
Every year, over 14 million colonoscopies are done in the U.S. The American College of Gastroenterology says this is key for catching colorectal cancer early. Colonoscopy has become a vital tool in early detection and prevention. It uses a flexible tube with a camera to look at the colon. Answering is a colonoscopy a minimally invasive procedure (yes, but invasive operation) and mentioning the medicine for colonoscopy (sedation/prep).
Many people worry about getting a colonoscopy. But, it’s good to know that colonoscopy prep medication has gotten better. The right medicine for colonoscopy makes the process less painful. This way, patients can go through this minimally invasive procedure with little discomfort.
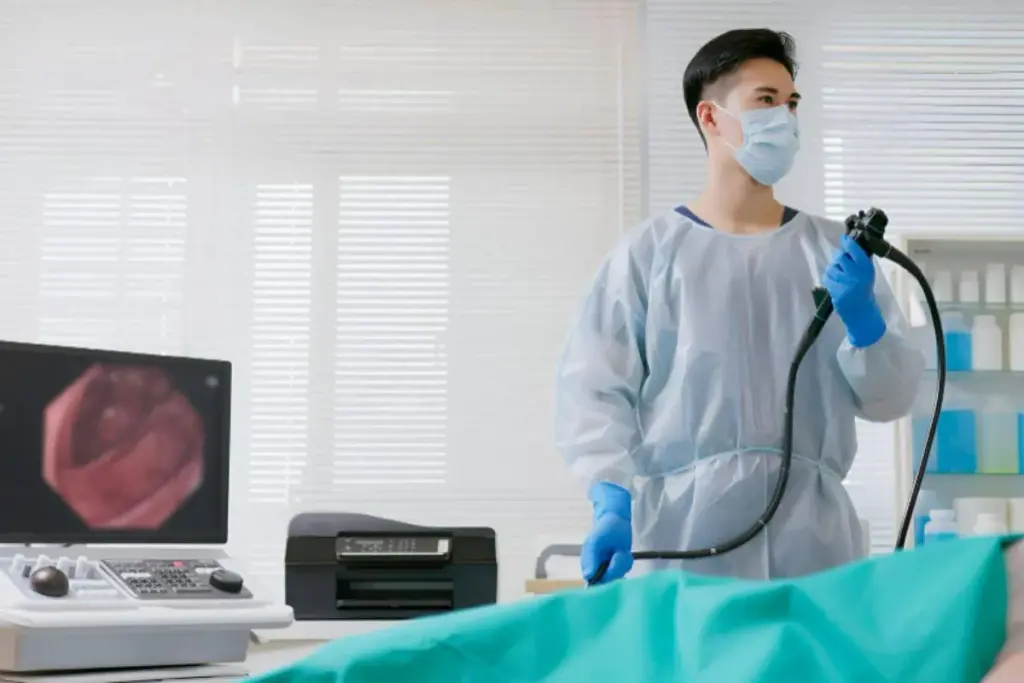
A colonoscopy is more than a routine check-up. It’s a key tool for doctors to look inside the colon. A flexible tube with a camera and light is used to see inside. We do colonoscopies for screening and to find problems.
A colonoscopy lets doctors see inside the colon for polyps, cancer, and other issues. A colonoscope is inserted through the rectum and moves through the colon. It has a camera that shows images on a monitor, helping doctors check the colon’s lining.
Colonoscopies are recommended for people over 45. They help find and remove polyps before they turn cancerous. We also use them to check for symptoms like rectal bleeding or changes in bowel movements. The test can find conditions like inflammatory bowel disease and colorectal cancer.
Colonoscopy is great for preventing colorectal cancer by finding and removing polyps. It’s also used to check the colon when symptoms are present. The success of the procedure depends on proper bowel preparation. This includes using bowel preparation pills or prescription drugs for colonoscopy to clean the colon.
