prostate removal surgery can be scary. People worry about side effects and how it will change their lives. But thanks to new prostatectomy surgery methods, there’s hope for those with prostate cancer.
We’ll look into what happens when the prostate is removed. We’ll talk about the prostate gland’s role, why it’s removed, and the latest in surgery.
Radical prostatectomy is a key treatment for prostate cancer in men. It involves removing the prostate gland and some surrounding tissue. We’ll explain the steps, surgical methods, and how robotic technology is making surgery better.
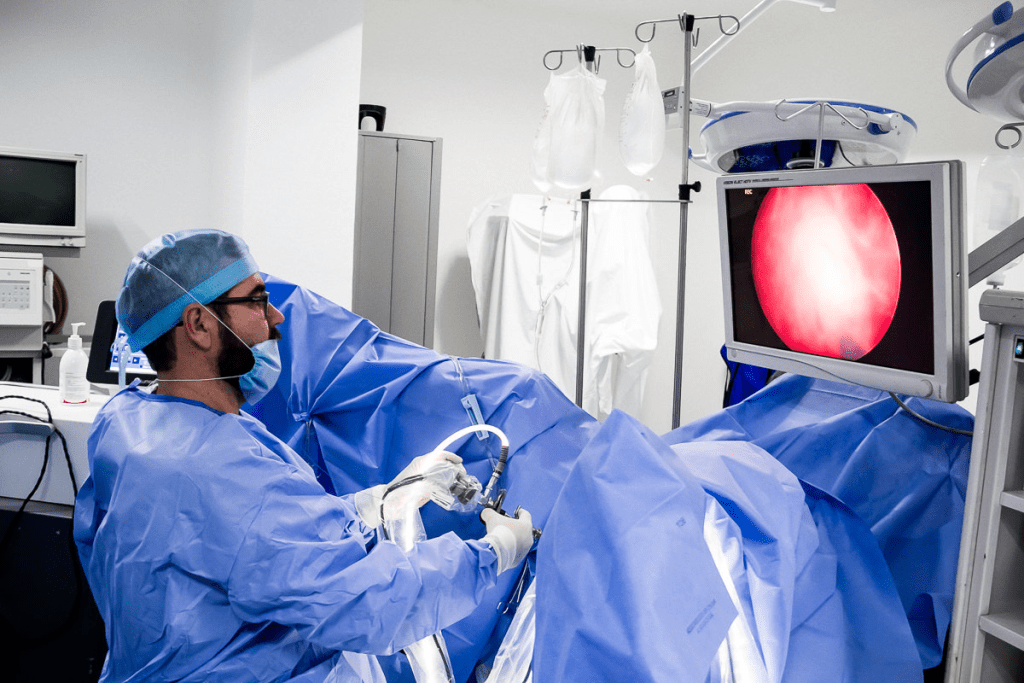
The surgery starts with general anesthesia to keep the patient comfortable. The surgeon then makes incisions based on the chosen method. The prostate gland is carefully dissected and removed, along with the seminal vesicles.
The next step is reconnecting the bladder to the urethra. This is a critical part of urinary health after surgery. After that, the incisions are closed, and the patient goes to the recovery room.
Radical prostatectomy can be done in different ways. Open surgery uses a big incision, while laparoscopic surgery uses small incisions. Laparoscopic surgery is less invasive and leads to quicker recovery.
Robotic-assisted prostatectomy is a big step forward in surgery. It uses a robotic system like the da Vinci Surgical System. This system offers better vision, precise tools, and comfort for the surgeon.
Robotic-assisted surgery is now the standard for radical prostatectomy. It leads to less pain and quicker recovery for patients.
