Getting a diagnosis of type1 diabetes for your child can be scary. You might wonder if they will outgrow it. Childhood diabetes, also called juvenile diabetes, is when the pancreas doesn’t make enough insulin.
Managing this condition is tough, but it’s key to know most kids with type 1 diabetes don’t just ‘grow out’ of it. Some kids might go through a phase where they make more insulin and need less. This is called partial or complete remission.
We’ll dive deeper into this topic. We’ll talk about what the condition is, how to manage it, and the chance of remission.
Key Takeaways
- Most children with type1 diabetes need insulin for life.
- Some kids might have a phase where they make more insulin.
- Parents need to understand the condition and its care.
- New treatments and care options are available for diabetes.
- Living with type1 diabetes is a lifelong challenge.
What Childhood Diabetes Actually Means
It’s important to understand childhood diabetes to manage it well. Type1 diabetes happens when the body’s immune system attacks the insulin-making cells in the pancreas. This makes it hard for the body to make insulin.

The Autoimmune Nature of Type1 Diabetes
Type1 diabetes is an autoimmune disease. This means the body’s defence system attacks the insulin-making cells in the pancreas. This attack stops the body from making insulin, a key hormone for glucose control.
Key aspects of this autoimmune response include:
- The body’s immune system mistakenly attacks the pancreas’s beta cells.
- A significant reduction or complete halt in insulin production.
- The necessity for external insulin administration to control blood glucose levels.
How T1D Differs from Type2 Diabetes
Type1 diabetes (T1D) is different from Type 2 diabetes in its causes and treatment. Type 2 diabetes is about insulin resistance and not making enough insulin. T1D is when the body can’t make insulin because of an autoimmune attack on the insulin-making cells.
The main differences are:
- Autoimmune destruction in T1D versus insulin resistance in Type 2.
- Insulin dependency from the start in T1D.
- Typical age of onset, with T1D often showing up in kids and young adults.
Key Signs and Symptoms in Children
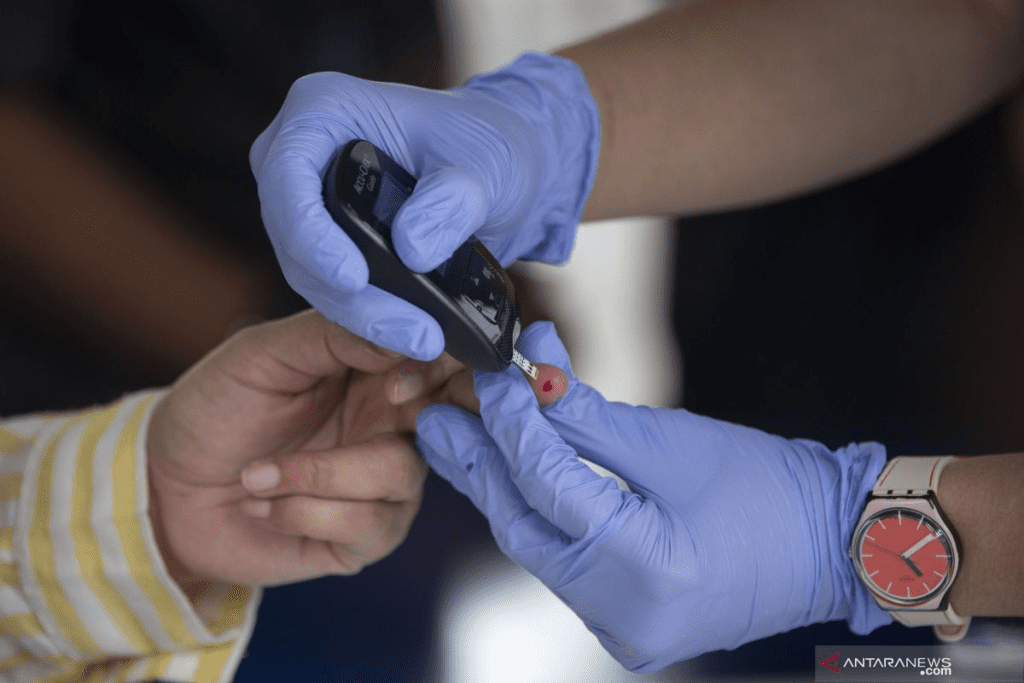
It’s key to spot the signs and symptoms of Type 1 diabetes in kids early. Common signs include:
- Increased thirst and urination.
