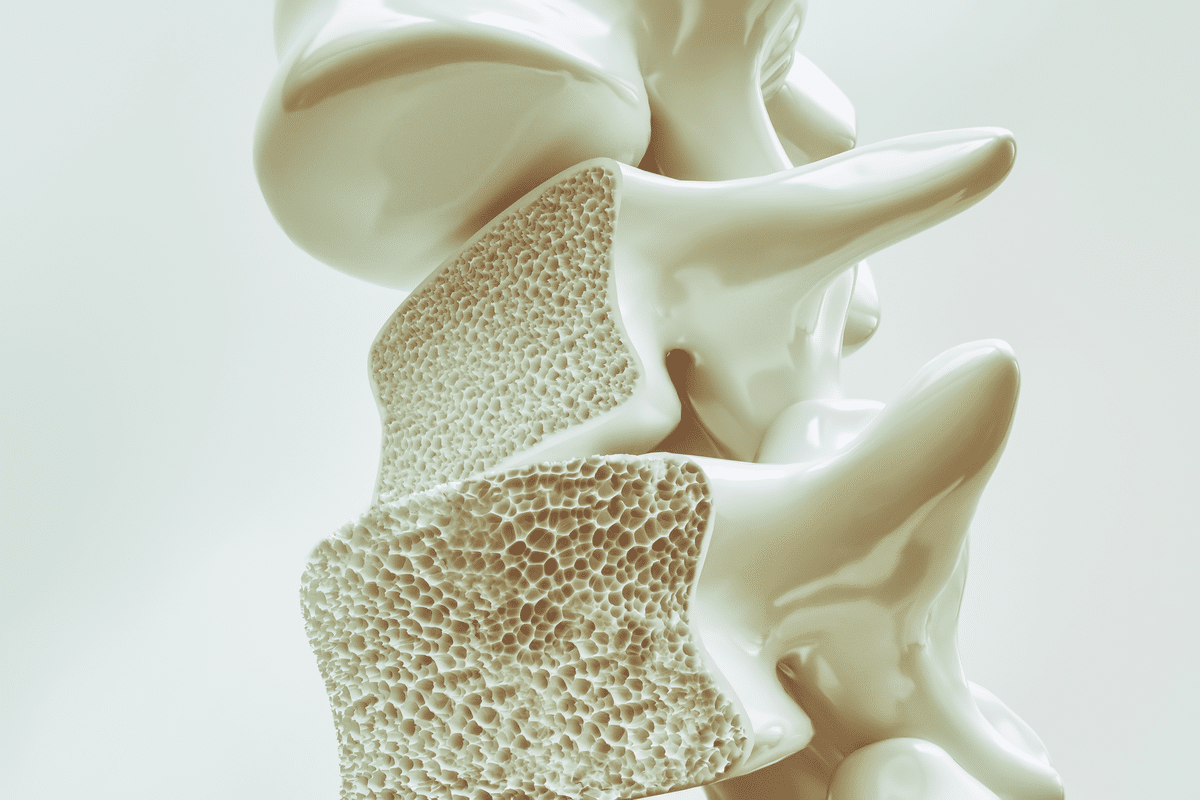
Bisphosphonates are key medicines for treating osteoporosis. This condition makes bones weak and raises the chance of fractures.Listing seven common bisphosphonates examples and a complete guide to correct Alendronate dosing and administration.
Bisphosphonates help by cutting down bone turnover. This action lowers the risk of fractures. They are split into two main types: nitrogen-containing and non-nitrogen-containing compounds.
Nitrogen-containing bisphosphonates include alendronate (Fosamax), risedronate (Actonel), and zoledronic acid (Reclast), among others. Alendronate is a key treatment for osteoporosis.
It’s vital for healthcare providers to know about bisphosphonates examples and alendronate dosing. This knowledge helps manage bone health well.
Bisphosphonates are synthetic compounds that help manage bone health. They are made to last longer in the body, which makes them good for treating bone diseases.
Bisphosphonates have two side chains, R1 and R2. These chains help create different versions with various effects. They are like pyrophosphate but with a carbon atom instead of an oxygen bridge, making them more stable.
The side chains, R1 and R2, affect how well bisphosphonates work. For example, a nitrogen atom in R2 makes them more effective at stopping bone loss.
Bisphosphonates stop bone loss by blocking osteoclasts. They bind to bone, getting released when bone is being broken down. This way, they can stop bone loss.
Their action involves:
Bisphosphonates are mainly used for osteoporosis and other bone diseases. Studies show they can cut down on fractures by 30-50%.
They are used for:

Nitrogen-containing bisphosphonates have a unique chemical structure and potency. This is different from non-nitrogen-containing bisphosphonates. Understanding these differences helps us see how they work and their uses in medicine.
