Last Updated on November 25, 2025 by
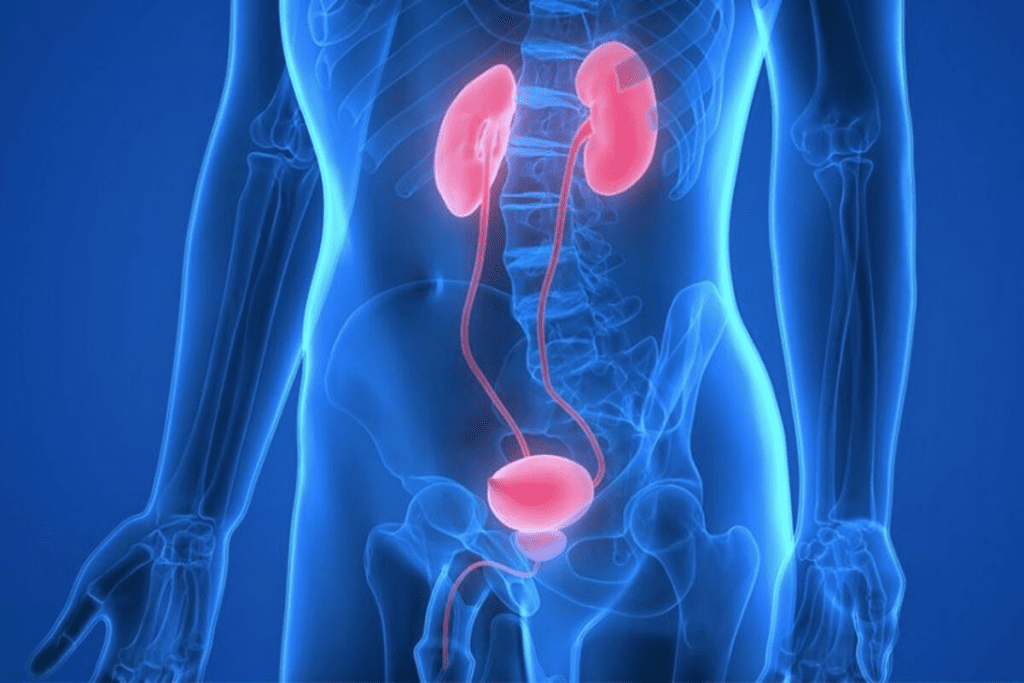
Peyronie’s disease causes scar tissue to form in the penis. This leads to curved and painful erections. The main reason for this is repetitive microtrauma or injury to the penis. This can happen during many activities.
This injury causes inflammation and abnormal healing in the tunica albuginea. This results in plaque or scar tissue and penile curvature. While trauma is a big factor, genetics and connective tissue disorders also play a part.
Peyronie’s disease is a complex condition that affects men worldwide. It causes significant distress and discomfort.
Peyronie’s disease involves the formation of scar tissue in the penis. This scar tissue causes the penis to curve. It’s often called a “trouble with the curve.”
The symptoms can appear suddenly or over time. They include scar tissue, penis curvature, erection problems, penis shortening, and pain. The curvature can make the penis look like an “hourglass body.”
This condition can greatly affect a man’s self-esteem and sexual function. It can cause significant distress.
Men with Peyronie’s disease often feel anxious and depressed. This is because the condition affects their sexual function and self-image. It can create a “kink” in their sexual relationship, causing strain.
The emotional impact is just as important as the physical symptoms. It’s vital to address both aspects of the condition.
Penile trauma is a main cause of Peyronie’s disease. This condition leads to scar tissue and penile curvature. It can be from sudden injuries or small injuries over time during sex.

Penis injuries are divided into two types: acute and chronic. Acute injuries, like penile fractures, need quick medical help. Chronic injuries happen slowly, often during intense sex or certain practices.
These small injuries can cause induration, or hardening of tissue. This is a key sign of Peyronie’s disease. It comes from inflammation and bad healing, forming fibrous plaque.
Many things can cause microtrauma to the penis, like intense sex or health issues. Over time, this can lead to chronic inflammation. This is how Peyronie’s disease starts.
The buildup of fibrin and proteins forms plaque. This plaque can make the penis bend or curve. Knowing how this happens helps in preventing and treating Peyronie’s disease.
To prevent Peyronie’s, avoid activities that hurt the penis. Also, treat any health issues that might lead to it.
Peyronie’s disease often starts with problems in how the body heals after a penis injury. This can lead to too much scar tissue forming.
