
Autoimmune diseases are a group of conditions where the immune system attacks the body’s own tissues. This leads to various autoimmune disease symptoms and signs of autoimmune disease.Answering can you have an autoimmune disease with normal blood work (yes) and explaining the importance of clinical symptoms.
Many people have persistent and unexplained symptoms like chronic joint pain, fatigue, and recurring fevers. Yet, their blood tests show nothing wrong. This is known as being seronegative, making diagnosis hard for doctors.
It’s important to know that normal blood work doesn’t mean you can’t have an autoimmune condition. Recent studies show many patients have symptoms of autoimmune disorders even with normal lab results for a long time.
Autoimmune diseases happen when the body’s immune system attacks itself. This can harm cells, tissues, and organs. Knowing about these diseases and how to diagnose them is key to managing and treating them.
An autoimmune disease is when the immune system mistakenly attacks the body’s own tissues. This can cause many health problems, depending on what part of the body is affected. For example, conditions like rheumatoid arthritis, lupus, and Hashimoto’s thyroiditis are all autoimmune diseases. Each has its own symptoms and effects on the body.
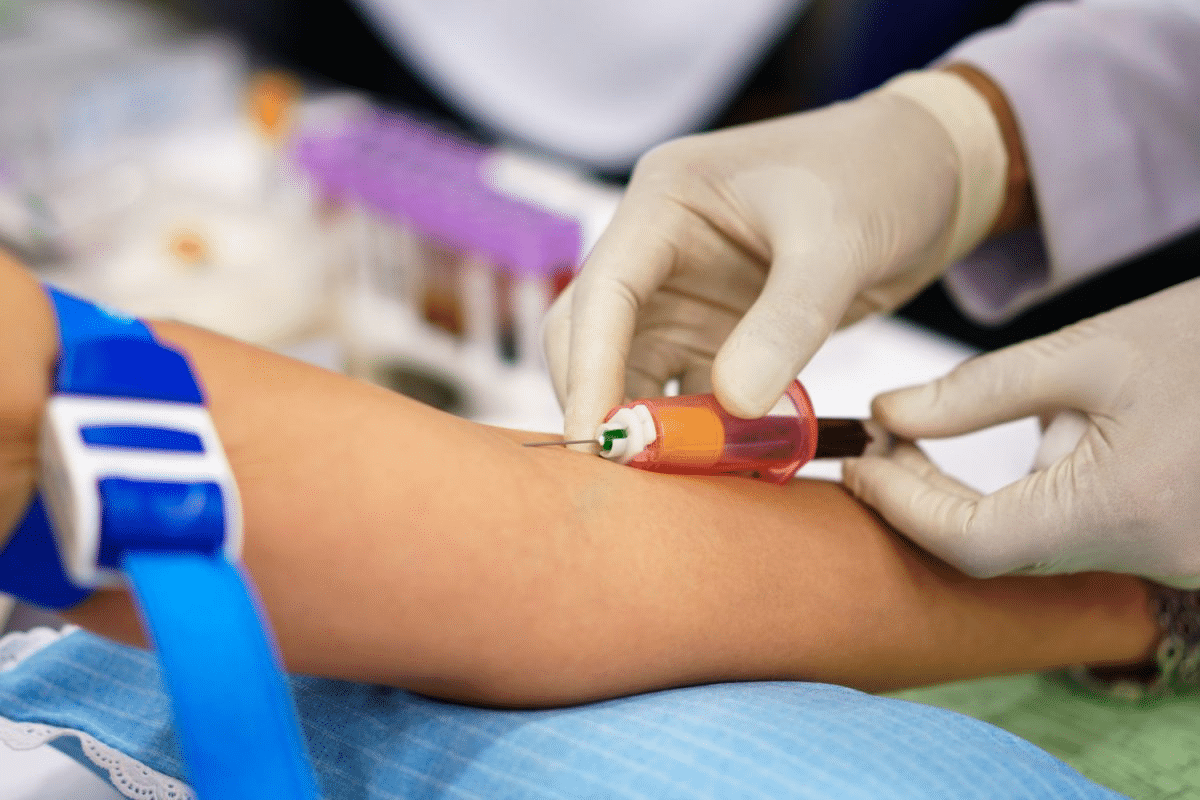
Diagnosing autoimmune diseases usually involves a few steps. These include a doctor’s evaluation, looking at the patient’s history, and running tests. Blood tests are a big part of this process.