- Weight loss even when hungry.
- Fatigue and blurry vision.
These symptoms come on fast, often in just a few weeks. They need quick medical help to manage the condition well.
Why Most Children Don’t “Grow Out” of Type 1 Diabetes
Type 1 diabetes in children is permanent because of its autoimmune nature. It destroys the beta cells in the pancreas. This makes the body unable to make insulin, a key hormone for glucose control.
Permanent Nature of Beta Cell Destruction
The destruction of beta cells is a key feature of Type 1 diabetes. This process is irreversible, meaning children need insulin for life to control blood sugar. Studies show that genetics and environment trigger this autoimmune attack.
Knowing what causes Type 1 diabetes helps in finding better ways to manage it. Even though we don’t know all the triggers, we know beta cell destruction is permanent. This means children need to manage their diabetes for their whole lives.
Necessity of Lifelong Insulin Therapy
Children with Type 1 diabetes need insulin because their beta cells are destroyed. Lifelong insulin therapy is needed to replace the insulin the pancreas can’t make. New ways to give insulin and check blood sugar have made managing Type 1 diabetes easier.
Insulin therapy for life shows how important a good diabetes plan is. This plan includes insulin, diet changes, and exercise. It also means checking blood sugar often to stay healthy.
Understanding Diabetes Management vs. Cure
Even though there’s no cure for Type 1 diabetes, managing it well can greatly improve life. Diabetes management includes insulin, diet, and exercise. Research is ongoing to find better ways to manage and maybe even cure Type 1 diabetes.
It’s important to know the difference between managing diabetes and finding a cure. While we can manage it well, finding a cure is what researchers are working towards. They aim to find a way to restore normal glucose regulation.
The “Honeymoon Phase”: When Symptoms Temporarily Improve
About 40% of kids and teens with type 1 diabetes go through a ‘honeymoon phase’ after diagnosis. During this time, their body’s insulin-making cells work a bit better. This means they need less insulin from outside their body. It’s a welcome break for families adjusting to a new diagnosis.
What Happens During Partial Remission
Partial remission, or the ‘honeymoon phase,’ means better blood sugar control and less insulin needed. During this time, the pancreas can make some insulin, making it easier to keep blood sugar in check. But remember, this phase is short-lived and doesn’t mean diabetes is gone for good.
The 40% Rule: Who Experiences Remission
Studies show that about 40% of kids and teens with type 1 diabetes will see some remission. Why some experience remission and others don’t is not fully understood. But age at diagnosis and initial health status might play a part.
Typical Duration: Months to Years
The ‘honeymoon phase’ can last anywhere from a few months to a few years. Keeping a close eye on blood sugar and adjusting insulin is key to keeping it under control and may extend the remission.
Managing Diabetes During the Honeymoon Period
Managing type 1 diabetes during the ‘honeymoon phase’ needs careful watching and flexibility. Insulin doses may change as insulin production varies. Working with a healthcare provider to adjust insulin therapy can help make the most of this time.
5 Key Factors That Influence Diabetes Remission
It’s important to know what affects diabetes remission in kids. Remission in type 1 diabetes is complex. We’ll look at these factors to help manage the condition well.
Age at Diagnosis: Why It Matters
The age a child is diagnosed with type 1 diabetes matters a lot. Younger kids have a better chance of remission because they have more beta-cell function. Early diagnosis and treatment can lead to better results.
Initial Metabolic Status and Blood Glucose Levels
The initial metabolic status and blood glucose levels at diagnosis are key. Kids with less severe metabolic derangement have a better chance of remission. Keeping blood glucose levels in check from the start is vital.
Genetic Background and Predisposition
A child’s genetic background can affect their risk of type 1 diabetes and remission. Knowing genetic factors helps tailor treatment plans.
Early Intervention and Treatment Approaches
The approach to early intervention and treatment is very important. Aggressive and appropriate management of type 1 diabetes can improve remission chances. This includes insulin therapy and lifestyle changes.
Understanding these factors helps healthcare providers and families manage type 1 diabetes better. This improves the quality of life for kids with the condition.
