
Did you know that surgical mortality statistics show big differences in results? The variations in surgical mortality statistics are influenced by the type of surgery, the health of the patient, and the experience of the surgical team. We dive into the complex world of surgical outcomes, looking at the latest research and stats.surgery survival ratesBowel Obstruction Surgery Survival Rates Explained
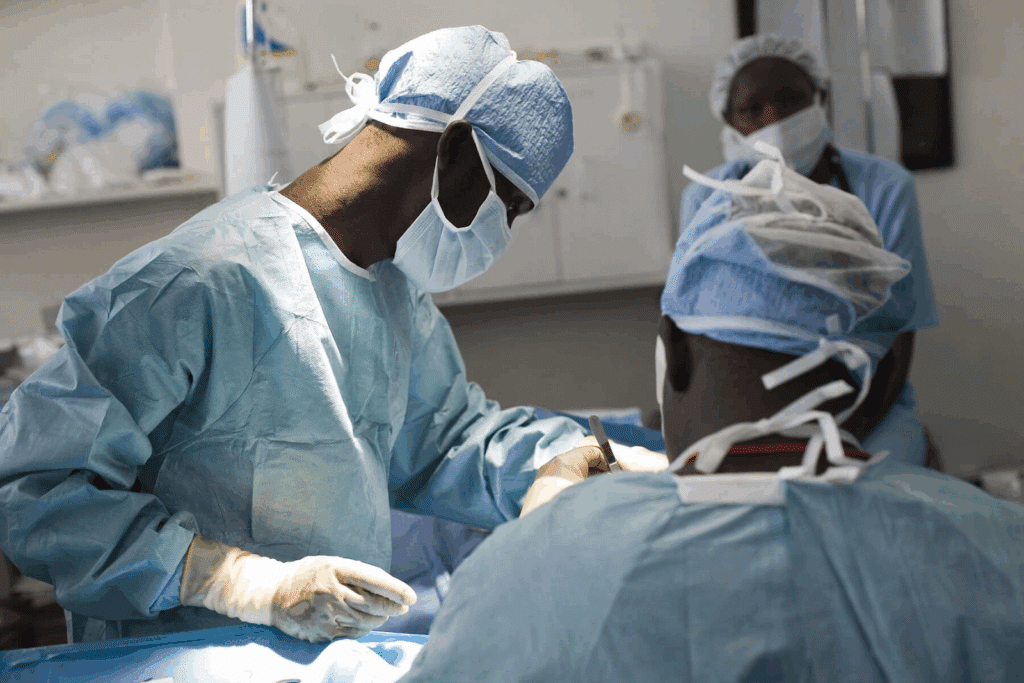
Recent studies highlight how surgery success rates can be affected by many things. This includes the skill of the surgical team and the quality of care after surgery. As we explore surgery survival rates, we aim to give a full picture of what affects patient results.
It’s key for doctors and patients to grasp surgery survival rates. These rates show how well surgeries work and the risks involved. By looking at these rates, we can learn what affects patient results and make smarter choices.
When we talk about surgery survival rates, we mean how many patients live after a surgery. These numbers come from surgical outcome statistics. They help us see the risks and possible results of surgeries.
Survival rate data comes from hospitals and national records. For example, studies show survival rates are key in making medical decisions. They affect how well patients do and what treatments they get, like heart transplant data from the United Network for Organ Sharing (UNOS).
Survival rates are very important in making medical choices. They help doctors and patients see the risks and benefits of surgeries. By looking at surgery mortality rates and other stats, we can choose better treatments.
| Type of Surgery | 1-Year Survival Rate | 5-Year Survival Rate |
| Orthotopic Heart Transplantation | 85% | 75% |
| Coronary Artery Bypass Grafting | 95% | 85% |
| Major Organ Transplants | 80% | 70% |
Many things affect how well patients do after surgery. Knowing these factors helps improve care and survival chances. We look at what matters most for surgical success, helping patients and doctors get the best results.
