Last Updated on November 14, 2025 by
Going under the knife can be scary, and you might wonder how we make sure you’re really asleep. General anesthesia is a complex mix of medicines, called anesthetics, to make you sleep like you’re dreaming.
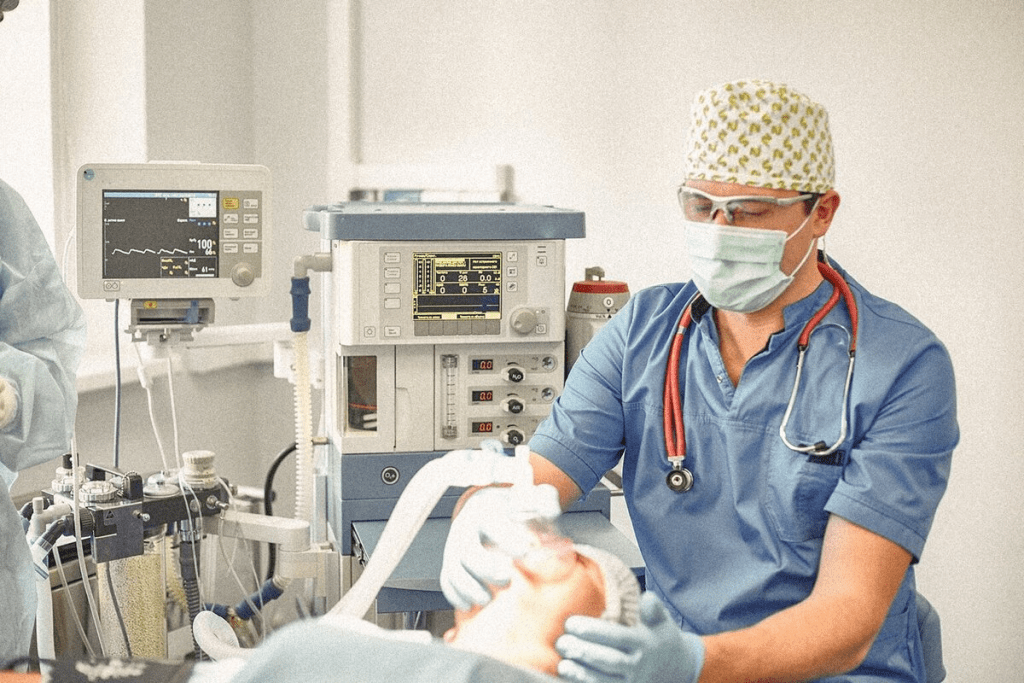
We use many ways to keep you safe and comfy. We watch you closely, check your vital signs, and use special brain activity monitors. This way, you stay asleep and pain-free, avoiding the rare but scary anesthesia awareness.
Anesthesia is more than just being ‘asleep’. It’s a carefully controlled state of unconsciousness. We use precise medical interventions to achieve this. When we give anesthetics, we’re not just putting patients to sleep. We’re creating a complex state that needs deep knowledge of neuroscience, pharmacology, and clinical skills.

When anesthetics take effect, they change brain activity a lot. Anesthetic drugs block the brain’s ability to send information between regions. This disconnects different parts of the brain.
Many anesthetics work by binding to GABA receptors. They activate interneurons to slow down the brain. This changes brain waves to low-frequency patterns. Patients become unresponsive to surgical stimuli.
Anesthetics enhance inhibitory activity in the brain. This creates a stable state that’s different from natural sleep. It’s key for keeping patients pain-free and unaware during surgery.
Surgical unconsciousness is different from natural sleep. Both states have reduced consciousness, but the reasons are unique. Anesthetics control the brain’s electrical activity, keeping it in a stable state. This is not seen in natural sleep cycles.
Natural sleep has various stages, like REM and non-REM sleep. These stages have different brain wave patterns and levels of consciousness. Anesthesia-induced unconsciousness is a uniform state. It’s kept by constant anesthetic drug administration. This state prevents patients from feeling pain or responding to surgery, making it vital for modern surgery.
To confirm unconsciousness, we watch for several key signs. These signs show if anesthesia is working well. They help make sure patients are comfortable and asleep during surgery.
We first check the eyelash reflex. It usually gets weaker as anesthesia kicks in. We also look at pupil response. Small pupils mean the anesthesia is strong enough.
Studies show that pupil size can tell us how deep the anesthesia is (Source).