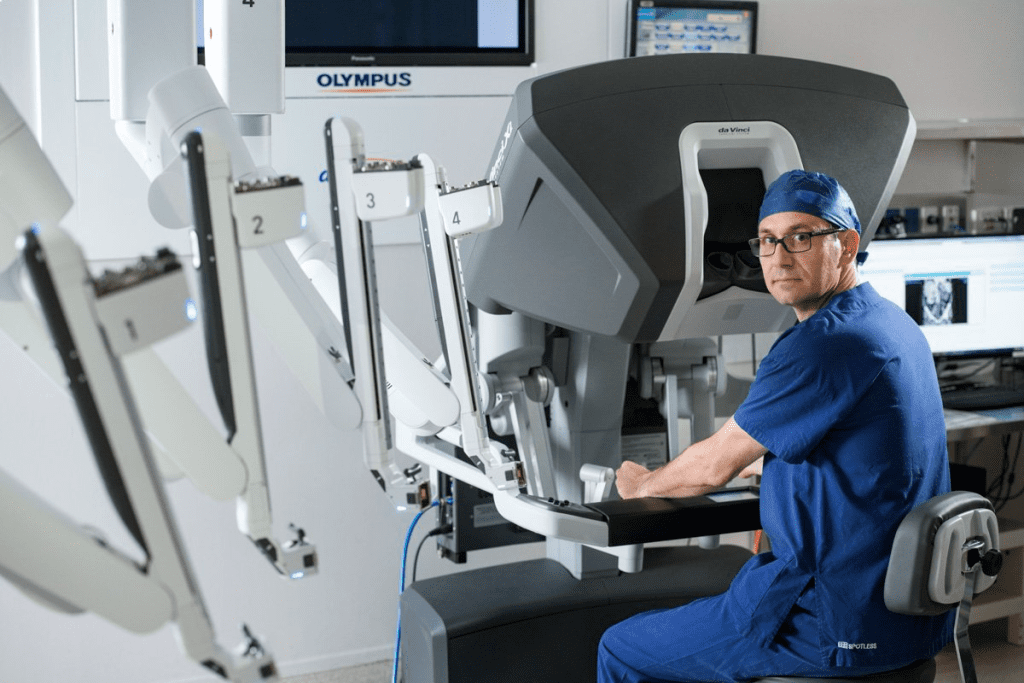
Medical technology keeps improving, making robotic-assisted systems better for prostate surgery. Knowing about these options helps patients choose the best treatment.
It’s important for patients to know about the side effects of prostate removal before surgery. This surgery is a common treatment for prostate cancer. But it can cause several side effects that patients should be aware of.
Urinary incontinence is a big worry for many after prostate removal. Studies show that 15% to 17% of men deal with some form of incontinence after surgery. This can be anything from a little leakage to more serious incontinence.
The reasons for incontinence vary. It can happen because of damage to the muscles and nerves during surgery. But most men get better over time. Many regain full control of their bladder within a year.
Key statistics on urinary incontinence:
Erectile dysfunction (ED) is another common side effect of prostate removal surgery. About 30% to 53% of men report ED after prostatectomy. The main reason is damage to the nerves that control erections during surgery.
Using nerve-sparing techniques has helped improve outcomes. But the risk of ED is not gone. The patient’s age, how well they could get an erection before surgery, and the surgery method all play a role.
Prevalence and causes of erectile dysfunction:
Pain and discomfort are common during recovery after prostate removal. The amount of pain can vary. But most patients feel some discomfort, mostly in the first few weeks after surgery.
It’s key to manage pain well during recovery. This can include taking medication, resting, and slowly starting to move more. Patients should follow their doctor’s advice on managing pain and discomfort.
Medical technology has changed prostatectomy surgery a lot. Now, patients get better results and heal faster. New methods in prostatectomy have made surgery better for everyone.
New tech and surgical methods have made care better. Techniques like robotic surgery, NeuroSAFE, and nerve-sparing are leading the way. These changes help patients live longer and feel better after surgery.
Robotic-assisted surgery is key in today’s prostatectomy. It lets surgeons do precise work. This means patients have less blood loss and heal quickly.
Research shows robotic surgery works well. It cuts down on problems and makes surgery more accurate. Now, 95% of prostate surgeries use robots, showing how effective it is.
The NeuroSAFE technique is a big step forward in prostate surgery. It watches nerves during surgery to maintain erectile function. This method doubles the chance of recovering sexual function.
This is great for patients worried about keeping their sexual health. Seeing and saving nerves in real-time is a big deal in prostate surgery. It gives patients hope for their sexual health.
Nerve-sparing methods are key to keeping function after prostate surgery. They help keep nerves around the prostate safe. These nerves are important for sex and urine control.
Using nerve-sparing methods lowers the chance of lasting problems. Success depends on the surgeon and the patient’s health. When done right, it improves life quality for patients.
Knowing what to expect after prostate surgery can make recovery easier. We’ll walk you through each stage, from right after surgery to when you regain your urinary and sexual functions.
The first 48 hours are key. You’ll likely stay in the hospital for 1-2 days. We focus on keeping you comfortable and watching for any issues.
The first four weeks are about healing. You might feel tired, sore, and have trouble controlling your urine. Here’s what we suggest:
Getting better with urine control takes time. Most men see big improvements in six months. Pelvic floor exercises, or Kegels, are key in this recovery.
Getting back to normal sexually can take a year or more. If the surgery spared nerves, you might recover faster. We’ll help you understand your options and manage your expectations.
Recovering from prostate surgery is a journey. It needs patience, understanding, and support. Knowing what to expect at each stage helps you navigate it better and get the best results.
Choosing to have a prostate removed is a big decision. It’s important to know what it means for the long run. Living without a prostate means making changes that can affect many parts of a man’s life.
