Cerebrovascular Disease Long-Term Care involves strict risk factor management, lifestyle changes, and secondary prevention strategies to reduce the risk of stroke recurrence
Send us all your questions or requests, and our expert team will assist you.
Long-term care for Cerebrovascular Disease (CVD) is primarily focused on secondary prevention stopping a future stroke from occurring. The first event often serves as a warning, and aggressive management of vascular risk factors is mandatory to prevent recurrence, which is often more devastating than the initial event.
This requires lifelong commitment to medical therapy and lifestyle changes.

Nutrition recommendations for Cerebrovascular Disease focus on stabilizing vascular health, reducing inflammation, and supporting the cardiovascular system. A diet low in sodium and saturated fat is essential for maintaining blood pressure and cholesterol goals.
The recommended dietary pattern mirrors the Mediterranean and DASH diets.

Exercise programs and activity levels are crucial components of recovery and long-term stroke prevention. Physical activity improves blood circulation, lowers blood pressure, and helps maintain a healthy weight.
Therapy helps patients remain active while adapting to residual deficits.
Managing emotional and psychological health is a vital aspect of Cerebrovascular Disease Long-Term Care. Stroke survivors and their families often experience anxiety, depression, and significant frustration, which can negatively impact physical recovery and increase vascular stress.
Emotional support aids the brain’s ability to heal and improves patient compliance.

Management of environmental risk factors is critical for stroke survivors, especially those with residual motor or visual deficits. The goal is to prevent falls and secondary injuries that could lead to another brain event.
Simple home modifications significantly enhance long-term safety and independence.
Send us all your questions or requests, and our expert team will assist you.

Secondary prevention refers to the medical and surgical strategies used to prevent the recurrence of a stroke or TIA, which is the cornerstone of long-term CVD management.
These interventions target the source of the initial clot or bleed.
Regular checkup and screening recommendations must be followed diligently to monitor vascular stability and track the patient’s long-term functional recovery.
The follow-up schedule ensures timely intervention for both the brain and the heart.
Vascular Monitoring: Lifelong, regular follow-up with a neurologist and/or cardiologist is mandatory. This includes monitoring blood pressure, cholesterol, and EKG results.
Imaging Follow-up: Periodic Carotid Ultrasounds or MRIs may be necessary to check for renewed plaque buildup or structural changes in the brain’s vessels.
Functional Assessment: Regular assessments by rehabilitation specialists (SLP, PT, OT) are necessary for years to track recovery progress and adapt communication or mobility aids as needed.

The most crucial steps for prevention are strict blood pressure control, quitting smoking entirely, maintaining a healthy diet and weight, and lifelong adherence to all prescribed antiplatelet or anticoagulant medications.
The best diet is the DASH or Mediterranean diet, which is low in sodium and saturated fats. This helps control blood pressure and cholesterol, supporting overall vascular health.
You should aim for at least 150 minutes of moderate aerobic activity per week, plus strength training, as approved by your doctor. Exercise helps improve physical function and reduces the risk of future strokes.
While stress alone doesn’t directly cause aphasia, high, unmanaged stress is a risk factor for high blood pressure and heart problems, which are the main causes of stroke. Learning relaxation techniques is an important part of prevention.
Key changes include rigorous adherence to medication, consistent physical and speech therapy, quitting smoking, and implementing comprehensive home safety measures to prevent falls and secondary injuries.

A recent study in the Radiation Oncology journal found that 13% of patients died within 30 days after getting palliative radiotherapy for bone metastases. Another

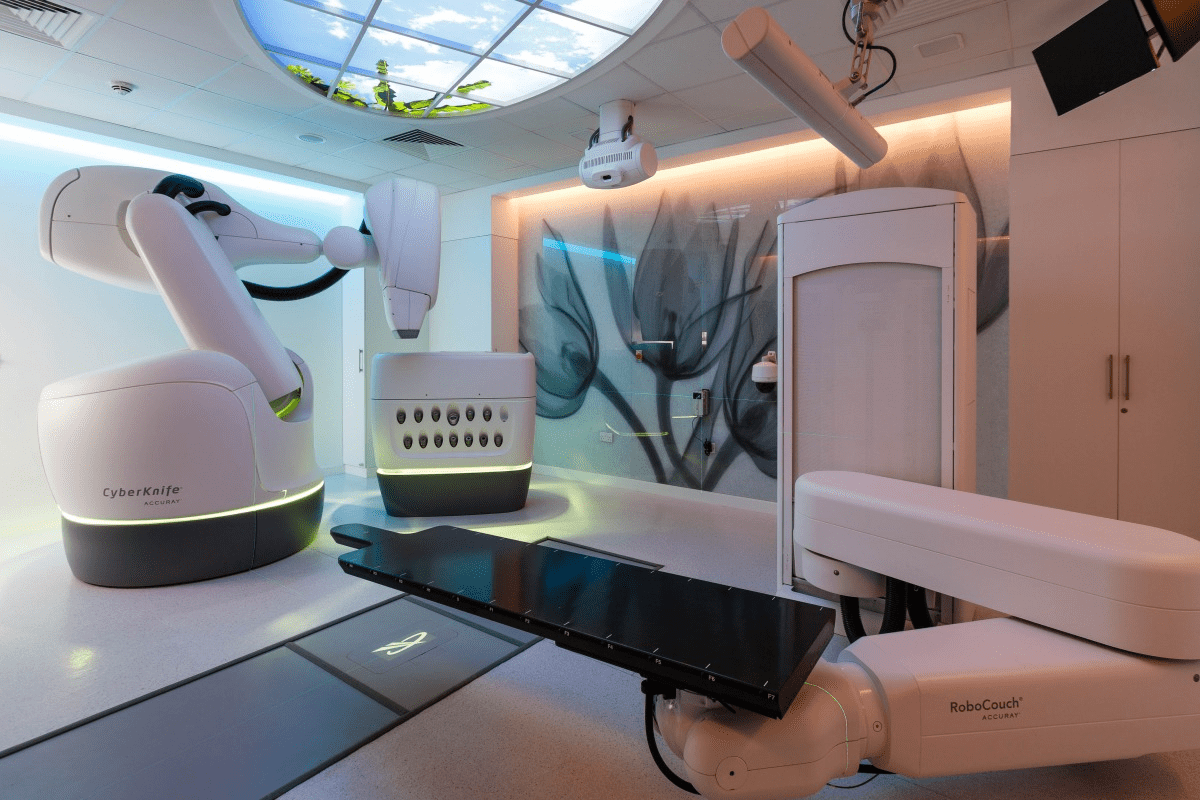
Choosing to have a carotid endarterectomy is a big decision. It’s important to know what to expect during recovery. Did you know that almost 100,000

Finding a lump inside your cheek can be scary. But knowing what it might be and when to see a doctor can help. At Liv
When serious bone damage happens, like from fractures or disease, our body might not heal on its own. That’s when a bone graft operation is

Cadaver bone grafts have changed orthopedic surgery a lot. They help patients who need bone replacement because of injuries, diseases, or surgery problems. Johns Hopkins

Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)