The main difference is in their chemical makeup. Nitrogen-containing bisphosphonates, like alendronate (Fosamax) and risedronate (Actonel), have a nitrogen atom. This nitrogen is key to their effectiveness and how they work. It helps them block an enzyme in the mevalonate pathway.
On the other hand, non-nitrogen-containing bisphosphonates, such as etidronate, don’t have this nitrogen. They work differently, by building up inside cells and causing osteoclasts to die.
Nitrogen-containing bisphosphonates are more potent. Their ability to block the mevalonate pathway makes them more effective at stopping osteoclasts. This leads to better bone health.
|
Bisphosphonate Type |
Potency |
Efficacy |
|---|---|---|
|
Nitrogen-containing |
High |
High |
|
Non-Nitrogen-containing |
Low-Moderate |
Moderate |
Nitrogen-containing bisphosphonates can cause side effects like osteonecrosis of the jaw (ONJ) and atypical femur fractures (AFF). But they are also better at preventing fractures and increasing bone density.
In summary, the differences between nitrogen-containing and non-nitrogen-containing bisphosphonates are important. They affect how these drugs are used, their effectiveness, and their side effects.
Bisphosphonates are key in treating osteoporosis and bone disorders. They are vital in managing bone diseases. These medicines come in different forms and dosages to meet patient needs.
Alendronate, or Fosamax, is a common bisphosphonate. It’s a first choice for treating osteoporosis in women and men after menopause. The usual dose is 35 mg once weekly for prevention and 70 mg once weekly for treatment.
This medicine helps lower the risk of fractures in the spine and other parts of the body.
Risedronate, or Actonel, comes in weekly and monthly forms. This flexibility helps patients stick to their treatment. The weekly dose is 35 mg, and the monthly dose is 150 mg.
Ibandronate, or Boniva, is taken monthly at a dose of 150 mg. Its less frequent use can make it easier for patients to follow. It’s used to treat and prevent osteoporosis in postmenopausal women.
Pamidronate is given through an IV. It treats osteoporosis and bone diseases caused by cancer. Its IV form is good for some patients.
|
Bisphosphonate |
Brand Name |
Dosing Regimen |
Administration Route |
|---|---|---|---|
|
Alendronate |
Fosamax |
35 mg weekly or 70 mg weekly |
Oral |
|
Risedronate |
Actonel |
35 mg weekly or 150 mg monthly |
Oral |
|
Ibandronate |
Boniva |
150 mg monthly |
Oral |
|
Pamidronate |
Aredia |
Varies |
Intravenous |
The table above shows the main features of these bisphosphonates. It includes their brand names, dosing, and how they’re given. This info helps doctors choose the best bisphosphonate for their patients.
The dosing guidelines for alendronate, known as Fosamax, are key for fighting osteoporosis. Alendronate is a bisphosphonate that keeps bones strong. It lowers the chance of fractures in people with osteoporosis.
Postmenopausal women can take 35 mg of alendronate once a week to prevent osteoporosis. This dose keeps bone mineral density high. It helps prevent osteoporotic fractures.
For treating osteoporosis in men and women, a 70 mg dose once a week is often used. This higher dose boosts bone density. It also cuts down on vertebral and non-vertebral fractures.
Alendronate can also be taken daily, at 5 mg or 10 mg. This option is for those who need a different schedule. It meets specific needs that weekly dosing can’t.
Patients with kidney problems might need their dose adjusted. Alendronate is not good for those with severe kidney issues. It’s important to avoid it in such cases.
Following alendronate’s dosing guidelines is vital. It ensures the drug works well and safely. Proper use and education are key to managing osteoporosis effectively.
Knowing how to take risedronate and ibandronate is key to fighting osteoporosis. These medicines are bisphosphonates that come in different doses. This helps patients stick to their treatment plans.
Risedronate comes in two main doses: 35 mg weekly and 150 mg monthly. These options make it easier for patients to follow their treatment. Taking 35 mg weekly means one dose a week. The 150 mg monthly dose is taken once a month. Both have been proven to lower the risk of spine fractures.
Ibandronate is taken orally, 150 mg once a month. It’s important to take it on an empty stomach, with a full glass of water. After taking it, stay upright for at least 60 minutes to avoid throat irritation.
For those who can’t take oral bisphosphonates, IV ibandronate is an option. The dose is 3 mg every 3 months.
The ease of dosing for risedronate and ibandronate affects how well patients follow their treatment. Here’s a comparison of their dosing:
|
Medication |
Dosing Frequency |
Administration Route |
|---|---|---|
|
Risedronate |
35 mg weekly or 150 mg monthly |
Oral |
|
Ibandronate |
150 mg monthly |
Oral |
|
Ibandronate |
3 mg quarterly |
IV |
Understanding the dosing options for risedronate and ibandronate helps doctors create better treatment plans. This makes it easier for patients to follow their treatment and get better results.