Prostate removal can affect a man’s ability to have children. Men can no longer father children naturally after a prostatectomy. This is because the prostate is part of the reproductive system, and removing it changes the seminal fluid. If you haven’t finished having children, talk to your doctor about keeping your fertility before surgery.
Urination changes are also big. Some men might leak right after surgery, but most regain control within a year. Doing Kegel exercises can help with recovery. You might need to make lifestyle changes or manage occasional leaks to keep your urinary health good.
Sex life changes too. Erectile dysfunction is common, but how much it affects you can vary. Using nerve-sparing techniques during surgery can help you keep your erectile function. You might need to try treatments for erectile dysfunction to keep your sex life healthy and fulfilling.
The emotional impact of not having a prostate is real. Men might feel many emotions, from relief to worry about the future. Getting support from doctors, family, and support groups is key to your mental health. Staying active and connected with others can also improve your overall well-being.
Knowing what to expect can help men get ready for life after a prostate removal. While everyone’s experience is different, being informed and supported can help you face the challenges and opportunities ahead.
For some patients, prostate removal is just the first step in their treatment journey, with further interventions needed to address ongoing health concerns. While many men recover well from prostatectomy, others may experience persistent side effects or cancer recurrence, necessitating additional treatments.
Urinary incontinence is a common side effect after prostate removal. We offer various treatments to manage incontinence, including pelvic floor exercises, behavioral therapy, and in some cases, surgical interventions like the implantation of an artificial urinary sphincter.
Pelvic floor rehabilitation is a key part of managing incontinence. It helps strengthen the muscles that support the bladder and urethra. This way, patients can better control their urinary function.
Erectile dysfunction is another possible side effect of prostate removal. We provide a range of treatments to help restore sexual function, including oral medications, vacuum erection devices, and penile implants.
Nerve-sparing techniques during surgery can greatly reduce the risk of erectile dysfunction. For those who experience persistent erectile dysfunction, our specialists work with them to find the most effective treatment plan.
Cancer recurrence after prostate removal is a concern for many patients. We closely monitor PSA levels to detect any recurrence early. Treatment options for recurrent prostate cancer include radiation therapy, hormone therapy, and in some cases, clinical trials for new treatments.
Early detection of recurrence is key for effective management. We work closely with patients to develop a personalized follow-up plan. This includes regular PSA monitoring and other diagnostic tests as needed.
Beyond managing specific side effects, we offer a range of supportive therapies to enhance overall well-being. These include physical therapy, counseling, and nutritional guidance tailored to the needs of men after prostate removal.
Rehabilitation is a key part of the recovery process. By addressing the physical, emotional, and nutritional aspects of health, we help patients achieve the best possible outcomes after prostatectomy.
Understanding prostatectomy and its effects is key to making smart choices about your prostate health. We’ve looked at different surgical methods, like robotic-assisted technology and nerve-sparing approaches. These have greatly improved how well patients do after surgery.
It’s also important to manage side effects like urinary incontinence and erectile dysfunction. Knowing about these changes and new ways in prostatectomy helps patients choose the right treatment.
At our place, we focus on giving full support and advice to help patients with their prostate health. We mix medical knowledge with care and understanding. This way, we help people take charge of their health and make wise choices about their care.
To make good choices about prostate health, you need to know all your options and what might happen. We suggest talking to your doctor to find the best treatment for you.
The prostate gland is a small gland in men, about the size of a walnut. It’s important for making fluids that are part of semen. It also helps control urine flow by surrounding the urethra.
Prostate removal surgery, or prostatectomy, is mainly for treating prostate cancer. It can also help with severe benign prostatic hyperplasia (BPH).
There are several types of prostatectomy. These include open radical prostatectomy, laparoscopic radical prostatectomy, and robotic-assisted laparoscopic prostatectomy. The right surgery depends on the case and the surgeon’s advice.
Recovery from prostate removal surgery takes several weeks to months. The first 1-4 weeks can be tough, with discomfort, urinary issues, and erectile problems.
Side effects include urinary incontinence, erectile dysfunction, and changes in orgasm. Some may also face pain, discomfort, or swelling.
Yes, living without a prostate is possible. Removing the prostate doesn’t stop a man from living a fulfilling life. Adjustments may be needed to manage side effects.
Robotic-assisted prostatectomy has benefits like smaller incisions and less blood loss. It also leads to faster recovery and better outcomes due to enhanced precision.
The NeuroSAFE technique is a nerve-sparing method used in prostatectomy. It aims to preserve nerves for erectile function. This technique can double the chances of recovering erectile function.
Yes, treatments for side effects include medications, physical therapy, and supportive therapies. For erectile dysfunction, medications or implants may help. For urinary incontinence, pelvic floor physical therapy is beneficial.
Yes, prostate cancer can come back after surgery. The risk depends on the cancer’s stage and grade. Regular check-ups and monitoring are key to catching any recurrence early.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!