
Calcium Pyrophosphate Deposition Disease, or CPPD, is a common form of arthritis in older people. It’s a type of inflammatory arthritis what is cppd in medical terms.
CPPD is marked by the buildup of calcium pyrophosphate dihydrate crystals. These crystals form in the joints, like the knees, wrists, and hips.
Learning about CPPD is important. It helps us understand its causes, symptoms, and how to treat it. This is key, as almost half of people over 85 have these crystals.

CPPD, or Calcium Pyrophosphate Deposition Disease, is a joint condition. It happens when calcium pyrophosphate dihydrate crystals build up in joints. This can affect the knees, wrists, and hips, causing various symptoms.
The term CPPD disease means arthritis caused by calcium pyrophosphate dihydrate crystals. These crystals form in the joints and surrounding tissues. The medical term CPPD stands for Calcium Pyrophosphate Deposition.
It’s linked to chondrocalcinosis, which is seen on X-rays as calcification in cartilage. Knowing what CPPD is helps doctors diagnose and treat it better. The crystals can cause different types of arthritis, like pseudogout and chronic CPPD arthropathy.
The name CPPD has changed over time. It used to be called pseudogout because it looked like gout. But now, it’s seen as a unique condition with its own causes and symptoms.
|
Term |
Description |
|---|---|
|
CPPD |
Calcium Pyrophosphate Deposition Disease |
|
Chondrocalcinosis |
Radiographic calcification in hyaline and/or fibrocartilage |
|
Pseudogout |
Acute CPP crystal arthritis |
Our understanding of CPPD has grown a lot. Finding calcium pyrophosphate dihydrate crystals in joints has helped doctors diagnose and treat it. This sets it apart from other types of arthritis.
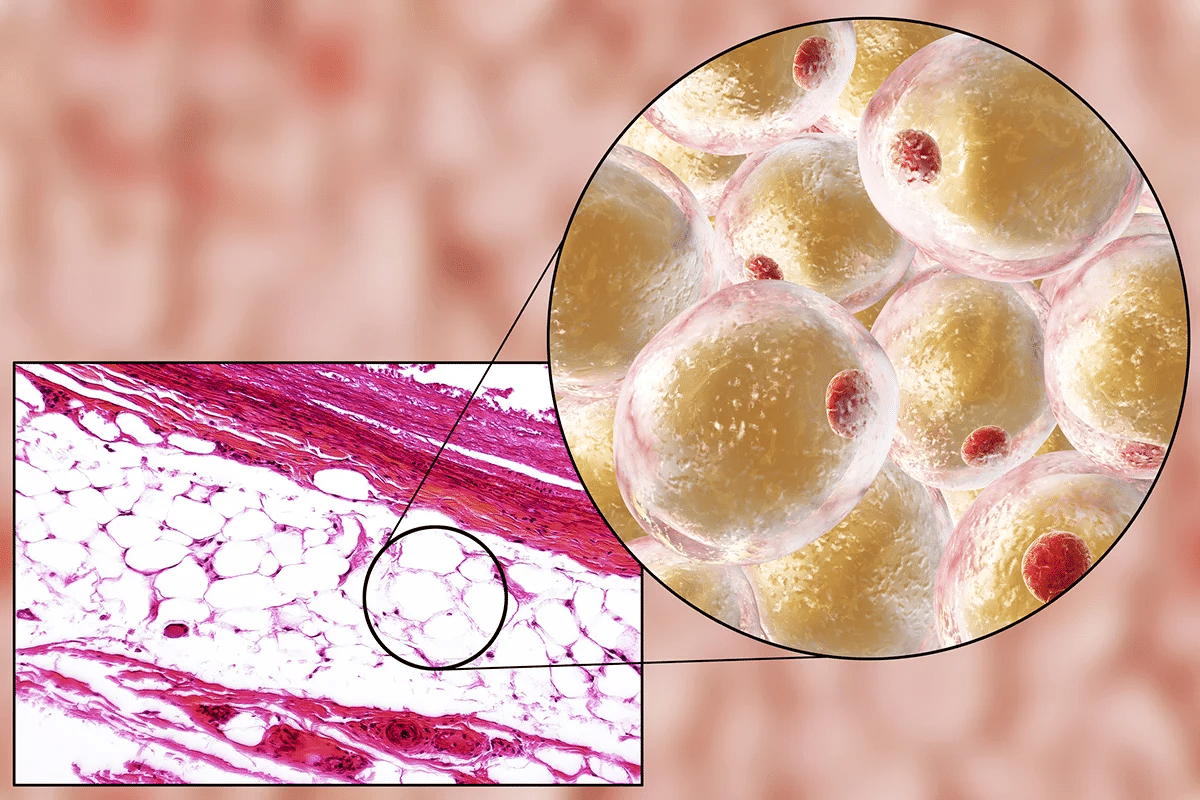
To understand CPPD, we must look at how calcium pyrophosphate dihydrate crystals form in joints. This process is key to the condition, causing crystals to build up and leading to symptoms.
