
Listing five key radiological signs revealed by an osteoarthritis knee x ray, including joint space narrowing.
We know that diagnosing knee osteoarthritis needs clear and reliable images. X-rays are the top choice for spotting signs of this joint disease.
We use the latest diagnostic methods at Liv Hospital. We look for five main signs of osteoarthritis in joints. This helps us decide the best treatment and improve patient care.
At Liv Hospital, we focus on our patients. We use proven methods to check and treat knee osteoarthritis. This ensures our patients get the best care possible.

Knee osteoarthritis becomes more common with age, hitting those over 45 hard. About 12.5 percent of people over 45 have it. This shows why we need to know about it and manage it well.
Osteoarthritis is the top arthritis type, and age is a big risk factor. As we get older, our joints, like the knee, wear out. This can cause osteoarthritis. It not only hurts our quality of life but also costs a lot in healthcare and lost work.
Knee osteoarthritis really affects people over 45. It causes pain, stiffness, and makes moving hard. Knowing how common and impactful it is helps us find better ways to manage it.
|
Age Group |
Prevalence of Knee OA |
Impact on Quality of Life |
|---|---|---|
|
45-54 years |
8% |
Moderate pain and stiffness |
|
55-64 years |
12% |
Significant pain and reduced mobility |
|
65+ years |
18% |
Severe pain and significant mobility issues |
Knee osteoarthritis happens when the cartilage in our joints wears down. This makes the bone underneath get affected, leading to bone spurs and cysts. This damage causes pain and makes it hard to move the joint.
Key factors in the pathophysiology include:
Knowing these factors helps us diagnose and treat knee osteoarthritis better. X-rays and MRI are key for seeing how damaged the joint is and deciding on treatment.
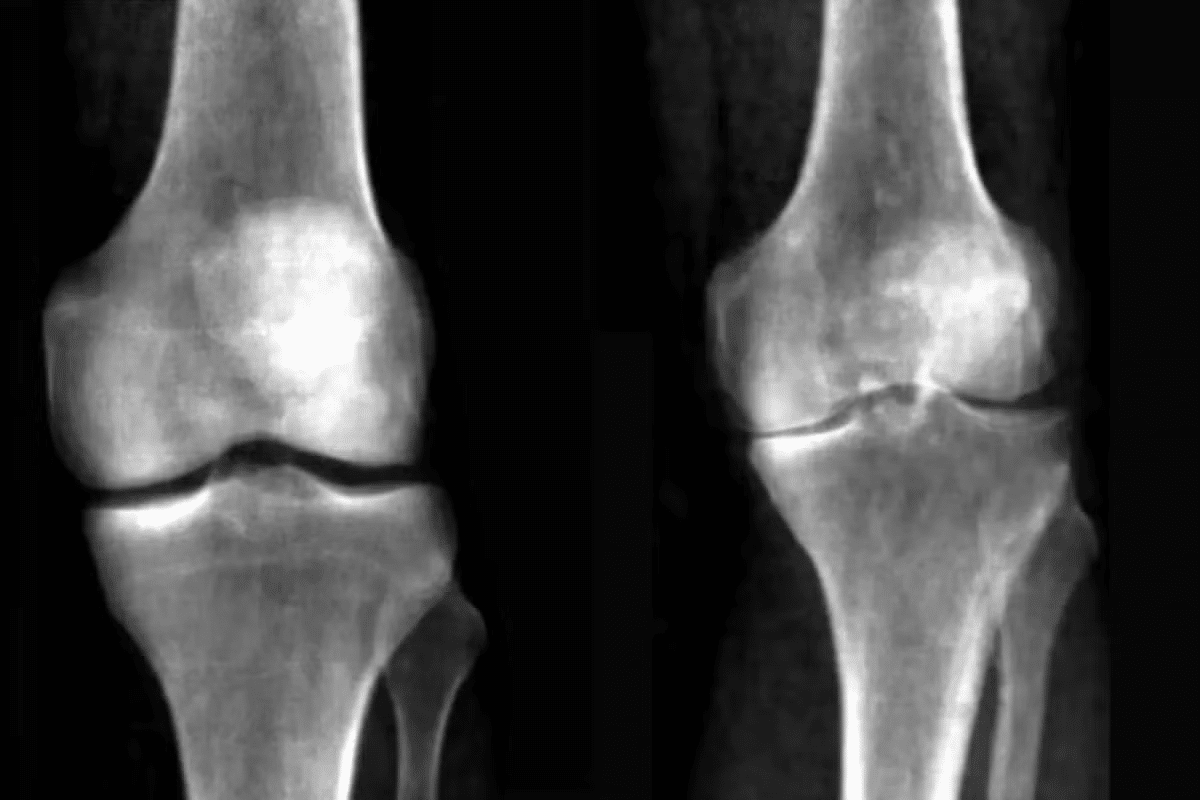
Knee X-rays are key in spotting degenerative changes in the joint. They are the most affordable and easy-to-get imaging option for first checks.