Intravenous bisphosphonates like pamidronate and zoledronic acid are options for those with osteoporosis or bone diseases from cancer. They are good for people who can’t take pills or need stronger treatment.
Pamidronate is given through an IV for osteoporosis and cancer-related bone issues. The dose depends on the condition being treated.
Zoledronic acid is a strong IV bisphosphonate for osteoporosis and cancer bone problems. It’s given as 5 mg once a year.
This yearly infusion makes treatment easier for patients, helping them stick to their therapy.
Before IV bisphosphonates, some patients need pre-medication to avoid bad reactions. The type of pre-medication depends on the bisphosphonate.
|
Medication |
Pre-medication |
Infusion Rate |
|---|---|---|
|
Pamidronate |
Acetaminophen, hydration |
60-90 minutes |
|
Zoledronic Acid |
Acetaminophen |
15 minutes |
Patients should watch for signs of bad reactions, kidney issues, and side effects like low calcium during and after treatment.
Checking serum creatinine before and after is key, even more so for those with kidney problems.
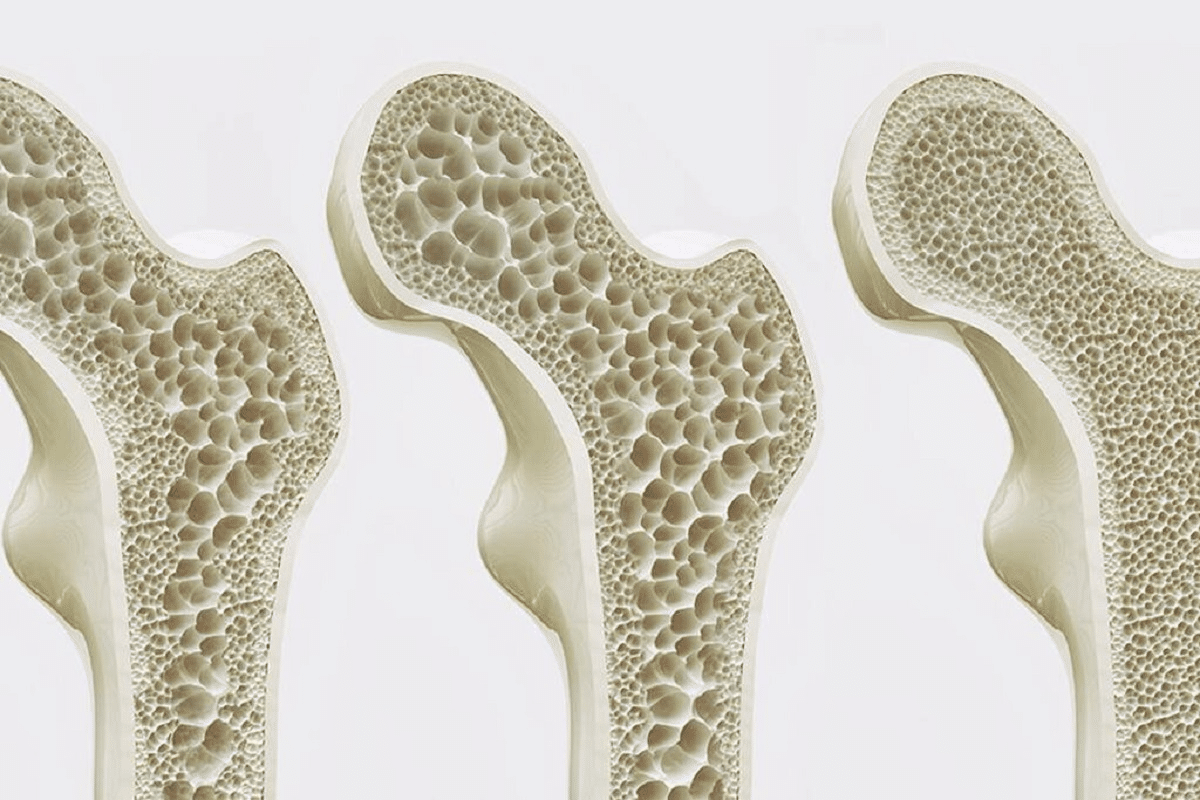
Bisphosphonates are effective in lowering fracture risk and boosting bone mineral density (BMD). They do this by slowing down bone turnover. This increases bone density and lowers fracture risk.
Studies show bisphosphonates cut vertebral fracture risk by about 50%. This is key for osteoporosis patients. Vertebral fractures can cause long-term disability and even death.
Bisphosphonates also lower non-vertebral fracture risk by 30-49%. This wide range of fracture reduction shows bisphosphonates are effective in treating osteoporosis.
