
Leukocytoclastic vasculitis (LCV) is a big problem in dermatology, affecting thousands every year. It’s a condition where small blood vessels get inflamed. This happens due to infections, medicines, or autoimmune diseases.
At Liv Hospital, we know how important it is to spot LCV early and check it thoroughly. We aim to give top-notch care that meets each patient’s needs.
Understanding LCV is key to treating it well. We’ll look into what causes it, its signs, how to diagnose it, and treatment choices. This will give you a full picture of this complex issue.
Understanding leukocytoclastic vasculitis (LCV) is key to its diagnosis and treatment. It’s a type of small vessel vasculitis. It’s mainly known for the fragmentation of neutrophils around affected vessels.
LCV affects small blood vessels like capillaries and arterioles. It’s marked by inflammation and damage to the vessel walls. The type of LCV depends on the size of the vessels, the extent of the disease, and its causes.
There are two main types of LCV: cutaneous and systemic. Cutaneous LCV only affects the skin. Systemic LCV, on the other hand, affects multiple organs and can be linked to infections, autoimmune diseases, or cancer.
|
Classification Criteria |
Description |
|---|---|
|
Vessel Size |
Primarily affects small vessels (capillaries, venules, arterioles) |
|
Clinical Presentation |
Cutaneous (limited to skin) or Systemic (involving multiple organs) |
|
Underlying Causes |
Infections, Autoimmune Disorders, Malignancies, Idiopathic |
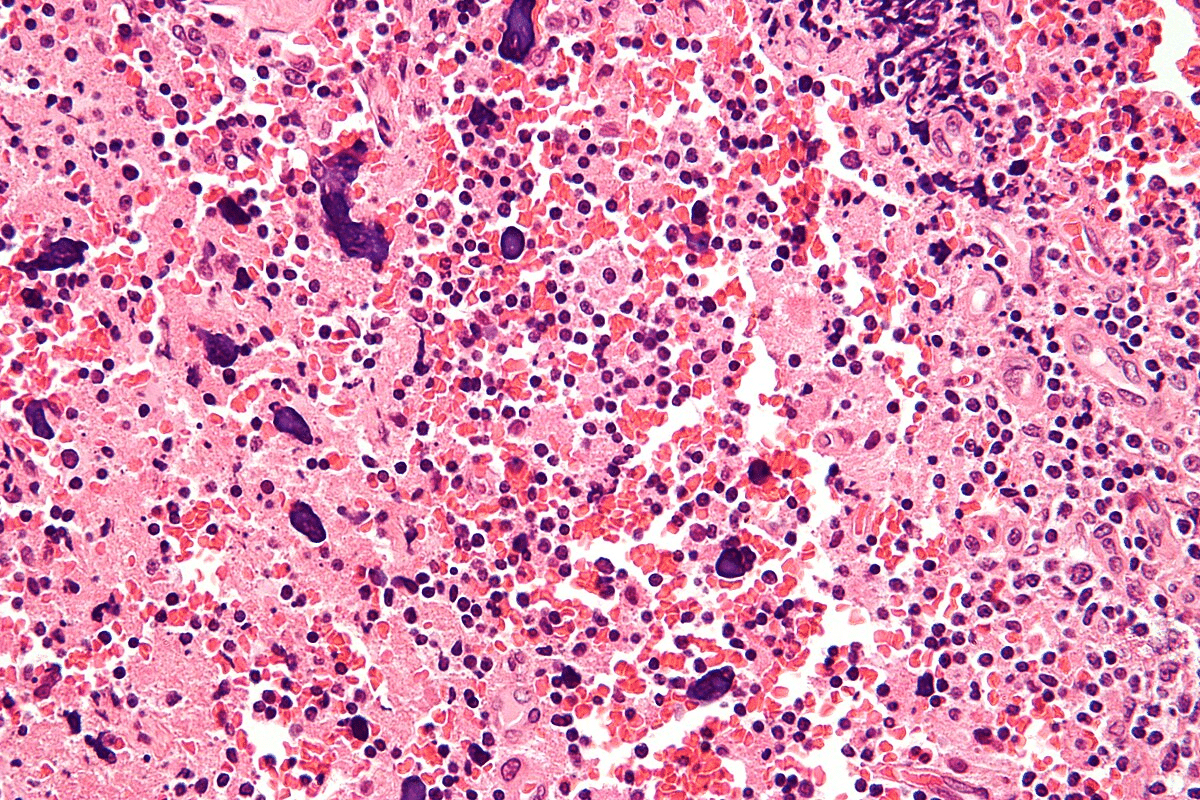
The main signs of LCV include inflammation and damage to the vessel walls. You’ll also see neutrophil fragmentation, red blood cell leakage, and sometimes, immune complexes.
Diagnosing LCV requires a detailed look at skin biopsies or affected tissues. This helps identify the specific vascular changes.