We check muscle tone and look for body movement. As anesthesia gets stronger, muscles relax more. This shows the patient is ready for surgery.
Another important sign is how the patient reacts to verbal commands and other things. When they stop responding, it means the anesthesia is working well.
We also watch lacrimation (tear production) and salivation patterns. Changes in these can tell us how deep the anesthesia is. For example, less salivation means deeper anesthesia.
We also look at heart rate, blood pressure, and breathing patterns. These signs help us understand the patient’s overall health during local anesthesia or general anesthesia.
By watching these signs closely, we can adjust the anesthesia. This ensures the patient stays comfortable and safe. Knowing anesthesia is what and how it affects patients helps us give the best care. For those asking anesthesia what is, it’s a way to make surgery painless by making patients unconscious.
When we give general anesthesia, we watch vital signs closely to keep patients safe. Monitoring vital signs is key in anesthesia care. It lets us see how the patient is doing in real-time.
We keep an eye on heart rate and blood pressure to make sure the heart and blood vessels are okay. Heart rate monitoring helps spot heart rhythm or rate problems. Blood pressure monitoring checks how well blood is flowing.
Changes in heart rate or blood pressure might mean trouble, like bleeding or heart problems. By watching these signs, we can act fast to keep the patient safe during the procedure.
Watching how a patient breathes is also very important. We check breathing patterns to make sure they’re breathing right. We also look at oxygen saturation to see if the blood has enough oxygen.
This helps us catch any breathing problems early. We can then fix them to keep the patient safe.
We also watch other important signs like temperature and CO2 levels. Checking the temperature helps us see if the patient is too hot or too cold. CO2 monitoring shows if the patient is breathing well.
By keeping these signs in check, we make sure the patient stays safe and stable. This reduces the chance of problems with general anesthesia, such as knowing what is general anesthesia and how it affects people.
We use the latest brain activity monitoring technologies to keep patients safe. These tools help us check if anesthesia is working correctly. This way, patients stay comfortable and don’t wake up during surgery.
Bispectral index (BIS) monitoring is the top choice for checking anesthesia levels. It looks at the brain’s electrical activity to see how awake a patient is. Keeping BIS levels between 40 and 60 helps avoid intraoperative awareness.
Other tools, like entropy and AEP, also help us understand brain activity. Entropy looks at how random the brain’s signals are. AEP checks how the brain reacts to sounds. These tools give us more information to make anesthesia better.
Brain monitoring technologies are key in stopping intraoperative awareness. They help us make sure patients don’t wake up during surgery. This makes them safer and more comfortable. Studies show BIS monitoring helps by making anesthesia more precise.
In short, brain monitoring is vital in today’s anesthesia care. It helps us give our patients the best care. This way, we reduce risks and make their surgery better.
Comprehensive monitoring is key to keeping patients safe during general anesthesia. It helps reduce the risk of anesthesia awareness and other complications.
We use a mix of clinical observation, vital sign monitoring, and advanced brain activity monitoring. This way, we can give patients the best care possible. It helps us see how the anesthetic is working and make changes if needed.
Our goal is to keep improving in anesthesia care while always focusing on patient safety. With these monitoring strategies, we aim to make sure patients have a safe and effective anesthetic experience.
General anesthesia makes patients unconscious. It uses anesthetics to change brain activity. This way, patients don’t feel pain or discomfort during surgery.
We check patients with clinical observations and vital signs. We also use advanced brain activity monitors. This ensures they are comfortable and asleep.
Anesthetics bind to GABA receptors, which enhances inhibitory activity. This changes brain waves, disconnecting brain regions. It prevents information transmission.
Anesthesia’s duration varies by procedure and patient health. We monitor patients closely for a smooth recovery.
We watch eyelash reflex and pupil response. We also check muscle tone, body movement, and verbal responses. Other indicators help us adjust anesthesia levels.
BIS monitoring is a key tool for assessing anesthesia depth. It provides a quantitative measure. This helps prevent patients from becoming aware during surgery.
Anesthesia is generally safe but can cause nausea, vomiting, and dizziness. We work to minimize these effects and ensure patient comfort.
Anesthesia can change heart rate, blood pressure, and breathing. We monitor these closely to keep patients safe.
Intraoperative awareness is a rare condition where patients are conscious during surgery. We use BIS monitoring and other technologies to prevent it.
Anesthesia is different from natural sleep. Anesthetics control brain activity, while sleep involves various stages. Anesthesia keeps the brain in a stable state.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!