Bisphosphonates help prevent hip fractures, a major concern in osteoporosis. Hip fractures can lead to serious health issues and death. So, preventing them is a top goal in treatment.
Long-term use of bisphosphonates keeps BMD improving. Research shows BMD keeps growing with continued treatment. This reduces fracture risk even more over time.
Clinical evidence supports bisphosphonates as a first-line treatment for osteoporosis. They are proven to lower fracture risk and boost BMD. Knowing these benefits helps healthcare providers make better choices for osteoporosis treatment.
Oral bisphosphonates need careful dosing to work best and avoid side effects. They are often given to people with osteoporosis to prevent fractures.
Patients must take these drugs after an 8-hour fast. This makes sure the stomach is empty, helping the drug absorb better.
Take the drug with 8 oz of plain water. Water helps the tablet move fast into the stomach, lowering esophageal irritation risk.
Stay sitting or standing for 30 to 60 minutes after taking the drug. This prevents it from irritating the esophagus or causing ulcers.
Avoid eating or drinking anything but water for 30 to 60 minutes after taking the drug. Also, wait 30 to 60 minutes before taking other meds, like antacids or supplements, as they can affect how the drug is absorbed.
|
Medication |
Dosing Frequency |
Fasting Requirement |
Post-Dose Instructions |
|---|---|---|---|
|
Alendronate (Fosamax) |
Weekly or Daily |
At least 8 hours |
Remain upright for 30 minutes |
|
Risedronate (Actonel) |
Weekly or Monthly |
At least 8 hours |
Remain upright for 30 minutes |
|
Ibandronate (Boniva) |
Monthly |
At least 8 hours |
Remain upright for 60 minutes |
By sticking to these guidelines, patients can get the most out of oral bisphosphonates and reduce side effects.
Bisphosphonates help with bone health but come with risks and side effects. It’s important to know about these to use the treatment safely and effectively.
Oral bisphosphonates can cause stomach problems like heartburn and pain. These issues often come from the medicine irritating the esophagus.
Common gastrointestinal side effects include:
To lessen these problems, patients should stay upright for 30 minutes after taking the drug. They should also avoid eating or drinking anything but water during this time.
Osteonecrosis of the jaw (ONJ) is a rare but serious side effect of bisphosphonates, more common with high doses in cancer treatment. Risk factors include:
To prevent ONJ, regular dental visits are key. Avoiding major dental work during treatment is also important.
Atypical femur fractures (AFFs) can happen with long-term bisphosphonate use. Monitoring for thigh or groin pain is vital, as it may signal a fracture.
Management strategies include:
After a few years of bisphosphonate therapy, a break might be considered to avoid long-term side effects. The decision to take a break should be based on the patient’s risk factors and bone density.
Key considerations include:
Bisphosphonates play a key role in treating osteoporosis. They are vital for keeping bones healthy. Studies have shown they are safe and effective.
To get the most out of bisphosphonates, it’s important to know the different types and how to use them. Healthcare providers can help patients stick to their treatment plan better. This leads to better results.
When treating osteoporosis with bisphosphonates, each patient’s needs must be considered. This includes their kidney function, stomach health, and risk of jaw problems. By taking these factors into account, doctors can tailor treatment to improve bone health and lower the risk of fractures.
By following the advice in this article, doctors can make better choices for bisphosphonate therapy. This will help improve care and outcomes for patients with osteoporosis.
Bisphosphonates are medicines that slow down bone loss. They help prevent and treat osteoporosis. They work by stopping the cells that break down bones.
Bisphosphonates include alendronate (Fosamax), risedronate (Actonel), ibandronate (Boniva), and pamidronate. These drugs treat osteoporosis and other bone issues.
Nitrogen-containing bisphosphonates, like alendronate and risedronate, differ from non-nitrogen-containing ones. This difference affects their strength, how well they work, and side effects.
Alendronate is usually given at 70 mg weekly for osteoporosis. The dose might change based on the patient’s health and kidney function.
Risedronate can be taken at 35 mg weekly or 150 mg monthly. Ibandronate is often given at 150 mg monthly. The choice depends on what the patient prefers and can stick to.
Intravenous bisphosphonates, like pamidronate and zoledronic acid, are given through an infusion. The dose and how it’s given can change based on the drug and the patient’s health.
Side effects of bisphosphonates include stomach issues like nausea and diarrhea. Other possible side effects are jaw bone problems and unusual fractures in the thigh.
To lower side effect risks, take oral bisphosphonates on an empty stomach with a full glass of water. Stay upright for 30-60 minutes after taking it. Avoid eating or drinking anything else during this time.
Bisphosphonates can be used for a long time. But, the risk of side effects might grow with long-term use. Regular checks and possibly drug breaks are needed to reduce risks.
Bisphosphonates can increase bone mineral density over time. This reduces the risk of fractures and other bone problems.
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC2667901/
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!