Here’s a quick summary of the key histopathologic features:
|
Histopathologic Feature |
Description |
|---|---|
|
Neutrophilic Inflammation |
Infiltration of neutrophils around and within the vessel walls |
|
Fibrinoid Necrosis |
Necrosis of the vessel wall with fibrin deposition |
|
Leukocytoclasis |
Fragmentation of neutrophils around the affected vessels |
|
Extravasation of Red Blood Cells |
Presence of red blood cells outside the vessels due to vascular damage |

The study of leukocytoclastic vasculitis looks at how common it is and who it affects. This helps us understand what increases the risk of getting it.
Leukocytoclastic vasculitis (LCV) is rare. But, we don’t know exactly how common it is. Research shows it can happen to anyone, but most often between 30 and 60 years old.
It seems to affect both men and women, but women might get it a bit more often. About 3-9 people per million get LCV each year. This number can change based on who is studied and how it’s diagnosed.
LCV can happen to people from all walks of life. Yet, some patterns have been noticed:
Several things can increase the risk of getting LCV:
Knowing these risk factors is key to spotting LCV early. This way, doctors can keep a closer eye on people at higher risk.
Leukocytoclastic vasculitis (LCV) is a complex condition. It involves immune complex deposition, complement activation, and vascular damage. Understanding these steps helps us grasp how LCV develops and grows.
Immune complex deposition is a key step in LCV. It happens when antibodies bind to antigens. In LCV, these complexes are found in small blood vessel walls. This triggers an inflammatory response, a main feature of the disease.
“The deposition of immune complexes in vessel walls is a key event in the development of LCV,” it starts a chain of reactions. These reactions cause inflammation and damage to the vessels.
The complement system boosts the immune system’s ability to fight off microbes and damaged cells. In LCV, immune complexes activate the complement system. This activation leads to the production of various complement components that fuel the inflammation.
Complement system activation creates C3a and C5a, strong mediators of inflammation. These attract neutrophils, making the damage worse.
Neutrophils are key in the inflammatory response. In LCV, they are drawn to immune complex sites by C5a. Activated neutrophils release enzymes and reactive oxygen species, causing blood vessel wall damage.
The damage from neutrophils shows in LCV’s typical signs, like leukocytoclasis and fibrinoid necrosis. This damage can cause symptoms like purpura, ulcers, and skin lesions.
Leukocytoclastic vasculitis (LCV) is a condition where blood vessels get inflamed. It has many causes, both known and unknown. Knowing what causes LCV is key to treating it well.
About 50% of LCV cases have no known cause. These cases are called idiopathic. Even with deep research, no cause is found. Scientists are working hard to understand these cases better.
The other cases have known causes. These include infections, some medicines, and autoimmune diseases. Knowing these causes helps manage the condition better.
The known triggers fall into a few main areas:
|
Trigger Category |
Examples |
|---|---|
|
Infections |
Bacterial infections, Viral hepatitis |
|
Medications |
Antibiotics (e.g., penicillin), NSAIDs (e.g., ibuprofen) |
|
Autoimmune Disorders |
Rheumatoid Arthritis, Systemic Lupus Erythematosus |
Finding out what causes LCV in a patient is very important. It helps doctors decide the best treatment. This might include fixing the cause, managing symptoms, and preventing more problems.
Leukocytoclastic vasculitis can happen when certain medicines are used. This includes antibiotics and NSAIDs. It’s a big worry because it can make treating other health issues harder. We’ll look into how different medicines can cause LCV.
Antibiotics are often linked to LCV. Beta-lactam antibiotics, like penicillins and cephalosporins, are common culprits. It’s thought that these drugs can spark an immune reaction, causing vasculitis.
“The use of antibiotics should be carefully monitored, as LCV can be a rare but serious side effect,” notes a study on drug-induced vasculitis.
NSAIDs, used for pain and inflammation, can also cause LCV. Ibuprofen and naproxen are NSAIDs that have been linked to LCV. This is a concern for people who might be more at risk.
Immunosuppressive drugs, used to treat autoimmune diseases and prevent transplant rejection, can also cause LCV. Azathioprine and cyclophosphamide are examples. This shows how complex the relationship between the immune system and drugs can be.
“The occurrence of LCV in patients on immunosuppressive agents highlights the need for careful monitoring. It shows the importance of weighing the benefits against the risks.”
In summary, medication-induced LCV is a complex issue. It requires careful thought about the medicines used in treatment. By understanding the causes and mechanisms, doctors can better manage and prevent this condition.
It’s important to know how infections can lead to leukocytoclastic vasculitis. This condition can be caused by bacterial or viral infections. Finding out what infection is causing it is key to treating it.
Bacteria like Staphylococcus aureus and Streptococcus can cause LCV. These bacteria start an immune reaction. This reaction leads to immune complexes that damage blood vessel walls.
