Last Updated on October 31, 2025 by
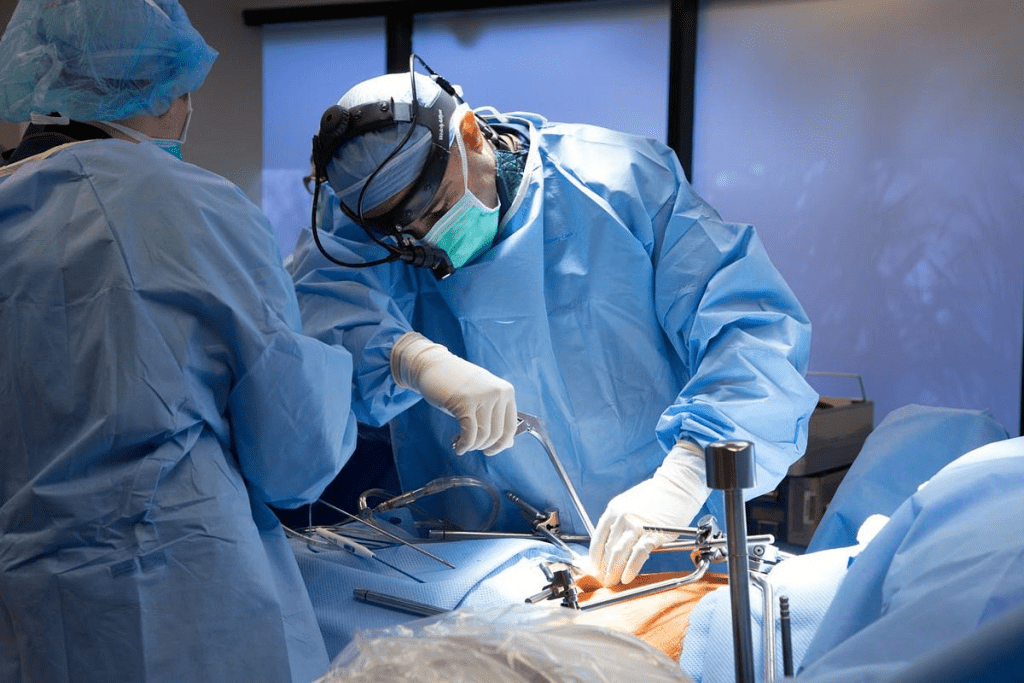
Urethral stricture surgery is a big worry for those facing this issue. At Liv Hospital, we know how vital it is to give full details about the surgery. This includes its results and possible problems.
Urethral stricture happens when scar tissue forms in the urethra. It can affect anyone, but it’s more common in men over 55. Open urethroplasty is seen as the best treatment. It has success rates from 71% to 95%, depending on the method and the patient.
It’s important for patients to understand urethral stricture surgery. A detailed check-up is done before surgery. This helps find out how bad and where the stricture is.
Tests like a retrograde urethrogram or cystoscopy are used to check the stricture. A retrograde urethrogram is an X-ray that shows the urethra’s blockage. Cystoscopy uses a camera to see the stricture directly. These tests are key for planning the surgery.
Your doctor will tell you what to eat or drink before surgery. They will also talk about your medications. It’s important to follow these instructions to stay safe during the surgery.
A narrow urethra, or urethral stricture, happens when scar tissue narrows the urethra. This can cause weak urine flow and trouble starting to urinate. Knowing the cause and extent of the stricture is important for treatment.
Tests confirm the blockage’s length and location. Sometimes, urethral dilation or a sounding rod might be used. But these are not always the final solution.
Liv Hospital’s team prepares patients for surgery by guiding them through what to expect. We emphasize the pre-surgical evaluation, customizing each treatment plan to suit individual needs.
There are several ways to fix urethral stricture, each with its own benefits. The right choice depends on the stricture’s location, length, and the patient’s health.
Open urethroplasty is the top choice for fixing urethral stricture. It removes the narrowed part and rebuilds it. Our skilled surgeons at Liv Hospital use advanced techniques for quick recovery and best results. Training in urethral reconstruction boosts the success rate of this surgery.
“Urethroplasty has changed how we treat urethral stricture, giving patients a lasting fix,” says a top urologist. Many studies back up the success of open urethroplasty.
Endoscopic urethrotomy is a less invasive option. It uses an endoscope to widen the stricture. But, it’s best for short strictures. Our surgeons decide if this method is right for each patient.
Urethral dilation stretches the narrowed area with dilators. It’s done under local anesthesia and works for simple strictures. But, it might need to be done again because the stricture can come back. At Liv Hospital, we customize treatment plans, considering the pros and cons of dilation.
Choosing less invasive treatments for stricture disease depends on many factors. Specialized training in urethral reconstruction helps decide between endoscopic treatments and urethroplasty.
Urethral stricture surgery has shown varying degrees of success. Long-term success rates range from 71% to 95%. Our personnel aims for the highest success rates at Liv Hospital. We use the most effective and up-to-date surgical methods.
The success rates of urethral stricture surgery are encouraging. Long-term success rates range between 71% and 95%. The type of surgery used greatly affects these outcomes.
Studies show that success rates can be influenced by several factors. These include the stricture’s length and location, and the patient’s health. For example, more endoscopic treatments are needed for longer strictures.
Several factors can impact the success of urethral stricture surgery. These include the length and location of the stricture, the surgical technique used, and patient-specific characteristics like age and health.