A patient’s age and health are big factors in surgery success. Older patients or those with health issues face higher surgery risks. For example, a study on breast cancer survival found age and health are key.
Doctors can plan better care by checking these factors before surgery.
The surgery’s complexity also matters a lot. More complex surgeries, like organ transplants or heart procedures, are riskier. The skill and experience of the surgical team are very important in these cases.
The surgeon’s experience and the facility’s quality also affect survival rates. Doctors with more experience and working in top facilities usually get better results. This is shown in operation mortality statistics, showing the need for better care and facilities.
Improving surgery outcomes and patient care is a team effort. It involves the surgical team, the patient’s health, and the quality of care at the facility.
Some surgeries carry higher risks and lower survival chances. It’s important to understand these complexities. We look at surgeries that are tough for both doctors and patients, and what makes them challenging.
Transplanting major organs like hearts, livers, and lungs is a complex task. It involves swapping a sick organ with a healthy one from a donor. The United Network for Organ Sharing (UNOS) reports that survival rates vary.
For example, heart transplant success rates range from 85% to 90% after one year (Source: UNOS data). The complexity of these transplants isn’t just in the surgery. It also includes managing the patient’s immune system to avoid organ rejection.
High-risk heart surgeries, like coronary artery bypass grafting (CABG) in risky patients, are tough. These surgeries are for patients with severe heart disease. Success depends on many factors, including patient health, surgical skill, and post-op care.
Research shows CABG can greatly improve survival for some patients. But, the death rate can be between 2% to 5% or more for high-risk patients. Patient health, surgery complexity, and care quality all play a role.
Neurosurgeries for brain tumors or vascular issues need precise techniques and deep neuroanatomy knowledge. Success rates depend on the tumor’s location, patient’s health, and surgeon’s experience.
Thanks to better techniques, imaging, and care, survival rates for these surgeries have improved. Yet, they are risky and need careful patient choice and advice.
In summary, surgeries like organ transplants, high-risk heart surgeries, and complex neurosurgeries need a full grasp of their risks and challenges. By studying success rates and data, doctors can work to better patient outcomes and survival chances.
Looking at survival rates for different surgeries shows us how outcomes vary. This helps us understand what makes some surgeries more successful. It also shows where we can do better.
General surgery includes many procedures, like removing appendixes or fixing hernias. Specialty surgeries, like brain or heart surgeries, are more complex and delicate. Studies show survival rates differ between these types.
General surgeries usually have better survival rates because they are simpler. But, specialty surgeries have seen big improvements in technology and techniques. This has led to better results over time.
Key differences in survival rates between general and specialty surgeries include:
Emergency surgeries are urgent and present unique challenges. Patients may face higher risks due to their condition, other health issues, or lack of preparation.
Research shows emergency surgeries have lower survival rates than planned surgeries. But, better emergency care and surgical techniques are helping improve these outcomes.
Factors influencing emergency surgery outcomes include:
By studying surgical outcome data and surgery survival statistics, we can learn more about different surgeries. This helps us aim to improve operation outcome data for everyone.
| Surgery Type | Survival Rate | Key Factors Influencing Outcome |
| General Surgery | Higher | Less complex, better preoperative care |
| Specialty Surgery | Variable | Complexity, surgeon expertise, technology |
| Emergency Surgery | Lower | Urgency, patient condition, timeliness of intervention |
The impact of where you live on your health care is big. It affects how easy it is to get good care. This can change how well you do after surgery.
Where you live affects how easy it is to see a doctor. Cities usually have better hospitals and more doctors than rural areas.
This means city folks might do better after surgery. They get care faster and from experts.
How well you do after surgery also depends on where you are. Different places have different levels of care and doctors.
| Region | Surgical Survival Rate (%) | Average Hospital Stay (Days) |
| Urban | 95 | 7 |
| Rural | 85 | 10 |
| Suburban | 90 | 8 |
Knowing these differences is key to making care better everywhere. By looking at surgery statistics mortality and operation success rates, we can work to improve surgical survival rates everywhere.