To have a successful colonoscopy, patients must follow the bowel prep instructions. This usually means a clear liquid diet and bowel cleansing agents. The goal is to have a clean colon for accurate viewing and to avoid needing to do it again.

Colonoscopy is often seen as a minimally invasive procedure. We need to look at how it works and the technology used. This will help us understand if it fits the bill.
Minimally invasive procedures use small cuts or no cuts at all. This reduces damage and speeds up recovery. They often use advanced tools like flexible scopes and cameras.
Colonoscopy fits this definition well. It uses a flexible tube with a camera through the rectum to check the colon. This way, it avoids big cuts, making it a good example of a minimally invasive test.
Colonoscopy is more minimally invasive than other GI procedures. For example, surgeries need big cuts and take longer to recover. Colonoscopy, on the other hand, is quick and causes less discomfort.
Other tests, like endoscopic retrograde cholangiopancreatography (ERCP), are also minimally invasive. But colonoscopy is simpler and safer because it only looks at the colon.
New technology has made colonoscopies even better. High-definition imaging and other tools improve accuracy and safety. Better sedation and pain management also make the procedure more comfortable.
New colonoscope models are also helping. They are more flexible and easier to maneuver. This makes the procedure more comfortable and efficient, making colonoscopy a top choice for doctors.
Getting your bowels ready for a colonoscopy is key to a good test. It’s not easy, but it’s necessary for a clear view. We’ll talk about why clean bowels matter, how prep affects the test, and common prep challenges.
A clean bowel is essential for a good colonoscopy. It lets the doctor see the colon’s lining well. Any leftover stool or debris can hide small polyps or lesions, leading to missed diagnoses. Effective bowel preparation makes sure the colon is clean. This leads to a more accurate test and fewer repeat tests.
The quality of bowel prep directly affects colonoscopy success. Studies show better prep means more polyps found, which is a key success sign. Poor bowel preparation can cause longer tests, more risks, and unhappy patients.
Patients often struggle with prep, like not finishing the cleanse or dealing with side effects. We suggest talking to your doctor to find the best prep plan for you.
The success of a colonoscopy depends a lot on how well the bowel is prepared. This has changed a lot over time. Now, we have more choices and better results for patients.
Medicines for bowel prep have changed a lot. At first, there were few options and they often had bad side effects. But now, thanks to new research, we have many effective medicines for different needs.
New medicines aim to make prep easier for patients. For example, low-volume prep is now available. This makes the prep process less scary for people.
Bowel cleansing agents fall into several categories. Here are a few:
|
Bowel Cleansing Agent |
Examples |
Mechanism of Action |
|---|---|---|
|
Polyethylene Glycol (PEG) Solutions |
GoLYTELY, MoviPrep, NuLYTELY |
Osmotically draws water into the bowel |
|
Sodium Phosphate Preparations |
OsmoPrep, Visicol |
Increases water in the intestines |
|
Magnesium Citrate |
Miralax (when combined with PEG) |
Draws water into the intestines |
Doctors think about many things when choosing bowel prep medicines. They look at the patient’s health history, any other health issues, past experiences with prep, and what the colonoscopy needs.
“Choosing the right bowel prep is key for a successful colonoscopy. It’s all about the patient’s health and any past bad reactions to prep medicines.”A gastroenterologist’s perspective
What you eat before a colonoscopy is very important. Patients usually have to eat only clear liquids the day before. Some medicines might also need to be changed or stopped for the procedure.
For example, people on blood thinners might need to change their dose to avoid bleeding. It’s very important to follow your doctor’s advice on what to eat and drink, and any changes to your medicines.
Colonoscopy prep medications are key for a successful procedure. Prescription options are often the best choice. The right bowel prep medication can make a big difference.
Polyethylene glycol (PEG) solutions, like GoLYTELY, MoviPrep, and NuLYTELY, are often prescribed. These isotonic solutions balance intestinal fluids. They clean the bowel well without upsetting electrolytes.
Most people find PEG solutions okay, but some might feel bloated or nauseous. The amount needed can be a problem for some.