The creation of calcium pyrophosphate dihydrate crystals is vital in CPPD. Increased adenosine triphosphate (ATP) breakdown raises inorganic pyrophosphate (PPi) levels. This is a major factor in crystal formation. Biochemical factors, like enzymes and ion transport, play a role in depositing CPP crystals in joints.
The exact mechanisms behind CPP crystal formation are multifactorial. Both genetics and environment play a part. For example, some metabolic conditions can change the joint’s chemistry, encouraging crystal formation.
CPPD mainly affects the tissues around joints, with the knees, wrists, and hips being most common. The buildup of CPP crystals causes inflammation and degeneration. This leads to the symptoms seen in CPPD.
The knees are most prone to CPPD because of the stress they bear. Other joints, like wrists and hips, can also be affected. This results in a variety of symptoms, from sudden arthritis to long-term joint damage.
It’s important to know about Calcium Pyrophosphate Deposition Disease (CPPD) to manage it well. CPPD happens when calcium pyrophosphate crystals form in joint cartilage. This leads to different symptoms.
CPPD is found in 7.0% to 13.7% of people. Age is the main risk factor. The disease becomes more common after 60.
It affects both men and women equally. This shows there’s no gender preference.
The exact cause of CPPD is not known. But, some genetic and environmental factors are linked to it. Trauma or surgery to a joint can raise the risk. Also, some metabolic disorders are associated with CPPD.
Key risk factors include:
Knowing these risk factors helps in early diagnosis and treatment of CPPD.
CPPD can show up in many ways, from no symptoms at all to sudden arthritis. It’s important to know how it can affect people to treat it right. Each way it shows up needs a different approach to manage it well.
Many people with CPPD don’t feel any pain because of it. This is called asymptomatic chondrocalcinosis. It happens when calcium pyrophosphate crystals build up in the cartilage but don’t cause symptoms. It’s thought that a lot of older adults might have this without knowing it.
Pseudogout is a sudden and severe joint pain and swelling. It happens when calcium pyrophosphate crystals get into the joint and cause inflammation. People with pseudogout often have swollen, warm, and painful joints, usually in the knee or wrist.
“The acute attacks of pseudogout can be quite debilitating, requiring prompt medical attention to alleviate symptoms and prevent long-term joint damage.”
Chronic CPPD arthropathy is a long-lasting and degenerative form of the disease. It causes ongoing joint pain and changes in the joints. This can make it hard to move and may look like osteoarthritis. Managing chronic CPPD arthropathy needs a mix of medicines and other treatments.
In summary, CPPD can affect people in many ways, impacting their daily life. Knowing how it can show up helps doctors give better care.
CPPD doesn’t happen alone; it often comes with other health issues. Knowing about these connections is key to giving patients the best care.
Many metabolic disorders are linked to CPPD. These include:
These disorders can affect how CPPD develops and grows. It’s important to treat them as part of the treatment plan.
Endocrine disorders also play a big role in CPPD. For example:
It’s vital to manage these endocrine conditions to lower CPPD risk and impact.
Hemochromatosis, a condition of too much iron, is another big comorbidity with CPPD. Other connections include:
|
Condition |
Association with CPPD |
|---|---|
|
Hemochromatosis |
Too much iron can lead to CPPD. |
|
Hyperparathyroidism |
Calcium imbalances can affect CPPD. |
|
Hypomagnesemia |
Low magnesium can change crystal formation. |
Knowing about these conditions and comorbidities helps healthcare providers give better treatment for CPPD.
It’s key to tell CPPD apart from other arthritis types for better treatment and care. CPPD is often mistaken for gout, osteoarthritis, and rheumatoid arthritis. This is because their symptoms and signs can look similar.
Gout and CPPD both cause sudden joint pain and swelling. But they have different causes. Gout is due to monosodium urate crystals, while CPPD is caused by calcium pyrophosphate dihydrate crystals. To tell them apart, doctors use synovial fluid analysis.
Osteoarthritis (OA) is a wear-and-tear disease that can happen with CPPD. OA mainly affects the cartilage, while CPPD involves calcium crystals in the joint. Chondrocalcinosis, seen on X-rays, can help tell CPPD from OA. But, CPPD can also show up without chondrocalcinosis.
Rheumatoid arthritis (RA) is an autoimmune disease that causes joint pain and damage. CPPD can look like RA with chronic pain and swelling. But RA has more widespread symptoms and specific blood tests. A detailed check-up and tests are needed to tell CPPD and RA apart.
In summary, knowing how to spot CPPD from other arthritis types is vital. It helps doctors give the right treatment. This way, patients can get better faster.
Getting a correct diagnosis for CPPD is key to managing and treating it well. Doctors use a mix of clinical checks, imaging, and lab tests to spot calcium pyrophosphate dihydrate (CPPD) crystals.
Imaging is a big help in finding CPPD. Here are some ways:
These tools help see how much the joints are affected and where CPPD crystals are.
The best way to confirm CPPD is by finding CPP crystals in synovial fluid. This fluid is taken from the joint and checked under a microscope. It’s the most reliable way to diagnose CPPD, mainly during flare-ups.