We are seeing big changes in how well surgeries work out thanks to new tech and techniques. These advancements are making patients do better and changing surgery for the better.
New tech and better surgery methods are leading to better surgical outcome statistics. A big area where this shows up is in new surgery techniques. These techniques help patients heal faster and lower the chance of problems.
Surgeons are always getting better at their jobs to boost surgery outcome rates. Some key improvements include:
These changes have made surgeries safer for people all over the world by lowering operation mortality statistics.
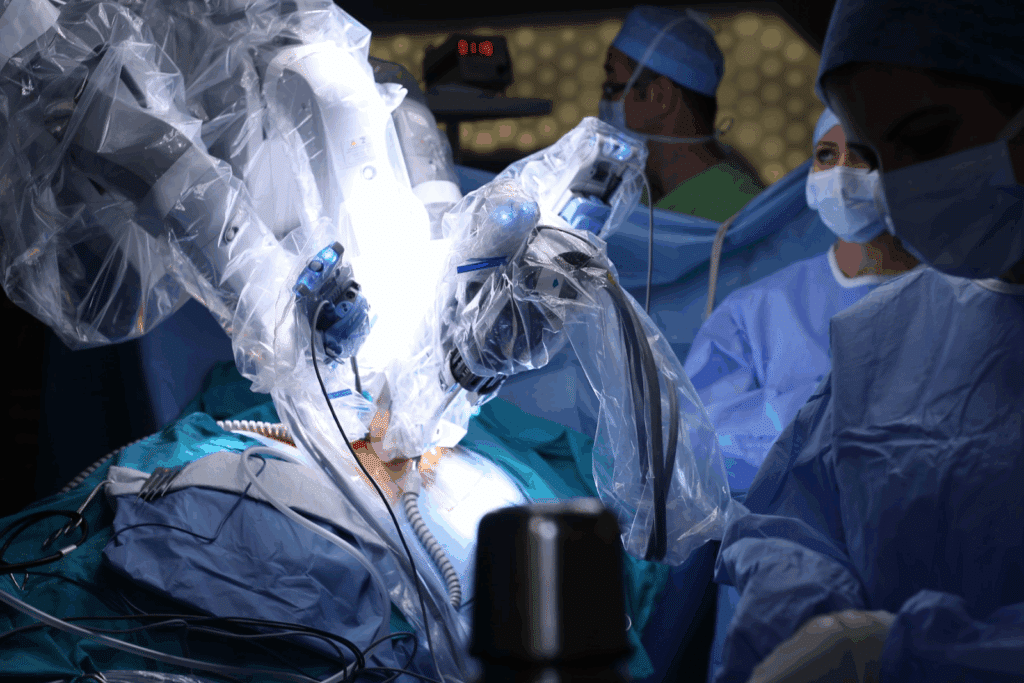
Technology and robotics are becoming more important in surgery. Robotic-assisted surgery, for example, gives surgeons more control and precision. This makes it possible to do complex surgeries more accurately.
“The use of robotics in surgery has opened new avenues for precision and minimal invasiveness, significantly impacting patient recovery and outcome.”
A study on robotic-assisted surgery outcomes
Technology not only makes surgery more precise but also helps train surgeons better. This leads to surgeons who are more ready to care for patients, which means better care for everyone.
As we keep using these new tools and methods, we’ll see even better surgical outcome statistics and fewer risks in surgery.
Understanding the risks of surgery is key. It means looking at many factors that could affect the surgery’s success.
Before surgery, doctors do important checks. They look at your medical history, do a physical exam, and run tests.
Studies show these checks can lower surgery death rates. For example, the United Network for Organ Sharing (UNOS) found that picking the right patients and doing thorough checks are vital for heart transplant success.