Knee X-rays are a top choice for diagnosing osteoarthritis. They show joint space narrowing, bone spurs, and other signs of wear and tear. This makes them vital for checking patients who might have osteoarthritis.
One big plus of using knee X-rays is how affordable they are. Compared to MRI, X-rays are cheaper and easier to find. They’re perfect for starting off in primary care.
X-rays are also easy to get because they’re common in most hospitals. This means patients can get checked quickly. It helps doctors start treatment sooner.
Knowing when to get knee X-rays is important for diagnosing osteoarthritis. They’re suggested for those with knee pain, stiffness, or trouble moving.
Doctors should also consider X-rays for patients with risk factors like age, weight, past injuries, or family history. Early scans help confirm the diagnosis and guide treatment.
Using knee X-rays helps doctors understand a patient’s condition better. This leads to better management and treatment of osteoarthritis.
Getting a proper radiographic assessment is key for diagnosing and managing knee osteoarthritis. We need high-quality images to make accurate diagnoses and plan treatments.
To fully assess knee osteoarthritis, we use three main radiographic views: anteroposterior (AP), lateral, and skyline. Each view gives us unique insights into the knee joint.
Weight-bearing radiographs are essential for accurately assessing knee osteoarthritis. Unlike non-weight-bearing images, they show the true extent of joint space narrowing and other degenerative changes under load.
Weight-bearing images have several benefits:
By using the right technique and weight-bearing images, we can get a clear and accurate picture of knee osteoarthritis. This helps us make effective treatment decisions.
One key sign of cartilage loss in osteoarthritis is the narrowing of the joint space. This narrowing is often seen in the medial tibiofemoral compartment. It’s a major feature of osteoarthritis. Understanding this is vital for patient health and mobility.
Normal joint space measurements are over 5mm. Keeping a healthy joint space is key for smooth movement and pain-free knees. Studies show that joint space narrowing is a reliable sign of osteoarthritis getting worse. “Assessing joint space narrowing is vital for diagnosing and tracking osteoarthritis,” say doctors.
The medial compartment of the knee is more often hit by osteoarthritis than the lateral. This is because the medial compartment bears more weight. The pattern of joint space narrowing in the medial compartment offers insights into osteoarthritis severity. Research shows that the rate of joint space narrowing matches the worsening of osteoarthritis symptoms.
Joint space narrowing is linked to more pain and mobility issues in osteoarthritis patients. As the joint space narrows, bone-on-bone contact increases, causing pain and reduced mobility. Spotting joint space narrowing early with X-rays or MRIs can lead to timely interventions to slow disease progression. A study found that the degree of joint space narrowing predicts functional limitations in knee osteoarthritis patients.
In summary, joint space narrowing is a key sign of cartilage loss in osteoarthritis. Knowing its patterns and how it relates to symptoms helps in managing the disease. With the help of X-rays and MRIs, healthcare providers can create effective treatment plans to improve patient outcomes.
Osteophytes are a key sign of osteoarthritis, seen on X-rays as bone spurs. These bony growths form at the joint edges. They help doctors diagnose osteoarthritis, often in the knee.
Marginal osteophytes grow at the joint edges. On an X-ray of an OA knee, they look like spurs along the joint edges. They form as the body tries to fix the damaged joint.