Lab tests aren’t the final say but they help rule out other issues and check for metabolic problems. Some tests include:
|
Test |
Purpose |
|---|---|
|
Serum calcium and phosphate levels |
To check for metabolic disorders linked to CPPD. |
|
Complete Blood Count (CBC) |
To see if there’s inflammation or infection. |
|
Erythrocyte Sedimentation Rate (ESR) |
To measure inflammation levels. |
By combining these methods, doctors get a full picture of CPPD. This helps them create a good treatment plan.
There’s no cure for CPPD yet, but many treatments can help manage its symptoms. The main goal is to ease pain, reduce swelling, and improve how joints work. We’ll look at different ways to treat CPPD, like medicines, non-medical methods, and new treatments.
Medicines are key in treating CPPD to lessen pain and swelling. Nonsteroidal anti-inflammatory drugs (NSAIDs) are often used for sudden CPPD attacks. Sometimes, colchicine is given to fight swelling. For severe cases, corticosteroids can be used, either taken by mouth or injected into the joint.
Choosing the right medicine depends on how bad the symptoms are, the patient’s health, and possible side effects. We must think carefully about these factors when picking a treatment plan.
Non-medical ways are also important in managing CPPD. Joint aspiration can help by taking out extra fluid from the joint. Physical therapy is also helpful, keeping joints flexible and strong. It’s also good to stay healthy and avoid putting too much strain on joints.
New research is looking into CPPD, with some promising treatments. Interleukin-1 (IL-1) inhibitors might help reduce swelling in CPPD. Other new treatments, like crystal-dissolving therapies, are being tested too.
As we learn more about CPPD, more treatment options will become available. We’re hopeful that future studies will find better ways to manage this condition.
Living with CPPD can be tough, but making lifestyle changes can help a lot. It’s important to manage CPPD with both medical care and lifestyle changes.
Protecting your joints is key when you have CPPD. Stay away from activities that hurt your joints too much. Use tools and devices that help you move better.
Exercise and physical therapy are very important for CPPD. Gentle exercises help keep your joints moving and less stiff.
“Physical therapy can be instrumental in helping patients with CPPD maintain functional ability and reduce pain.”
— Expert in Rheumatology
|
Exercise Type |
Benefits |
|---|---|
|
Low-impact aerobics |
Improves cardiovascular health without straining joints |
|
Range-of-motion exercises |
Maintains joint flexibility and reduces stiffness |
|
Strengthening exercises |
Supports joint stability and overall muscle strength |
Changing your diet can also help with CPPD. There’s no special “CPPD diet,” but eating healthy and staying hydrated is good.
If you have CPPD, knowing when to see a doctor is important. Look for sudden pain, swelling, fever, or signs of infection.
Key signs that require medical attention:
By making these lifestyle changes and taking care of yourself, you can manage your CPPD symptoms better. This can improve your life a lot.
Knowing what CPPD is in medical terms is key to managing calcium pyrophosphate deposition arthropathy. CPPD is a common issue in older adults. It happens when calcium pyrophosphate dihydrate crystals build up in joints, causing various symptoms.
The term CPPD is often used in medical texts. Learning about its causes, symptoms, and treatments helps people deal with their diagnosis better. This knowledge improves their life quality.
Managing CPPD well requires both medicine and lifestyle changes. Making healthy choices, like protecting joints, exercising, and eating right, is important. These steps help lower the risk of serious problems and boost overall health.
As we’ve seen, understanding CPPD is vital for managing it. Recognizing its signs and symptoms helps people get the right care on time. This leads to a better life for those with CPPD.
CPPD stands for Calcium Pyrophosphate Deposition Disease. It’s a condition where calcium pyrophosphate dihydrate crystals build up in joints. This leads to different symptoms.
Symptoms of CPPD vary. They can range from no symptoms at all to severe joint pain and swelling. Some people may also experience stiffness.
Doctors use X-rays and ultrasound to diagnose CPPD. They also check the fluid in the joints for crystals. Lab tests help rule out other conditions.
Treatments for CPPD include medicines like NSAIDs and colchicine. Non-medical options include joint injections and physical therapy. New treatments aim to reduce crystals and inflammation.
Yes, making lifestyle changes can help manage CPPD. This includes protecting joints, exercising, and following a healthy diet. These steps can improve symptoms and quality of life.
CPPD is linked to metabolic disorders, endocrine conditions, and hemochromatosis. It’s important to treat these conditions to manage CPPD effectively.
CPPD is different from other arthritis types like gout and osteoarthritis. It needs a detailed diagnosis to find the cause of symptoms.
Genetics play a role in CPPD. Knowing the genetic risks helps identify people at high risk. This guides preventive measures.
There’s no cure for CPPD. But, with the right treatment and lifestyle changes, people can live better lives despite the condition.
Seek medical help if you have sudden joint pain or swelling. Or if your symptoms get worse. Getting a proper diagnosis and treatment is key.
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK540151/
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!