Last Updated on November 25, 2025 by
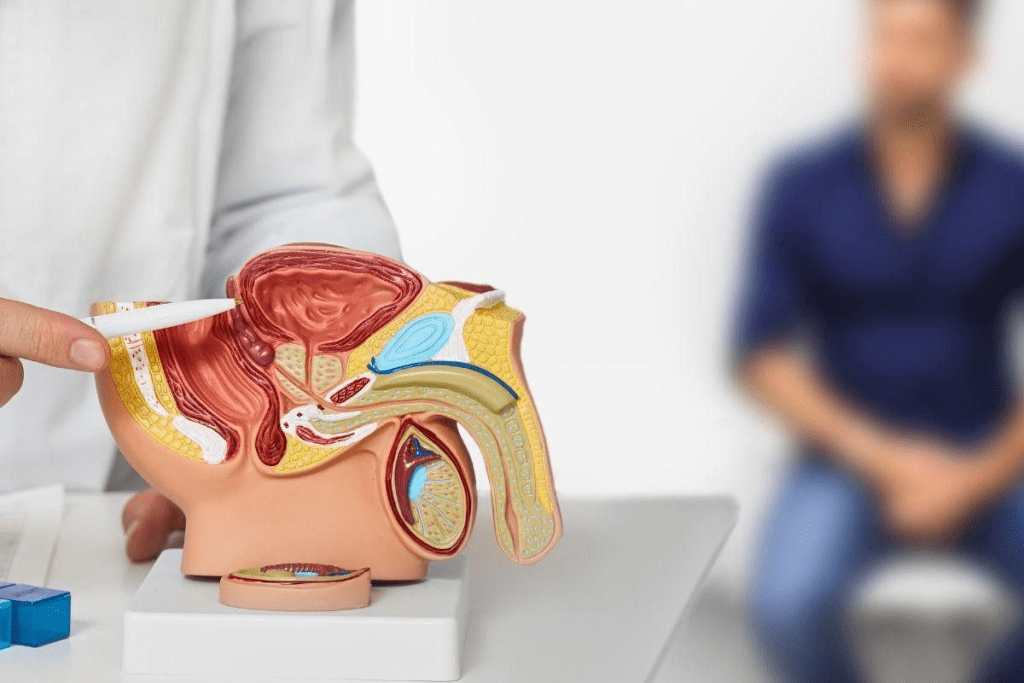
Prostate surgery, like radical prostatectomy, is a big deal. It involves taking out the prostate gland. We see it as a major surgery because it’s complex, needs anesthesia, and can have side effects afterward.

The goal of this surgery is to get rid of prostate cancer. It’s a key treatment for many. The risks and challenges of prostate removal make it a big step for patients.
It’s important for patients to know what prostate surgery is about. This helps them get ready for what might happen and how they’ll recover.
Prostate surgery is considered a major operation. This is because it’s complex, needs anesthesia, and has a long recovery time. It involves removing the prostate gland, mainly to treat cancer.
A major surgery is complex, needs general anesthesia, and has a long recovery. It often involves big cuts or special techniques like laparoscopy or robotics. “Major surgeries are those that carry significant risks and require careful preoperative planning and postoperative care,” say medical experts.
“Surgical procedures are considered major based on their complexity, the medical risks, and the impact on the patient’s recovery and quality of life.”
Medical Expert
Prostate surgery is major because of its detailed nature and possible long-term effects. It can be done in different ways, like open surgery, laparoscopic surgery, or robotic-assisted surgery. Each method has its own recovery and risk considerations.
Prostate surgery is major for several reasons. It’s in a delicate area, needing great skill. It also affects urinary and sexual functions after surgery.
The prostatectomy surgery is complex, with methods like robotic prostatectomy needing careful post-op care. The choice of surgery depends on the patient’s health, the surgeon’s skills, and the case’s needs.
In conclusion, prostate surgery is a major operation. It’s complex, needs careful care before and after, and affects recovery and quality of life greatly.
There are several ways to do radical prostatectomy surgery. Each method has its own good and bad points. The choice depends on the patient’s health and the surgeon’s skill.
Open radical prostatectomy is a traditional surgery. The surgeon makes one big cut in the belly to get to the prostate. This method is chosen based on the patient’s needs and the surgeon’s opinion.
This surgery takes longer to recover from than some newer methods. But it’s a good choice for many patients needing prostate removal.