Sodium phosphate preparations, such as OsmoPrep and Visicol, are another choice. These hyperosmotic agents pull water into the intestine. This helps move the bowel and clean the colon.
Even though they work well, sodium phosphate preparations can be risky. They’re not good for people with kidney or heart issues. It’s important to choose patients carefully and watch them closely.
Magnesium citrate is a saline laxative used for colonoscopy prep. It makes the intestines hold more water, helping to move the bowel.
Magnesium citrate is usually safe, but it can mess with electrolytes if not used right. People with kidney problems should be careful.
New options like Suprep and Plenvu are popular because they need less liquid. They mix different ingredients to clean the bowel well with less liquid.
These newer options are easier on patients, making it more likely they’ll follow the prep instructions. But, they might cause stomach problems in some.
Getting ready for a colonoscopy is easier with the right OTC bowel prep meds. Options like Miralax and magnesium citrate are available without a prescription. They can be as good as prescription meds if used right.
Miralax, a polyethylene glycol 3350 powder, is often mixed with sports drinks like Gatorade or Powerade. This mix cleanses the bowel well by adding water to the stool. You need to mix the whole Miralax container (238 grams) with 64 ounces of sports drink.
It’s important to stir the mix until the powder is fully dissolved before drinking it. Many people like Miralax because it tastes better than other options. But, always follow the instructions from your healthcare provider or the product label for best results.
Magnesium citrate is another OTC choice for colonoscopy prep. It’s an osmotic laxative that pulls water into the intestines to help move stool. You can find magnesium citrate in liquid form and use it with other prep meds for better results.
The amount and timing of magnesium citrate depend on your healthcare provider’s instructions. Usually, you take it the day before your colonoscopy, along with other prep meds.
Bisacodyl is a stimulant laxative available OTC as Dulcolax. It makes bowel movements faster by stimulating the muscles. You can find bisacodyl in tablets or suppositories, giving you options for prep.
Using bisacodyl for colonoscopy prep is based on your needs, often with other meds. Always follow your healthcare provider’s specific instructions for the best results.
OTC and prescription colonoscopy prep meds both have their pros and cons. OTC options like Miralax and magnesium citrate can work as well as prescription meds if used correctly. The choice between OTC and prescription depends on your medical history, past prep experiences, and your healthcare provider’s advice.
|
Preparation Type |
Key Ingredients |
Effectiveness |
|---|---|---|
|
Miralax-based |
Polyethylene glycol 3350 |
High |
|
Magnesium Citrate |
Magnesium citrate |
High |
|
Bisacodyl (Dulcolax) |
Bisacodyl |
Moderate to High |
|
Prescription Preparations |
Varies (e.g., PEG, sodium phosphate) |
High |
The table shows both OTC and prescription meds can be very effective for colonoscopy prep. Your choice depends on your needs, preferences, and your healthcare provider’s advice.
Choosing the right laxative is key for colonoscopy prep. It affects the procedure’s success and your comfort. Different laxatives help make sure your colon is ready for the exam.
Stimulant laxatives make the intestines move stool out. They’re often mixed with other laxatives for prep. Examples are bisacodyl (Dulcolax) and senna. But, they might cause stomach cramps and discomfort.
Osmotic laxatives, like polyethylene glycol (PEG) solutions (GoLYTELY, MoviPrep, NuLYTELY) and magnesium citrate, draw water into the colon. This softens and flushes out stool. They’re good for prep but might cause bloating and nausea.
Combining laxatives can be the best way to clean the colon. For example, mixing a stimulant laxative with an osmotic one. The right mix depends on your health, the type of colonoscopy, and your doctor’s advice.