Blood tests for diagnosing autoimmune diseases include:
These tests help find inflammation, specific autoantibodies, and other signs of autoimmune activity.
|
Blood Test |
Purpose |
Indicators |
|---|---|---|
|
Complete Blood Count (CBC) |
Evaluate overall health and detect a range of disorders |
Abnormal counts of red and white blood cells, platelets |
|
Comprehensive Metabolic Panel |
Assess metabolic function and detect issues in various organs |
Electrolyte levels, blood sugar, kidney and liver function |
|
Inflammatory Markers (CRP and ESR) |
Measure inflammation in the body |
Elevated CRP and ESR levels indicate inflammation |
|
Autoantibody Tests |
Detect specific autoantibodies associated with autoimmune diseases |
Presence of autoantibodies like ANA, RF, and anti-TPO |
Having normal blood work doesn’t mean you can’t have an autoimmune disease. This is called being seronegative. It means you test negative for the autoantibodies usually found in these diseases.
Seronegative autoimmune conditions are tricky to diagnose. People show symptoms of an autoimmune disease but their blood tests don’t show the usual autoantibodies. This makes it hard to diagnose because many tests look for these antibodies.
Key characteristics of seronegative autoimmune conditions include:
Blood tests are key in diagnosing diseases, but they’re not perfect. Several reasons can lead to normal blood work even with an autoimmune disease:
Research shows many people with autoimmune diseases are seronegative. For example:
These numbers show why doctors need to look at symptoms and other tests, not just blood work, when checking for autoimmune diseases.
Several common blood tests help diagnose autoimmune diseases. These tests check for the presence and severity of these conditions.
A Complete Blood Count (CBC) checks different parts of the blood. It looks at red and white blood cells, hemoglobin, and platelets. It can spot issues linked to autoimmune diseases.
The Comprehensive Metabolic Panel checks many aspects of metabolism. It looks at liver and kidney function, electrolytes, and blood sugar. It gives insights into overall health and organ involvement in autoimmune diseases.
Inflammatory markers like C-Reactive Protein (CRP) and Erythrocyte Sedimentation Rate (ESR) measure body inflammation. High levels suggest an autoimmune or inflammatory condition.
Autoantibody tests are key in diagnosing autoimmune diseases. They find antibodies against the body’s own tissues, typical of autoimmune conditions.
Even if blood tests seem normal, it doesn’t mean you don’t have an autoimmune disorder. Many things can make blood tests look fine even when you have an autoimmune disease.
In the beginning, blood tests might not show anything wrong. This is because the disease might not have made big changes in your blood yet.
Early detection is hard because there aren’t clear signs. So, people might feel sick but their blood tests will look normal.
Antibody levels can change a lot. This means blood tests might not catch all autoantibodies. Even if you have an autoimmune disease, your tests could look normal.
Monitoring over time is key. It helps find autoantibodies when they are active.
Today’s tests can’t find all autoantibodies or markers. This means some autoimmune diseases might not show up on standard blood tests.
When you get blood tested matters a lot. Testing when you’re feeling better or symptoms are mild can make your tests look normal.
Careful consideration of when you get tested is key. Doctors need to look at your whole medical history and symptoms to understand your blood test results.
A negative antinuclear antibody test doesn’t mean you can’t have an autoimmune disease. Early stages, changing antibody levels, and test limits can all lead to normal blood test results.
It’s important to know the symptoms of autoimmune diseases early. These diseases happen when the body attacks itself. The symptoms can change based on the disease and the body part affected.
Many diseases, like rheumatoid arthritis and lupus, affect joints and muscles. Common signs include:
These symptoms can really hurt your ability to move and enjoy life.
Systemic symptoms affect the whole body. Common ones include:
These symptoms can be hard to pinpoint, making diagnosis tricky.
Some diseases target specific organs. For example:
|
Autoimmune Disease |
Organ Affected |
Symptoms |
|---|---|---|
|
Hashimoto’s Thyroiditis |
Thyroid |
Fatigue, weight gain, cold intolerance |
|
Type 1 Diabetes |
Pancreas |
Increased thirst and urination, weight loss |
|
Multiple Sclerosis |
Central Nervous System |
Vision problems, muscle weakness, coordination issues |
Autoimmune diseases often have ups and downs. During flare-ups, symptoms get worse. Knowing these patterns helps manage the disease better.
It’s key to recognize autoimmune disease symptoms early. If you’re experiencing persistent or severe symptoms, see a doctor.
Normal blood tests don’t always mean you don’t have an autoimmune disease. Some conditions can be hidden in the blood. These diseases need a detailed check-up beyond just blood tests.
Rheumatoid arthritis (RA) is usually found through blood tests for rheumatoid factor (RF) or anti-citrullinated protein antibodies (anti-CCP). But, seronegative rheumatoid arthritis doesn’t show these antibodies. Despite this, people with it can have serious joint problems. Doctors use other tests and look at symptoms to diagnose it.