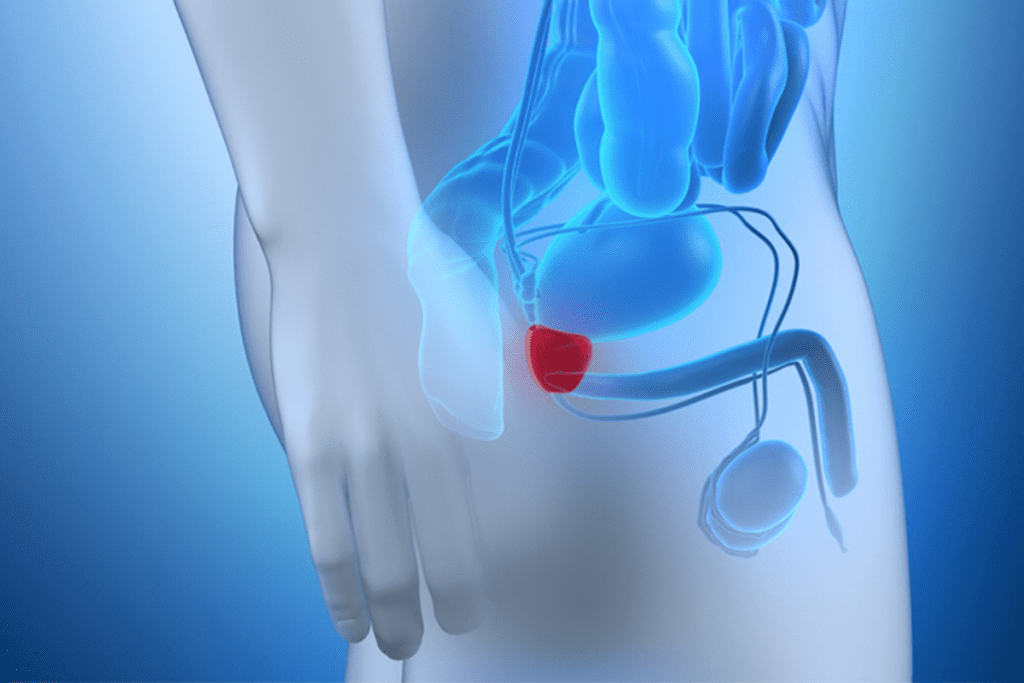
Robotic-assisted laparoscopic prostatectomy is a newer, less invasive surgery. It uses a robotic system to help the surgeon. This technique is more precise and flexible, making it easier to work around the prostate.
Patients who have a robotic prostatectomy usually lose less blood and recover faster. The robot gives a clear view of the area, helping to save nerves.
Laparoscopic radical prostatectomy is another less invasive surgery. It uses a laparoscope through small cuts. This way, the surgeon can see and work inside the body without big cuts.
Laparoscopic prostatectomy causes less damage, hurts less after, and you can go home sooner. The choice between laparoscopic and robotic-assisted depends on the surgeon and the patient’s needs.
It’s important for patients to know about the different radical prostatectomy surgeries. Each has its own benefits and downsides. The right choice is made based on each patient’s situation.
Knowing what to expect after prostate surgery can help ease your worries. The type of surgery you have affects your stay in the hospital and how you recover.
The time you spend in the hospital varies with the surgery type. For example, most robotic prostate cancer surgery patients go home the next day. The usual stay for robotic prostatectomy is one to two days. Some might even go home the same day as surgery.
Hospital Stay Comparison by Surgery Type:
Remember, everyone recovers differently. Your healthcare team will guide you based on your needs and progress.
In the first week, you might feel some pain, tiredness, and discomfort. This will be managed with medication. You’ll also get instructions on catheter care if needed. It’s important to follow these steps to avoid complications.
The first week can be tough, but with the right support, you can get through it. Your medical team will be in touch, answering your questions and checking on your recovery.
Having a support system is key during this time. It could be family, friends, or a caregiver. They can help with daily tasks and offer emotional support.
The recovery after prostatectomy is a key time that needs careful handling and patience. We’ll help you understand the recovery process to make your return to normal life easier.
In the first weeks after surgery, it’s important to avoid hard activities. Light walking is good for blood flow and preventing clots. But, stay away from heavy lifting and bending.
As you get better, you can start doing more. Always listen to your surgeon about what you can do. Usually, you can get back to your usual life in 6-8 weeks.
Looking after your catheter and wound is key to recovery. You’ll likely have a catheter for 1-2 weeks after surgery. Keep the wound clean and dry, and follow your doctor’s advice for dressing changes.
“Proper wound care and catheter management are vital for avoiding infections and a smooth recovery.”