A study showed a link between Staphylococcus aureus infections and LCV. It’s vital to treat the bacterial infection to manage LCV.
Viral infections, like hepatitis B and C, HIV, and parvovirus B19, can also cause LCV. These viruses trigger an immune response. This response leads to inflammation in blood vessels.
Hepatitis C virus (HCV) is linked to LCV. Studies show HCV patients are more likely to get LCV. This makes it important to check for viral hepatitis when diagnosing LCV.
Other infectious agents can also trigger LCV. For example, some parasitic infections are associated with it. Knowing all possible triggers is important for treating patients well.
Managing LCV depends on treating the underlying cause. A detailed diagnostic test is needed to find the infection. Understanding infections’ role in LCV helps doctors treat it more effectively.
Autoimmune disorders are closely linked with Leukocytoclastic Vasculitis (LCV). This condition causes inflammation in blood vessels. LCV mainly affects small blood vessels and is often seen in autoimmune diseases.
ANCA-associated vasculitides are autoimmune disorders that can cause LCV. These include diseases like Granulomatosis with Polyangiitis (GPA) and Microscopic Polyangiitis (MPA). They are known for causing inflammation that can damage organs like the skin, kidneys, and lungs.
We will explore ANCA-associated vasculitides and their role in LCV. We will also discuss why early diagnosis and treatment are key.
IgA vasculitis, also known as Henoch-Schönlein Purpura (HSP), is linked to LCV. It is caused by IgA immune complexes in blood vessels, leading to inflammation and purpura. This condition is more common in children but can also affect adults.
Rheumatoid Arthritis (RA) and Systemic Lupus Erythematosus (SLE) can also be associated with LCV. RA mainly affects the joints, while SLE can affect many organs. Both can cause vasculitis, including LCV, as part of their disease spectrum.
The table below summarizes the key features of these autoimmune disorders and their association with LCV:
|
Autoimmune Disorder |
Characteristics |
Association with LCV |
|---|---|---|
|
ANCA-Associated Vasculitides |
Presence of ANCA, affects small to medium-sized vessels |
Strong association, can cause LCV |
|
IgA Vasculitis (HSP) |
IgA immune complex deposition, purpura, and inflammation |
Directly associated with LCV |
|
Rheumatoid Arthritis |
Chronic inflammatory joint disease |
Can cause vasculitis, including LCV |
|
Systemic Lupus Erythematosus |
Systemic autoimmune disease affecting multiple organs |
Can cause vasculitis, including LCV |
Cryoglobulinemic vasculitis is another condition linked to LCV. It is caused by cryoglobulins in the blood. These proteins can cause inflammation and damage to blood vessels when they precipitate in cold temperatures. This condition can be linked to infections, autoimmune diseases, and lymphoproliferative disorders.
Understanding the various autoimmune disorders associated with LCV is key for proper diagnosis and treatment. We have discussed several conditions, including ANCA-associated vasculitides, IgA vasculitis, rheumatoid arthritis, SLE, and cryoglobulinemic vasculitis. We highlighted their characteristics and links to LCV.
Understanding LCV’s clinical presentation is key to diagnosing and managing it well. The symptoms of LCV can vary, affecting the skin and other organs.
The skin signs of LCV are often the most noticeable. These can include:
These skin signs come from inflammation of blood vessels, causing damage and purpura.
Patients with LCV may also have systemic symptoms. These include:
The presence and severity of these symptoms can vary widely among patients.
LCV can lead to several complications if not treated promptly. These include:
|
Complication |
Description |
|---|---|
|
Skin Ulceration |
Necrotic lesions can lead to skin ulcers, which may become infected. |
|
Renal Failure |
Severe renal involvement can result in acute or chronic kidney failure. |
|
Gastrointestinal Bleeding |
Vasculitis affecting the gastrointestinal tract can cause significant bleeding. |
Early recognition and management of LCV are critical to prevent these complications.
“The clinical presentation of LCV can be quite varied, making it essential for clinicians to be aware of its diverse manifestations to ensure timely diagnosis and treatment.”
To diagnose Leukocytoclastic Vasculitis, doctors use a detailed method. This includes checking the patient’s health, running tests, and looking at skin samples. This thorough approach helps find LCV and figure out why it happens.
The first step is a detailed check-up. Doctors look at the patient’s past health, find possible causes, and check the skin for signs of LCV.
They look for signs like palpable purpura, which are key signs of LCV. The size and where the skin lesions are can tell a lot about the diagnosis and if it’s affecting the whole body.
Lab tests are very important in diagnosing LCV. They help rule out other conditions and find possible causes. Common tests include:
|
Laboratory Test |
Purpose |
|---|---|
|
CBC |
Check for signs of infection or inflammation |
|
ESR/CRP |
See how much inflammation there is |
|
Urinalysis |
Check the kidneys |
A skin biopsy is a key tool for diagnosing LCV. It shows signs of the condition like leukocytoclasis and inflammation. This helps confirm the diagnosis and gives clues about the cause.
