Last Updated on October 31, 2025 by
The most common surgery for fixing the bladder is called cystocele repair or anterior vaginal repair surgery. It’s done to fix a problem where the bladder bulges into the vagina. This can cause pain and other issues.

To find out if you need this surgery, doctors will do a pelvic exam and look at your medical history. They will also do tests on your bladder and urine. Knowing your options is important if you’re looking to feel better. What is the common name for bladder repair surgery? Learn about the bladder sling and other procedures for prolapse.
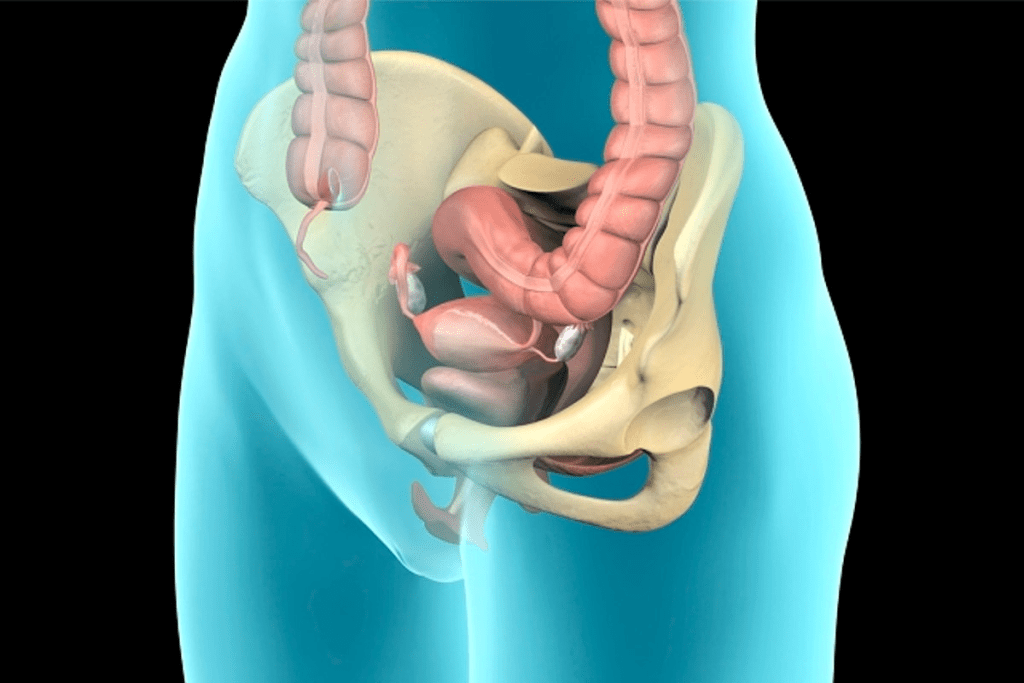
Bladder prolapse happens when the tissues between the bladder and vagina weaken. This causes the bladder to sag into the vagina. It can make life uncomfortable and affect a woman’s quality of life.
Several things can cause bladder prolapse. These include:
These factors can put strain on the pelvic floor muscles and tissues. This can lead to prolapse.
While some cases of bladder prolapse might not need surgery, severe cases can be very uncomfortable. Symptoms that might mean you need surgery include:
If these symptoms are severe and affect your daily life, prolapse of the bladder surgery might be considered.
Before surgery, there are non-surgical options to try. These include:
For elderly women, treatment for incontinence might include a mix of these options. They are tailored to their needs.
It’s important to talk to a healthcare provider. They can help decide the best treatment based on your symptoms and health.
Cystocele repair is a key surgery for bladder issues. It’s aimed at fixing bladder prolapse, where the bladder bulges into the vagina. This can cause discomfort and other problems.
Anterior vaginal repair, or anterior colporrhaphy, is a common method for cystocele repair. It fixes the vaginal wall in front of the bladder. This helps support the bladder and put it back in its right place.
This surgery has a success rate of 70% to 90%. It shows it’s effective in treating bladder prolapse. But success can vary based on each patient’s situation.
The cystocele repair surgery has several steps:
The surgery is usually done under general or regional anesthesia to reduce pain. The choice of anesthesia depends on the patient’s health and the surgeon’s choice.
Cystocele repair is for women with severe bladder prolapse symptoms. These include pelvic pressure, urinary incontinence, or trouble emptying the bladder. It’s for those whose symptoms greatly affect their life and haven’t improved with other treatments.
We look at several things when deciding if someone is a good candidate. These include how bad the prolapse is, the patient’s overall health, and any past surgeries. A detailed check is key to finding the best treatment.
“Cystocele repair is a highly effective treatment for bladder prolapse, giving women a lot of relief.”