Expert Opinion
When you can go back to work depends on how you’re healing and your job. Desk jobs might be easier to get back to than jobs that are hard on your body. Always talk to your surgeon before going back to work.
By knowing the recovery journey after prostatectomy and following the right steps, you can have a successful recovery. This way, you can get back to your usual activities.
The journey to recovery after prostate surgery is long. Knowing about urinary continence and sexual function can help. It’s important to look at the different factors that affect recovery.
Many men regain control over their bladder after prostate surgery. Between 79% to 94% of patients get better within 12 months. This is a key part of feeling well again.
Recovering sexual function is also key. The numbers vary, with 10% to 67% of men getting better in 1 to 3 years. Age, health, and the surgery method all matter.
Success in prostate surgery is about bladder control, sexual function, and cancer control. Up to 60% to 70% of men do well in these areas within 4 years. Knowing these stats helps set realistic hopes for life expectancy after prostate removal and prostate removal side effects.
Every person’s recovery is different. While stats give a general view, individual results can vary. Things like surgeon experience, surgical approach, and patient health greatly affect recovery. Understanding these can help patients make better choices for their care.
It’s important to know what makes prostate surgery successful. This knowledge helps both patients and doctors. We’ll look at the key factors that affect the outcome of such a big operation.
Age and health before surgery are very important. Younger patients with fewer health problems usually do better. Health issues like diabetes or heart disease can make recovery harder. We think about these things when deciding if surgery is right for someone.
The surgeon’s experience and the hospital’s volume are key. Surgeons who do many prostate surgeries tend to do better. Hospitals that do a lot of these surgeries also have better care.
Choosing the right surgery is very important. Different methods, like robotic or laparoscopic, have their benefits. The best method can reduce problems and help recovery.
By looking at age, health, surgeon experience, hospital volume, and surgical method, we can understand what makes prostate surgery successful. This helps make better treatment choices.
Prostate surgery, like robotic prostatectomy and prostate removal, is a complex operation. It has significant effects after the surgery. We talked about the different parts of prostate surgery, from its major operation status to the recovery outcomes.
The success of prostate surgery depends on many things. These include the patient’s health, the surgeon’s experience, and the surgical method. Knowing these can help patients understand their treatment better. For more information, check out studies on PubMed Central.
At our institution, we aim to provide top-notch healthcare. We offer full support and guidance to international patients. Our team works hard to give personalized care during recovery, aiming for the best results for prostate surgery patients.
Prostate surgery, or prostatectomy, is when the prostate gland is removed. It’s major because it’s complex, needs anesthesia, and has a long recovery.
There are three main types: open radical prostatectomy, robotic-assisted laparoscopic prostatectomy, and laparoscopic radical prostatectomy. Each has its own recovery time and risks.
Recovery usually takes 6-8 weeks. You’ll need to manage your physical limits, care for your wounds, and slowly get back to work.
Right after surgery, you’ll deal with pain, manage your catheter, and go to follow-up appointments. How long you stay in the hospital depends on your surgery.
Long-term, most men regain urinary control (79-94% at 12 months) and some regain sexual function (10-67% at 1-3 years). Success rates are around 60-70%.
Yes, living without a prostate is possible. After surgery, men can lead active lives, but may face some side effects.
Success depends on your health, the surgeon’s skill, and the surgery type. Knowing these can help make treatment choices.
The prostate gland is key in the male reproductive system, making semen. Removing it can affect urination and sex.
Side effects include urinary incontinence, erectile dysfunction, and other issues. Managing these is key to recovery.
Robotic prostatectomy is a precise method that can reduce blood loss and recovery time. But, like any surgery, it carries risks.
Surgery can be done open, laparoscopic, or robotic-assisted. The choice depends on your health and the surgeon’s experience.
Ficarra, V., Novara, G., Ahlering, T. E., et al. (2024). Comparison of the effectiveness of open, laparoscopic, and robotic radical prostatectomy: A multicenter cohort study. BMC Urology. https://bmcurol.biomedcentral.com/articles/10.1186/s12894-024-01597-3
Tewari, A., Srivastava, A., & Löhnert, M. (2021). Functional and oncological outcomes after open versus robot-assisted radical prostatectomy: Surgeon heterogeneity matters. European Urology. https://www.europeanurology.com/article/S0302-2838%2821%2901928-X/fulltext
Post-prostatectomy urinary incontinence: Etiology, evaluation, and management. (2015). PMC (National Institutes of Health). https://pmc.ncbi.nlm.nih.gov/articles/PMC4548645/
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!