The Reality of Complete Remission in Type1 Diabetes
Type 1 diabetes remission, including complete remission, is rare. It means keeping blood sugar normal without insulin. Only about 5% of people with type 1 diabetes achieve this.
The Rare Cases: Less Than 5% Experience Complete Remission
Complete remission in type 1 diabetes is very rare. Studies show less than 5% of people with it can stop using insulin. This is because the disease is an autoimmune attack on the pancreas’ insulin-making cells.
Key factors contributing to the rarity of complete remission include:
- The extent of beta cell destruction
- The effectiveness of the immune system’s attack
- The individual’s genetic predisposition
- The timing and approach to initial treatment
Why Half of Children Never Experience Any Remission
Many children with type 1 diabetes never see remission. About half of them don’t enter any kind of remission. This is due to several reasons, like age at diagnosis and genetic background.
The Three-Year Threshold: Why Long-Term Remission Is Extremely Rare
Remission, when it happens, usually lasts only a few years. Studies show it mostly occurs within the first three years. Remission lasting longer than this is very rare. This highlights the need for early and effective treatment.
Setting Realistic Expectations for Parents and Children
Knowing how rare complete remission is helps parents and kids set realistic goals. While hope for remission is there, managing diabetes well is key. It’s about living a good life despite the challenges.
We know type 1 diabetes can be tough. But with the right care and lifestyle, people can live full and happy lives.
Conclusion: Living Well with Childhood Diabetes
Type1 diabetes is a lifelong condition, but kids can live active, healthy lives with the right care. New ways to check blood sugar and give insulin have made life better for kids with type1 diabetes.
Managing type1 diabetes is a big job. It needs regular checks, insulin shots, and changes in how you live. Kids with diabetes can do all the things they want to do and reach their goals.
We keep working on new medical tech and ways to treat diabetes. We’re dedicated to giving top-notch care and support to kids with type1 diabetes and their families. With good diabetes care, kids can grow up happy and healthy.
FAQ
What is type1 diabetes, and how does it differ from type2 diabetes?
Type1 diabetes is an autoimmune disease. It happens when the body’s immune system attacks and destroys the insulin-producing beta cells in the pancreas. This results in the body’s inability to produce insulin. It’s different from type2 diabetes, which is caused by insulin resistance and impaired insulin secretion.
What are the common symptoms of type1 diabetes in children?
Symptoms of type1 diabetes in children appear quickly. They include increased thirst and urination, weight loss, and fatigue. It’s important to recognize these signs early to get a timely diagnosis and start treatment.
Will my child “grow out” of type1 diabetes?
Type1 diabetes is a lifelong condition. There is no cure for it. While management strategies can control the condition, the autoimmune destruction of beta cells is permanent. This means a lifelong need for insulin therapy.
What is the “honeymoon phase” in type1 diabetes, and how long does it last?
The ‘honeymoon phase’ or partial remission is when the body’s remaining insulin-producing cells can make some insulin. This reduces the need for exogenous insulin. This phase can last from months to a few years. It’s seen in about 40% of children with type1 diabetes.
What factors influence whether a child with type1 diabetes will experience remission?
Several factors can affect whether a child with type1 diabetes will experience remission. These include the age at diagnosis, initial metabolic status and blood glucose levels, genetic predisposition, and early intervention and treatment approach.
Is complete remission possible in type1 diabetes?
Complete remission, where the body makes normal insulin again without needing insulin therapy, is very rare. It happens in less than 5% of cases.
How can I manage my child’s type 1 diabetes effectively?
Understanding the condition, its management, and what affects remission is key. Tailoring management strategies to the child’s needs is important. Advances in medical technology and treatment strategies improve the quality of life for children with type1 diabetes.
What is the significance of early intervention in type 1 diabetes?
Early intervention and treatment can affect the extent of remission and overall management. Understanding the importance of timely diagnosis and intervention is vital for good glycemic control
Reference
- American Diabetes Association. (2022). 2. Classification and diagnosis of diabetes: Standards of medical care in diabetes”2022. Diabetes Care, 45(Supplement 1), S17“S38. Retrieved from https://diabetesjournals.org/care/article/45/Supplement_1/S17/138927/2-Classification-and-Diagnosis-of-Diabetes-Standards