Hence, Liv Hospital’s team of experts discusses these factors with you in detail. We ensure you understand what to expect from your surgery and the possible outcomes.
It’s important to talk about the early problems that can happen after urethral stricture surgery. Liv Hospital works hard to manage these risks. This way, we can give our patients the best care possible.
Wound pain is a common issue after this surgery. Effective pain management is key for comfort and healing. We offer pain medication as part of our care after surgery.
Infection is a big risk, affecting about 32% of patients. We use antibiotics to lower this risk. Keeping an eye out for infection signs is a big part of our care.
Edema and swelling can also happen early on. We watch for these and use medicine if needed. Proper post-operative care is key in reducing these risks.
When patients go home, they get a urinary catheter, pain meds, antibiotics, and maybe something for bladder spasms. Our team makes sure patients know how to handle these things. This helps them recover smoothly.
Knowing about these early complications and how we manage them helps patients through their recovery. Liv Hospital’s team is dedicated to top-notch care and supports every step of the way.
Urethral stricture surgery can lead to long-term issues. At Liv Hospital, we focus on these complications to give the best care.
Urinary spraying or weak streams are common problems. They happen when the urethra can’t keep a steady flow. This is often due to scars or incomplete healing. About 23% of patients face this issue later on.
Studies show that each internal urethrotomy raises the risk of needing more surgery by 19%. We talk about these complications and how to manage them.
Fistulas are another serious issue. They are abnormal connections between the urethra and the skin or other organs. This can cause pain and infections. A study on NCBI stresses the importance of careful planning and follow-up to avoid this.
Erectile dysfunction can greatly affect a patient’s life. It’s caused by physical and mental factors. Many studies show it’s a common problem after surgery.
We aim to help patients understand these risks. Liv Hospital’s workforce is equipped to offer top-notch care to reduce these risks and improve outcomes.
After urethral stricture surgery, recovery is key. At our institution, we focus on post-operative care. This ensures our patients heal well and get back to normal quickly.
Right after surgery, patients go to the recovery room. They need someone to drive them home if it’s an outpatient procedure. We watch for any immediate problems and manage pain to reduce discomfort.
Managing urinary catheters is a big part of care. Patients usually have a catheter to help the urethra heal while they can urinate. Our team teaches patients how to care for their catheters to avoid infections and ensure healing.
In some cases, male external catheters are used for urinary incontinence during recovery. It’s important to fit and manage these catheters correctly to avoid skin problems and keep patients comfortable. Our healthcare team teaches patients how to use and care for these catheters.
Long-term follow-ups are vital to track healing and catch any issues early. Patients usually need to see their healthcare provider regularly to check on healing and remove catheters or stents when needed.
At these visits, we check for stricture recurrence and answer any questions. Our aim is to support patients throughout their recovery, ensuring the best results.
By sticking to the recovery plan and attending all follow-up visits, patients can greatly improve their surgery outcomes.
Urethral stricture treatment isn’t just about surgery. There are other ways to manage it. Surgery is often the best choice, but not everyone can or wants to have it.
At Liv Hospital, we talk about other options with our patients. We look at non-surgical methods and using urinary catheters. These can help patients feel better and live better lives.
There are many non-surgical ways to treat urethral stricture. The American Urological Association says endoscopic methods are good for short strictures.
These methods work well for some patients, mainly those with short or simple strictures.
For quick relief, urinary catheters can be a good choice. They help with urine retention and symptoms of urethral stricture.
It’s important to talk to a doctor to find the best treatment. At Liv Hospital, we help with catheters and other non-surgical options.
Choosing between non-surgical options and surgery depends on several things. These include the stricture’s length and location, the patient’s health, and personal wishes.
We help our patients choose the best treatment. We consider both surgery and non-surgical options.
Urethral stricture surgery can greatly help patients. At Liv Hospital, we’ve seen it improve lives. It can make urinating easier and more normal again.
While there are risks, many see big improvements. We guide patients to choose the best treatment for them. This includes talking about the surgery’s benefits and risks.
In the end, surgery is a good choice for many. With the right care, patients can live better lives. This makes the surgery a valuable option.
Urethral stricture surgery is a procedure to fix a narrow urethra. It’s the top choice for treating this issue.
Doctors use tests like retrograde urethrogram or cystoscopy to find out where and how bad the stricture is.
There are several ways to fix a narrow urethra. These include open urethroplasty, endoscopic urethrotomy, and urethral dilation. Each method has its own benefits and when to use it.
The success rate of surgery varies. It can be between 71% to 95%. This depends on the surgery type and the patient’s health.
Early problems can include pain, infection, and swelling. These are managed with good care after surgery.
Long-term issues might include urine spraying, fistulas, and problems with sex. These can be lessened with careful planning and follow-up care.
Recovery involves careful post-operative care. This includes learning to use urinary catheters and regular check-ups to see how you’re healing.
Yes, there are non-surgical options and using catheters. These might be for those who can’t or don’t want to have surgery.
Urethra sounding uses a rod to widen the urethra. It’s not a cure but can help diagnose or temporarily relieve symptoms.
Urethral dilation is a treatment for urethral stricture. But, it might not work as well as open urethroplasty in all cases.
Looking for “quick fix urine near me” might offer temporary relief. But, it’s key to see a healthcare provider for the right diagnosis and treatment.
Keloid removal cream might help with scars after surgery. But, it’s important to talk to your healthcare provider about using it as part of your care.
The frontal suture isn’t directly linked to urethral stricture surgery. But, knowing about surgical terms can help understand the procedure better.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!