Key locations for marginal osteophytes include:
The size and number of osteophytes can show how severe OA symptoms are. Bigger osteophytes might mean more advanced disease. This could lead to more pain and less mobility.
Studies have shown that osteophyte size and number are linked to joint space narrowing and pain levels.
An X-ray image can help see osteophytes in osteoarthritis:
Osteophyte formation is vital for diagnosing and tracking OA. Knowing where, how they look, and what they mean is key to managing knee OA well.
Subchondral sclerosis is a key part of knee osteoarthritis. It shows up as denser bones on X-rays. This is a big sign of the knee joint’s degeneration. We’ll look at how it looks on X-rays, why it happens, and how it gets worse. This will help us understand its role in diagnosing and treating osteoarthritis.
On X-rays, subchondral sclerosis looks like whitened areas because of denser bones. These changes happen in the parts of the knee that bear weight. The radiographic appearance is key for figuring out how bad osteoarthritis is. X-rays help us see these changes and judge the severity.
The reasons for subchondral sclerosis are tied to how stress is spread out in the knee. As osteoarthritis gets worse, the joint can’t handle shock and load well. This puts more stress on the bone below, making it harder.
Subchondral sclerosis gets worse over time if not treated. As osteoarthritis gets worse, the bone changes get more severe. This makes the joint worse overall. Knowing this helps doctors come up with better treatment plans.
Spotting subchondral sclerosis on X-rays helps doctors manage knee osteoarthritis better. This can slow down the disease and help patients feel better.
Subchondral bone cysts are a key sign of advanced osteoarthritis. They are fluid-filled cavities in the bone. X-rays can show these cysts, helping doctors diagnose and plan treatment.
These cysts form when synovial fluid gets into the bone through cartilage fissures. This happens when joint pressure goes up and cartilage wears down. On X-rays, they look like clear, round spots in the bone.
“The presence of subchondral bone cysts is a significant indicator of advanced osteoarthritis,” experts say. These cysts are not just random findings. They are closely tied to how severe and how fast the disease gets worse.
Subchondral bone cysts are important because they show how the disease is getting worse. Research shows that bigger cysts mean more severe symptoms and less ability to function. This shows why it’s key to watch how these cysts grow in managing osteoarthritis.
In summary, subchondral bone cysts are a major sign of advanced osteoarthritis, seen on X-rays. They play a big role in how the disease gets worse. Knowing how they form and what they mean is vital for doctors to make good treatment plans.
Knee osteoarthritis often shows uneven degeneration on x-rays. This is key to understanding how the disease progresses and how severe it is. Asymmetric joint space loss means the space between the bones in the knee narrows unevenly. This can cause many problems.
Asymmetric joint space loss can cause the knee to become misaligned. There are two main types: varus and valgus deformities. Varus malalignment makes the knee bow outward, stressing the inner knee. On the other hand, valgus malalignment makes the knee bow inward, stressing the outer knee.
The extent of asymmetric joint space loss affects how doctors plan treatment for knee osteoarthritis. Knowing how much the joint space has narrowed and how the knee is aligned helps doctors choose between non-surgical and surgical options.
Important factors include:
For example, those with severe asymmetric joint space loss and malalignment might need surgery like osteotomy or knee replacement. Accurate x-ray assessments are vital for finding the best treatment plan.
Understanding knee osteoarthritis needs a good classification system. The Kellgren-Lawrence classification is key. It’s a radiographic grading system used by doctors to see how bad osteoarthritis is in the knee.
The Kellgren-Lawrence classification rates osteoarthritis from 0 to 4. This scale shows how the disease progresses. Here’s how it works:
The Kellgren-Lawrence classification helps doctors decide how to treat knee osteoarthritis. By looking at X-rays, doctors can choose the best treatment. This could be non-surgical or surgery.
For example, those with lower grades (0-2) might get physical therapy and medicine. But, those with higher grades (3-4) might need surgery.
Even though the Kellgren-Lawrence classification is helpful, it has its downsides. It mainly looks at X-ray findings. These might not always match the patient’s symptoms or how well they can move.