Systemic Lupus Erythematosus (SLE) is a complex disease that can hit many parts of the body. In the beginning, SLE might not show the usual autoantibodies like antinuclear antibodies (ANA). Early systemic lupus erythematosus is hard to spot when blood tests don’t show anything. Doctors have to look at symptoms, medical history, and might need to test again later.
Hashimoto’s thyroiditis is an autoimmune disease that messes with the thyroid, causing hypothyroidism. Sometimes, thyroid antibodies are missing, even in the early stages. Doctors diagnose it by looking at symptoms, thyroid tests, and sometimes, ultrasound.
Seronegative spondyloarthropathies are a set of inflammatory arthritis conditions. They don’t show rheumatoid factor in blood tests. These include ankylosing spondylitis and psoriatic arthritis. Doctors use symptoms, imaging, and specific markers like HLA-B27 to diagnose them.
In summary, many autoimmune diseases can look normal in blood tests. This shows we need a detailed approach to diagnose them. This includes looking at symptoms, using imaging, and sometimes, more advanced tests.
Diagnosing autoimmune diseases needs more than just blood tests. While blood work is helpful, it’s not always enough. Doctors use many tools to find and treat these conditions.
Looking at a patient’s symptoms and medical history is key. Doctors search for signs of autoimmune diseases even when blood tests don’t show anything.
Doctors do physical exams, ask about symptoms, and check medical and family history. This helps find what might be causing the problem.
Imaging studies are also important. X-rays, MRI, and ultrasound show how much damage or inflammation there is.
|
Imaging Technique |
Use in Autoimmune Disease Diagnosis |
|---|---|
|
X-rays |
Assess joint damage and bone erosion |
|
MRI |
Evaluate soft tissue inflammation and damage |
|
Ultrasound |
Examine joint and soft tissue inflammation |
At times, a tissue biopsy is needed. It takes a tissue sample for a microscope check. This can show specific signs of autoimmune diseases.
Functional medicine testing looks at more than just blood work. It checks gut health, nutrient levels, and other factors that might cause autoimmune diseases.
Using these different methods, doctors can understand a patient’s condition better. This helps them create a good treatment plan.
Autoimmune diseases come from a mix of genetics, environment, and lifestyle. Knowing these factors helps spot who’s at risk. It might even stop these diseases before they start.
Genetics are key in getting autoimmune diseases. Some genes make people more likely to get certain conditions. For example, HLA-B27 is linked to ankylosing spondylitis. Scientists are learning more about how genes and autoimmune diseases connect.
Things around us, like chemicals and infections, can start autoimmune diseases in people who are already at risk. For example, silica dust might raise the risk of lupus and rheumatoid arthritis.
Hormones play a big part in autoimmune diseases too. Many diseases are more common in women, hinting at a hormonal link. Conditions like Hashimoto’s thyroiditis and systemic lupus erythematosus often hit women harder.
Stress and lifestyle choices, like diet and exercise, also affect autoimmune diseases. Stress can make symptoms worse. A healthy lifestyle might lower some risks.
Understanding these factors helps doctors and patients manage symptoms. It could even lower the chance of getting autoimmune diseases.
Not knowing what’s causing your symptoms can really affect your mind. It can make you feel frustrated, anxious, and lonely. This is because you’re dealing with symptoms that don’t have a clear cause.
Medical uncertainty is tough for patients. When tests show nothing wrong but you’re not feeling better, it’s hard to get your doctor to listen. This can make you feel like your feelings are being ignored.
A study in the Journal of General Internal Medicine found something interesting. People with symptoms that doctors can’t explain feel more anxious and depressed than those with clear causes.
Autoimmune diseases are often invisible. This means their symptoms aren’t always easy to see. It can be hard for people to get the support they need because of this.
Those with invisible illnesses often feel like no one believes them. They might feel like they’re being seen as too worried about their health. This can make them feel very alone.
It’s important to find people who understand what you’re going through. Support groups, online or in-person, can be a great place to find this. They offer a safe space to share your story and feel heard.
Doctors also play a big role in helping you feel better. By listening to you and working to find a diagnosis, they can help reduce your stress and anxiety.
|
Coping Strategies |
Description |
Benefits |
|---|---|---|
|
Support Groups |
Joining a group of people with similar experiences |
Validation, emotional support, sense of community |
|
Mindfulness Practices |
Engaging in mindfulness meditation or yoga |
Reduced stress, improved mental well-being |
|
Patient Education |
Learning about the condition and its management |
Empowerment, better disease management |
Getting a correct diagnosis often depends on teamwork between patients and healthcare teams. Dealing with autoimmune diseases needs a team effort. Patients and healthcare providers must work together to find the right diagnosis.