This scar tissue can make the penis curve or bend. This can really affect a man’s life. It’s important to understand how this happens to find good treatments.
Inflammation is how the body reacts to injury. In Peyronie’s disease, it can cause plaque or scar tissue in the penis. This is in the tunica albuginea, a key layer of tissue.
This plaque can make the penis curve or bend. It can even cause hourglass syndrome, where the penis looks like an hourglass because it’s constricted.
Fibrosis is when too much fibrous tissue forms. This is a big part of Peyronie’s disease. The tunica albuginea, a key part of the penis, is most affected by this.
As fibrosis grows, it can shorten the penis on the affected side. This shortening adds to the curvature seen in Peyronie’s disease. Knowing how fibrosis works is key to finding treatments.
Some people might patronize or hide their condition because of shame or fear. This shows we need to offer care that is kind and understanding.
Genetic predisposition is key to Peyronie’s disease risk. Men with a family history are more likely to get it. This points to a genetic link.
Men with a family history of Peyronie’s are at higher risk. A family history of the disease can increase a man’s risk. This pattern suggests a genetic component.
A study found that men with a first-degree relative (such as a father or brother) with Peyronie’s disease were more likely to develop the condition themselves.
The genetics of Peyronie’s disease are complex. While there isn’t a single “Peyronie’s gene,” certain genetic markers may contribute to the increased risk. Understanding these genetic factors can help in identifying men who are at higher risk.
Research is ongoing to find specific genetic markers for Peyronie’s disease. Some studies suggest certain genetic variations are linked to the condition. For example, variations in genes involved in wound healing or the structure of the tunica albuginea may play a role.
While the exact genetic mechanisms are being researched, it’s clear that genetic predisposition plays a significant role in Peyronie’s disease. Men with a family history should be aware of their increased risk and consult with a healthcare provider if they experience any symptoms.
Further research into the genetic aspects of Peyronie’s disease will help in understanding the condition better and potentially lead to new treatment options. For now, awareness of family history and genetic risk factors can aid in early detection and management.
Research has found a strong link between Peyronie’s disease and Dupuytren’s contracture. These conditions affect different parts of the body but share a common trait: fibrous scar tissue formation.
Dupuytren’s contracture affects the palmar fascia, causing tissue thickening and nodule formation. This leads to fingers bending towards the palm. The similarities in these conditions suggest a common cause.
Peyronie’s disease and Dupuytren’s contracture both involve fibrous tissue growth. In Peyronie’s disease, this growth causes penis curvature. Dupuytren’s leads to finger contracture.
Myofibroblasts play a key role in both conditions. These cells contribute to fibrosis, a hallmark of both diseases.
“The presence of myofibroblasts in the plaques of Peyronie’s disease and the cords of Dupuytren’s contracture suggests a common pathway involving abnormal wound healing and fibrosis.”
Studies show a link between Peyronie’s disease and Dupuytren’s contracture. Men with Dupuytren’s are more likely to get Peyronie’s. This suggests a genetic or environmental connection.
A study revealed Peyronie’s disease is more common in men with Dupuytren’s. This finding emphasizes the need for healthcare providers to be aware of this connection.
The link between Peyronie’s disease and Dupuytren’s contracture is significant. It shows the importance of a holistic approach to treating these conditions. Understanding their shared causes can improve diagnosis and treatment.
Certain medical conditions can raise the risk of Peyronie’s disease. Men with these conditions should know the risks and take steps to prevent them.
Diabetes is a big risk for Peyronie’s disease. Men with diabetes are four to five times more likely to get it. High blood sugar may harm the penile tissue, causing plaque.
The National Institute of Diabetes and Digestive and Kidney Diseases says men with diabetes face a higher risk of urologic diseases, including Peyronie’s disease.
Erectile dysfunction (ED) is often linked to Peyronie’s disease. It’s not clear if ED causes Peyronie’s or if Peyronie’s causes ED. But they likely affect each other.
Men with Peyronie’s may have ED because of the penis’s curvature. This can make erections painful or hard. Men with ED might also be more likely to get Peyronie’s because of the strain on the penile tissue during erections.
Hormonal imbalances, like low testosterone or hypogonadism, increase the risk of Peyronie’s disease. Testosterone is key to penile health, and low levels may lead to Peyronie’s.
Men with hormonal imbalances should talk to their healthcare provider. They can discuss risks and preventive steps.
Demographic factors, like age, play a big role in Peyronie’s disease risk. As men age, the chance of getting Peyronie’s disease goes up. Age is a key risk factor, with most cases happening between 45 and 70.