It also doesn’t consider soft tissue changes or other factors that can affect how the disease shows up. Yet, the Kellgren-Lawrence classification is a key tool for doctors. It helps them understand how severe the disease is and track how it changes over time.
There are more ways to see knee osteoarthritis than just X-rays. X-rays show the basics of joint wear, but other methods give deeper insights. They help us see how soft tissues and bones are affected.
Magnetic Resonance Imaging (MRI) is great for soft tissue damage in knee osteoarthritis. We use MRI to check cartilage loss, meniscal tears, or ligament injuries not seen on X-rays.
A study in the Journal of Orthopaedic Research shows MRI’s role in early osteoarthritis detection. This allows for quicker treatment.
“MRI has become an essential tool in the assessment of knee osteoarthritis, providing detailed images of both bone and soft tissue.”
An MRI can help in:
|
Imaging Modality |
Primary Use in Knee OA |
Benefits |
|---|---|---|
|
MRI |
Soft tissue assessment |
Detailed images of cartilage, menisci, and ligaments |
|
CT Scan |
Bone structure evaluation |
High-resolution images of bone density and structure |
|
Ultrasound |
Soft tissue and joint assessment |
Dynamic assessment of joint and soft tissue pathology |
Computed Tomography (CT) scans are good for bone density and subchondral bone changes. Ultrasound checks soft tissue and joint issues.
CT scans are useful for:
Ultrasound is great for:
The future of osteoarthritis imaging looks promising. We’ll see more advanced and functional methods. These will give detailed info on joint health and disease.
New technologies, like artificial intelligence-enhanced imaging, will improve diagnosis. They will also help tailor treatments for knee osteoarthritis patients.
Understanding your osteoarthritis knee x ray results is key for diagnosis and treatment. We’ve talked about the main signs of OA seen on X-rays. These include joint space narrowing, osteophyte formation, subchondral sclerosis, and subchondral bone cysts.
An xray of oa knee gives important info about how severe osteoarthritis is. This helps doctors decide on the best treatment. By looking at your knee oa xray, doctors can see how bad the condition is. Then, they can make a good treatment plan.
We’ve also stressed the need for the right technique in knee OA radiographic assessment. This includes standard views and weight-bearing images. Knowing what your osteoarthritis knee x ray shows helps you understand your treatment options. It also lets you work with your healthcare provider to manage your condition.
X-ray imaging is key in diagnosing knee osteoarthritis. It shows signs like joint space narrowing and bone changes. These signs help doctors understand the disease’s severity.
For a knee OA radiographic assessment, three views are needed. These include anteroposterior (AP), lateral, and skyline views. Weight-bearing images are also essential for accurate assessment.
Joint space narrowing is a key indicator of cartilage loss in osteoarthritis. The severity of this narrowing often matches the pain and mobility issues patients face.
Osteophyte formation is a hallmark of osteoarthritis. The size and location of these bone spurs can show how severe the disease is and its impact on symptoms.
Subchondral sclerosis is increased bone density in osteoarthritis. It appears as whitened areas on X-rays. This change is due to disease progression and biomechanical changes.
MRI is considered when soft tissue details are needed. This includes ligaments and menisci. It’s also used when X-ray findings are unclear.
The Kellgren-Lawrence system grades knee osteoarthritis severity. It ranges from Grade 0 (normal) to Grade 4 (severe). It helps in deciding treatment options.
Asymmetric joint space loss indicates malalignment. This affects treatment planning. It may require corrective surgery or joint replacement.
X-ray imaging is cost-effective and accessible. It provides valuable information on bone and joint changes. It’s essential for diagnosing and managing osteoarthritis.
Yes, the Kellgren-Lawrence system has limitations. It relies only on radiographic findings. It may not fully capture the disease’s complexity or symptoms in all patients.
Other imaging modalities like MRI, CT scans, and ultrasound can assess knee osteoarthritis. Each provides unique information on different disease aspects.
Osteoarthritis can severely impact patients over 45. It causes chronic pain, limits mobility, and affects daily activities. Effective management strategies are needed.
https://my.clevelandclinic.org/health/diseases/21750-osteoarthritis-knee
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!