The informed consent process is also vital. It makes sure patients know the risks and benefits of their surgery.
Good informed consent means talking clearly about the surgery. This includes the risks, benefits, and other options. It respects patients’ choices and helps manage their worries.
| Risk Factor | Description | Mitigation Strategy |
| Patient Age | Older patients may have higher risks due to comorbidities. | Comprehensive geriatric assessment. |
| Surgical Complexity | More complex surgeries have higher risks of complications. | Surgeon experience and team expertise. |
| Pre-existing Conditions | Conditions like diabetes or heart disease can increase surgical risks. | Optimization of pre-existing conditions before surgery. |
By understanding and assessing these risks, doctors can give better advice. This helps improve surgical mortality data and operation survival rates.
Many factors affect long-term survival after surgery. These include how often the disease comes back and the care patients get after surgery. Looking into these details helps us improve how well patients do after surgery.
How often the disease comes back is key to long-term survival. The chance of it coming back changes based on the surgery type, disease stage, and patient health. For example, catching breast cancer early can lower the chance of it coming back, which helps patients live longer.
Let’s look at some data to see how recurrence rates affect survival:
| Surgery Type | Recurrence Rate | 5-Year Survival Rate |
| Breast Cancer Surgery | 20% | 80% |
| Colorectal Cancer Surgery | 30% | 60% |
| Prostate Cancer Surgery | 10% | 90% |
Getting regular check-ups is vital for long-term survival after surgery. These visits help doctors catch problems early, which can lead to better treatment results. We suggest a plan that includes:
By focusing on follow-up care, we can greatly improve patients’ quality of life and survival chances. It’s a team effort between doctors and patients to get the best results.
Patients need reliable info and support when thinking about surgery. We offer an overview of resources like support groups, counseling, and websites. These help patients understand the surgical process.
Studies show support groups and counseling are key for patients. They offer emotional support and a sense of community. This is very helpful for those facing surgery.
By looking at surgical success data, patients can make better choices. They can understand their options better.
Websites and databases give patients important info on surgery success rates. They help patients weigh the risks and benefits of different surgeries. This way, patients can make informed decisions about their care.
Surgery survival rates show how many patients make it through an operation. They’re key to knowing the risks and results of different surgeries. This helps doctors make better choices and patients know what to expect.
A patient’s age, health, and any existing conditions greatly affect their surgery survival rate. Older patients or those with health issues might face higher risks, which can lower their survival chances.
The complexity of a surgery is a big factor in survival rates. More complex surgeries, like organ transplants or high-risk heart surgeries, have lower survival rates. This is because they’re more challenging and come with higher risks.
The surgeon’s experience and the healthcare facility’s quality are very important. Surgeons with more experience and top-notch facilities tend to have better survival rates.
Yes, survival rates vary between general and specialty surgeries. Specialty surgeries, like neurosurgeries or cardiac surgeries, have different rates. This is because of their complexity and the specific conditions they treat.
Where you live can affect your surgery outcome. This is because of differences in healthcare access and quality between cities and rural areas. Also, there are regional differences in surgical care and policies.
New surgical techniques, technology, and robotics are boosting survival rates. These advancements lead to more precise and less invasive surgeries. This reduces risks and helps patients recover faster.
To assess surgery risks, thorough pre-surgical checks and informed consent are needed. These steps help both doctors and patients understand the risks and benefits of a surgery.
Long-term survival after surgery is key for patients’ health and quality of life. Factors like how likely the condition is to come back and the quality of follow-up care greatly affect long-term survival.
Patients looking into surgery have many resources. These include support groups, counseling, and websites with information. These resources help patients make informed decisions about their care.
Reliable info on surgery outcomes can be found through reputable health organizations, journals, and government health departments. These sources offer accurate and current data on surgical results.
Survival data from operations is critical for making medical decisions. It helps doctors and patients understand the risks and possible outcomes of surgeries. This leads to more informed choices about treatment.
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/40130129/
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!