The biopsy findings help doctors understand how severe LCV is and what might have caused it.
After confirming LCV, doctors work to find the cause. They look at the patient’s history, medicines, and possible infections. Knowing the cause helps in treating the condition.
Understanding the cause is key to managing LCV effectively.
Managing leukocytoclastic vasculitis needs a detailed plan. This plan includes fixing the root cause, easing symptoms, and using the right medicine. Each patient’s treatment is unique, based on their condition and what’s causing their vasculitis.
The first step is to find and fix any causes or triggers. This might mean stopping certain medicines, treating infections, or managing autoimmune diseases.
Managing symptoms is key to helping patients with LCV live better. This includes caring for skin wounds, managing pain, and preventing infections.
Medicine is often needed to fight inflammation and the immune system’s overreaction in LCV. The right medicine depends on how severe the disease is and any other health issues.
Here’s a table showing common medicines for LCV:
|
Medication Class |
Examples |
Use in LCV |
|---|---|---|
|
Corticosteroids |
Prednisone |
First-line treatment for reducing inflammation |
|
Immunosuppressants |
Azathioprine, Cyclophosphamide |
Used in severe cases or when corticosteroids are ineffective |
|
Biologic Agents |
Rituximab |
Reserved for refractory cases or specific underlying causes |
To know if Leukocytoclastic Vasculitis can be cured, we need to look at several important factors. The outcome for LCV patients varies a lot. It depends on many things.
The chance of recovery from LCV depends on several things. These include the cause, how much of the body is affected, and the patient’s health. Finding the cause is key because it affects treatment and results.
These factors help doctors predict if a patient will get better and if they might get sick again. This helps doctors create a treatment plan that fits each patient.
LCV can happen in different ways. Some people might only have one episode and then get better. Others might keep getting sick over and over. Knowing these patterns helps doctors manage patient hopes and make treatment plans.
Some things make it more likely for someone to get sick again. These include:
Managing LCV for a long time needs a few steps. These include:
Teaching patients is very important. They need to know the signs of getting sick again and why they must follow their treatment plan.
To stop LCV from coming back, we need to find and manage the things that trigger it. This might mean:
By being proactive, doctors can lower the chance of LCV coming back. This helps patients do better.
In short, while curing LCV is not always possible, understanding the prognosis, patterns of getting better or worse, and long-term care helps doctors give better care. This improves how patients do.
Leukocytoclastic vasculitis (LCV) is a complex condition. It causes inflammation in blood vessels. This leads to symptoms like skin issues and more.
We’ve looked at what LCV is, how common it is, and why it happens. We’ve also talked about its symptoms and how it’s diagnosed.
Knowing what causes LCV is key to treating it. We’ve covered how things like medications and infections can trigger it. A good diagnosis involves several steps, like tests and biopsies.
Treating LCV means fixing the cause and managing symptoms. We’ve discussed how to create a treatment plan that works. LCV needs a detailed approach to manage well.
In short, LCV is a complex condition that needs a deep understanding. We hope this summary helps. It’s all about improving patient care.
Leukocytoclastic vasculitis is a condition that affects small blood vessels. It causes inflammation and damage to the vessel walls. This often leads to skin lesions and can affect other organs too.
LCV can be caused by infections, medications, autoimmune disorders, and sometimes there’s no known cause.
The chance of curing LCV depends on its cause and how severe it is. In some cases, it can get better on its own or with treatment.
Symptoms include skin issues like purpura, erythema, and ulcers. Systemic symptoms like fever, joint pain, and muscle aches can also occur, depending on the organs affected.
Doctors use clinical evaluation, lab tests, and skin biopsies to diagnose LCV. They also look for underlying causes or triggers.
Some medications, like antibiotics, NSAIDs, and immunosuppressants, can cause LCV in certain people.
Infections, including bacterial and viral ones, can trigger LCV. This happens when the body’s immune response leads to vasculitis.
Yes, autoimmune conditions like ANCA-associated vasculitides, IgA vasculitis, rheumatoid arthritis, and SLE can lead to LCV.
Treatment includes addressing the cause, managing symptoms, and using medications like corticosteroids and immunosuppressants. These help control inflammation and prevent damage.
The prognosis depends on the cause, how much of the body is affected, and how well the treatment works. Some may go into remission, while others may have ongoing or recurring disease.
To prevent recurrence, avoid known triggers, manage underlying conditions, and use long-term medications in some cases.
Knowing about LCV is key for early diagnosis and treatment. It helps manage symptoms and prevent complications, improving patient outcomes.
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://pubmed.ncbi.nlm.nih.gov/16249905/
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!