Urethral sling procedures are becoming more popular for treating stress urinary incontinence. A bladder sling helps keep the urethra stable, stopping urine leaks. We’ll look at the different materials and methods used in these surgeries.
Bladder slings can be made from various materials, each with its own benefits and risks. Synthetic materials like polypropylene mesh are strong and durable. But some complications have led to looking for other options.
Biological materials like autografts, allografts, and xenografts are also used. These materials might lower the risk of some complications seen with synthetic meshes.
Mid-urethral sling techniques place a sling under the mid-urethra for support. This method is effective for stress urinary incontinence. The retropubic and transobturator routes are two main ways to insert the sling, each with its own benefits.
Bladder slings support the urethra, preventing urine leaks. This helps improve life quality for those with stress urinary incontinence. Studies show bladder slings are effective in treating incontinence.
We see bladder sling procedures as a good option for many. The choice of material and technique depends on the patient’s history and the surgeon’s expertise.
In bladder support surgeries, mesh and native tissue repairs are key options. We’ll look at their benefits and risks to guide your choice.
Synthetic mesh is popular for bladder repairs because it’s strong and works well. The chance of needing another repair is low, about 5.2%. But it’s important to know about possible serious side effects.
Mesh offers long-term support and lowers the chance of prolapse coming back. Yet, it can cause rare but serious problems like mesh erosion, pain, and infection.
Native tissue repair uses your own tissue for bladder support. It has its own pros and cons. One big plus is fewer complications from synthetic materials. But it might have a slightly higher chance of needing another repair.
The results of native tissue repair depend on the method and your health. Methods like anterior vaginal repair are used. They might not last as long as mesh, but they are a good choice for some patients.
The FDA has rules for using synthetic mesh in POP repairs. The FDA warns against mesh in some cases, like transvaginal use, because of risks. It’s key to talk to your doctor about these guidelines and how they apply to you.
It’s wise to talk to your healthcare provider about the best repair for you. They’ll consider your needs and the latest medical advice.
Robotic-assisted and laparoscopic surgeries are changing how bladder repair is done. They offer patients less invasive options. These new methods are becoming more popular in urogynecology, bringing many benefits over traditional surgery.
Robotic-assisted bladder repair surgeries use a robotic system to help surgeons. This allows for more precise and delicate work. High success rates exceeding 95% have been seen, making it a top choice for patients.
The robotic system gives a three-dimensional view of the area being worked on. This helps surgeons do complex repairs more easily and accurately. It also means less damage to tissue and faster healing.
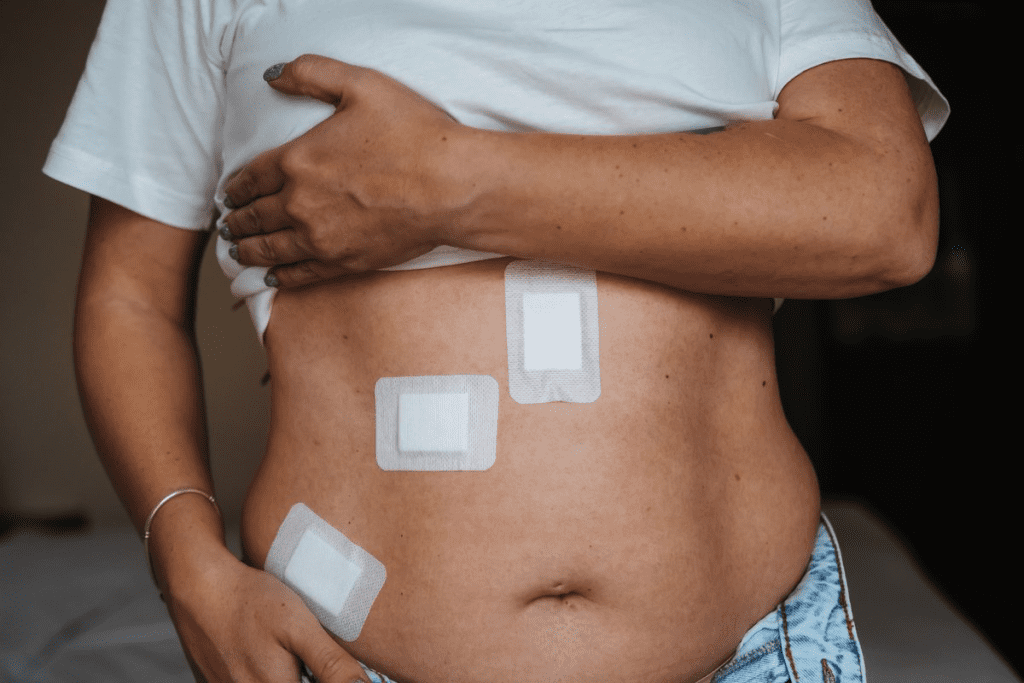
Laparoscopic bladder repair involves small incisions for a laparoscope and tools. This method is less invasive, lowering the risk of complications and speeding up recovery.