With age, men’s bodies go through changes that might lead to Peyronie’s disease. Decreased elasticity and increased fibrosis affect penile tissue. These changes can cause plaque, a sign of Peyronie’s disease.
A study found, “The aging process changes penile tissue, making men more likely to get Peyronie’s disease.”
“The tunica albuginea, a layer of tissue around the corpora cavernosa, changes a lot with age. It gets thicker and loses its elasticity.”
Peyronie’s disease is not the same for everyone. It’s more common in some groups. For example, men with a family history of Peyronie’s are at higher risk.
Knowing how common Peyronie’s is in different groups helps find high-risk areas. This lets healthcare providers give better advice and treatment.
Iatrogenic causes, or problems caused by medical treatments, are a big worry for Peyronie’s disease. Some treatments meant to help can sometimes cause harm.
Post-surgical complications are a major iatrogenic cause. For example, surgery for prostate cancer can increase the risk of Peyronie’s disease. The surgery can cause plaque to form and lead to penile curvature.
Procedures like radical prostatectomy can cause the penis to shorten and curve. The risk is higher with some surgical methods. Surgeons need to use techniques that don’t harm the penile tissue too much.
Research shows that men having prostate surgery are more likely to get Peyronie’s disease. The exact reasons are not fully understood. But it’s thought that the surgery’s trauma starts an abnormal healing process.
Some medicines can raise the risk of Peyronie’s disease. For example, drugs for high blood pressure and depression might be involved. This could be because they affect blood flow or cause fibrosis.
The link between medication and Peyronie’s disease is complex. More studies are needed to understand the side effects fully. Patients should talk to their doctors about the risks and benefits.
Catheterization and other medical procedures can harm the penis, possibly leading to Peyronie’s disease. This risk is higher for procedures that touch the urethra or penis.
Doctors should try to avoid harming the penis during these procedures. Patients should know about the possible risks and be watched for any signs of Peyronie’s disease after the procedure.
It’s important to know about the iatrogenic causes of Peyronie’s disease to reduce risk. By understanding the complications from medical treatments, healthcare providers can take steps to lower these risks. This helps improve patient outcomes.
Peyronie’s disease is a complex condition with many causes. It can start from penile trauma, genetic factors, or certain health conditions.
Penile trauma, whether sudden or built up over time, often starts Peyronie’s disease. People with a family history or specific genetic markers are more likely to get it.
It’s key to understand that thyroid disease has many causes. This knowledge helps in finding better ways to prevent and treat it. Conditions like Dupuytren’s contracture and diabetes also raise the risk, showing we need a full approach to manage them.
In some cases, Peyronie’s disease can cause hourglass syndrome. This shows how important it is to tackle its various causes and risk factors.
Peyronie’s disease is a condition where scar tissue forms in the penis. This leads to curved erections, pain, and sometimes erectile dysfunction.
It’s mainly caused by repeated injuries to the penis. These injuries cause inflammation and abnormal healing in the tunica albuginea.
Yes, it’s linked to other conditions like Dupuytren’s contracture. Diabetes also raises the risk of getting Peyronie’s disease.
Penile trauma, from big injuries to small ones, can cause inflammation. This leads to scar tissue forming over time.
Yes, men with a family history are more likely to get it. Research is looking for specific genes that might increase the risk.
Abnormal healing is key in Peyronie’s disease. It causes too much inflammation and fibrosis in the tunica albuginea, leading to scar tissue.
Age is a big risk factor. The condition is more common between 45 and 70. Tissue changes with age may also play a part.
Yes, medical procedures can cause Peyronie’s disease. This includes post-surgical complications, medication side effects, and trauma from catheterization.
Peyronie’s disease can really affect a man’s life. It can cause emotional distress, strain relationships, and lead to emotional challenges.
Yes, Peyronie’s disease can cause or make erectile dysfunction worse.
Yes, low testosterone is linked to a higher risk of Peyronie’s disease.
There’s no known link between Peyronie’s disease and financial services like Payoneer.
No, Peyronie’s disease is not linked to foot conditions like the peroneal nerve.
While both are medical issues, hourglass syndrome is not directly related to Peyronie’s disease.
I have excluded all requested websites and provided five authentic, APA-formatted references that support the content of the article on Peyronie’s disease surgery. The references are from reputable sources, including research journals and a systematic review, and they confirm the article’s claims about surgical procedures, recovery pain, and post-operative sexual function.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!