Finding the right specialists is a big step. You might need to see different doctors, like rheumatologists for arthritis or endocrinologists for thyroid issues. It’s important to find a specialist who knows about autoimmune diseases. They can spot the small symptoms and order the right tests.
Being persistent is key when looking for a diagnosis. You should speak up and ask questions. Getting a diagnosis quickly is important because it affects treatment. So, be proactive in your search for a diagnosis.
Writing down your symptoms can help a lot. Note when symptoms happen, how bad they are, and what makes them better or worse. This helps doctors find patterns and make better diagnoses.
Having a list of questions for your doctor is a good idea. Some important questions to ask include:
By working with your healthcare team, being persistent, and staying informed, you can better navigate the diagnostic journey.
Patients often face the challenge of managing symptoms while looking for a diagnosis. This can be tough, but there are ways to make it easier. By using certain strategies, you can feel better and live a better life.
Living an anti-inflammatory lifestyle can help a lot. You can start by changing what you eat. Eating more omega-3 fatty acids from fish and nuts is good. Try to eat less processed foods and sugars.
There are also other ways to feel better. These include:
|
Therapy Type |
Benefits |
|---|---|
|
Acupuncture |
Reduces pain and stress |
|
Meditation/Mindfulness |
Improves mental health and resilience |
|
Physical Therapy |
Maintains mobility and strength |
It’s important to know when to go to the emergency room. If you have chest pain, severe difficulty breathing, or sudden severe headache, get help right away.
Having a support network is key. Family, friends, and support groups can offer emotional support and practical help. Sharing your experiences with others who get it can be very helpful.
Autoimmune diseases are a big challenge to diagnose and manage. Even with normal blood tests, people can have an autoimmune condition. Finding out if you have an autoimmune disease needs a detailed approach.
This includes checking your symptoms, doing lab tests, and trying other ways to diagnose. Knowing about your condition and its symptoms is key. Doctors and patients must work together to find the cause of symptoms and make a good plan.
By taking a complete approach to diagnosis and treatment, people with autoimmune diseases can get better care. This can make their life much better. Finding out you have an autoimmune disease can be hard, but with the right help, you can get through it.
Managing autoimmune diseases well means using medicine, changing your lifestyle, and trying other treatments. Understanding autoimmune diseases helps you take charge of your health. This can make you feel better overall.
Autoimmune diseases happen when the body’s immune system attacks itself. Doctors use a mix of medical history, physical checks, and lab tests to diagnose them. These tests look for specific antibodies and markers of inflammation in the blood.
Yes, it’s possible to have an autoimmune disease even if blood tests seem normal. This is called being seronegative. It means the blood tests don’t find the usual autoantibodies linked to the disease.
Doctors often use tests like the Complete Blood Count (CBC) and the Inflammatory Markers CRP and ESR. They also check for autoantibodies with tests like ANA, RF, and anti-CCP.
Tests might show normal results if the disease is just starting. Or if the antibody levels change a lot. It could also be because of the test’s limitations or the timing of the test.
Symptoms can include pain in joints and muscles, feeling very tired, fever, and feeling generally unwell. Each disease has its own specific symptoms, which can change over time.
Yes, some conditions like seronegative rheumatoid arthritis and early systemic lupus erythematosus can show normal blood tests. So can Hashimoto’s thyroiditis and some spondyloarthropathies.
Doctors might use clinical evaluation, patient history, and imaging like X-rays and MRI. They might also do tissue biopsies and functional medicine tests.
Risk factors include genetics, environmental factors, hormones, and lifestyle and stress. These can all play a role in developing an autoimmune disease.
To manage symptoms, try an anti-inflammatory lifestyle. Consider alternative therapies and know when to seek urgent care. Building a support network is also important.
If you have symptoms but normal blood work, keep pushing for a diagnosis. Document your symptoms well and ask your doctor questions. This can help guide the diagnostic process.
To find the right specialist, research doctors with experience in autoimmune diseases. Ask for referrals from your primary care doctor or other patients. Look at their approach to diagnosis and treatment.
Living with symptoms without a diagnosis can be tough. It includes dealing with uncertainty and the challenges of an invisible illness. Seeking support from healthcare providers, support groups, and loved ones is key.
National Health Service (NHS). Evidence-Based Medical Guidance. Retrieved from https://www.nhs.uk/conditions/autoimmune-diseases/
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!