Laparoscopic techniques are great for those at risk of open surgery complications or who want less visible scars. The small cuts mean less pain after surgery and a lower chance of infection.
Both robotic-assisted and laparoscopic surgeries have significant recovery benefits over open surgery. Patients usually have shorter hospital stays and less pain after surgery. This lets them get back to their daily lives sooner.
These methods also lower the risk of problems like infection and adhesions. So, patients can expect a smoother and more comfortable healing process.
Getting ready for bladder repair surgery is key to a smooth process. We know surgery can be scary, but being prepared helps a lot. It makes the whole experience better.
Before surgery, we do many tests to check your health and bladder. You’ll have a pelvic exam to see how bad the prolapse is. We also look at your medical history and do bladder and urine tests to check function and for infections.
These tests help us plan the surgery just for you. Our team will explain everything and answer your questions.
Some medicines can affect surgery or recovery. So, we review your meds with you. We might change or stop some to lower risks. This includes blood thinners and medicines that could react with anesthesia.
We’ll tell you exactly what to do with your meds before surgery. It’s important to follow these steps to stay safe and get the best results.
On surgery day, we want you to be ready and comfortable. You’ll get clear instructions on what to do before surgery, like fasting and personal care.
When you get to the surgical facility, you’ll meet our team. The anesthesiologist and nurses will help you understand what’s happening. We make sure you’re comfortable and have all your questions answered before the surgery starts.
Knowing what to expect and following our advice makes you more confident about your surgery. Our team is here to give you the best care and support every step of the way.
Recovering from bladder surgery can be tough, but knowing what to expect helps. The time it takes to recover depends on the surgery type and your health.
Recovery from bladder prolapse surgery usually takes one to six weeks. You’ll need to avoid heavy lifting and bending during this time.
It’s key to follow your surgeon’s advice on activity levels and follow-up care. Slowly getting back to normal activities with medical guidance can lead to the best results.
Bladder surgery can have risks like severe pain, infection, and heavy bleeding. It’s important to watch for these symptoms and talk to your doctor if you notice anything off.
Common complications may include:
Knowing about these complications and how to handle them can make recovery easier.
Regular check-ups after bladder surgery are key to seeing how well the surgery worked. Success rates depend on the surgery type and individual factors. Most people see big improvements in their symptoms.
Regular follow-up appointments help doctors keep an eye on your healing. This ongoing care is vital for the best results and to make sure the surgery lasts.
Bladder repair surgery includes many procedures, like cystocele repair and bladder sling surgery. Each has its own benefits and risks. Patients need to think carefully about their options.
It’s important to talk to healthcare experts for personalized advice. They can guide you based on your health and needs. Knowing about different surgical methods, like robotic and laparoscopic, helps choose the best treatment.
By using the information we’ve shared and talking to a healthcare provider, patients can make smart choices. This can greatly improve their quality.
A cystocele happens when the wall between the bladder and vagina weakens. This causes the bladder to drop into the vagina. It’s a form of pelvic organ prolapse.
Symptoms that might need surgery include feeling heavy or full in the pelvis. You might also have trouble emptying your bladder or see a bulge in your vagina.
Non-surgical options include pelvic floor exercises and lifestyle changes. You can also use a pessary, a device to support the bladder.
The bladder sling procedure places a supportive sling under the urethra. It helps control incontinence by supporting the urethra and bladder neck.
Mesh repairs use synthetic material, while native tissue repairs use your own tissue. Mesh repairs can lead to complications like mesh erosion. Native tissue repairs might take longer to recover.
These methods offer smaller incisions and less blood loss. They also mean shorter hospital stays and faster recovery times than open surgery.
Preparation includes pre-surgical tests and medication adjustments. You’ll also get instructions for surgery day, like fasting and arranging for care after surgery.
The recovery involves rest and avoiding certain activities. You’ll also have follow-up appointments. Possible complications include infection, bleeding, and urinary retention.
Success rates vary based on the surgery type and individual factors. Many women see big improvements. Long-term follow-ups are key to watch for any new symptoms.
A urethral sling procedure is for urinary incontinence. It supports the urethra. Other surgeries might focus on bladder prolapse or cystocele repair.
The FDA has guidelines and warnings on mesh use in pelvic organ prolapse repairs. They highlight the risks and complications.
Yes, some bladder sling surgeries use these minimally invasive methods. They can offer benefits like less recovery time and less pain after surgery.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!