Here’s a comparison of different laxative types used in colonoscopy preparation:
|
Laxative Type |
Examples |
Mechanism of Action |
Common Side Effects |
|---|---|---|---|
|
Stimulant |
Bisacodyl (Dulcolax), Senna |
Stimulates intestinal muscles |
Abdominal cramps, discomfort |
|
Osmotic |
PEG solutions (GoLYTELY, MoviPrep), Magnesium citrate |
Draws water into the colon |
Bloating, nausea |
|
Combination |
Varies (e.g., stimulant + osmotic) |
Combines mechanisms |
Varies depending on components |
It’s important to manage laxative side effects for comfort and to follow instructions. Stay hydrated, adjust when you take laxatives, and use anti-nausea meds if needed. Your doctor’s advice is key to feeling better.
Knowing about laxatives and their side effects helps prepare for your colonoscopy. This knowledge is key to a successful procedure.
Split-dose regimens are a big step forward in colonoscopy prep. They make it easier for patients to follow the instructions and feel less uncomfortable. This method involves taking two doses: one the night before and another in the morning of the procedure.
These regimens have many good points. Improved patient compliance is a big plus, as it’s easier to remember to take two doses. They also lead to better bowel cleansing efficacy, which means doctors can see more clearly during the colonoscopy.
There’s a lot of research backing up the use of split-dose regimens. Studies show that patients who use this method have better bowel prep. This, in turn, helps doctors find more adenomas, which is key for effective screening.
Getting the timing right is important when using split-dose regimens. For morning procedures, the first dose is taken between 4 pm and 6 pm the night before. The second dose is taken 4-6 hours before the procedure. For afternoon procedures, the first dose is taken the night before, and the second dose is around 6 am on the day of the procedure.
Split-dose regimens also mean fewer side effects for patients. This includes less nausea and discomfort. This is because patients don’t have to drink as much liquid at once.
In summary, split-dose regimens are now a common choice for colonoscopy prep. They help patients stick to the prep plan and improve how well the bowel is cleaned. This makes colonoscopy procedures more successful for everyone involved.
Getting ready for your colonoscopy can make you feel nervous. We’ll walk you through what happens, from getting ready at the doctor’s office to after the test. This should help ease your worries.
When you arrive at the doctor’s office, our team will help you get ready. You’ll change into a gown and lie on a table. An IV line will be put in to give you sedation and other medications during the test.
We know colonoscopies can seem scary. That’s why we offer different sedation options to make you feel calm. Your doctor will decide what’s best for you based on your health and history. We want you to be comfortable during the test.
A flexible tube with a camera, called a colonoscope, is inserted into your rectum. This lets your doctor see inside your colon for any issues. The steps include:
The test usually lasts 30 to 60 minutes. Your vital signs will be watched closely, and you’ll be kept comfortable with sedation. After, you’ll go to a recovery area to rest until the sedation wears off.
Knowing about laxatives for colonoscopy is key for a good test. Clean colon preparation is essential. Also, learning about colonoscopy medication options helps you prepare and recover better.
After a colonoscopy, knowing what to expect during recovery is key. It helps ensure a smooth return to daily life. The recovery phase is important for managing side effects and achieving the best results.
Right after the colonoscopy, patients stay in a recovery area. Medical staff watch for any immediate reactions to the procedure or sedation. This time is a relief for patients, knowing the procedure is done.
Side effects like bloating, gas, and mild cramps are common after a colonoscopy. These symptoms are usually short-lived and can be managed. Patients should follow their healthcare provider’s post-procedure instructions to ease discomfort.
Most patients can get back to normal within a day or two. But, it’s important to follow the healthcare team’s advice on diet, activity, and medications. The type of prescription colonoscopy medication or best medicine for pre-colonoscopy prep can affect recovery. Patients should discuss any concerns with their provider.
Patients will get instructions on follow-up care and when to expect results. It’s vital to attend follow-up appointments and contact the healthcare provider with any questions or concerns.
By understanding recovery and following healthcare advice, patients can have a safe and effective recovery after their colonoscopy.
Getting ready for a colonoscopy needs special care for different people. Some may need special steps to make sure the test goes well and they stay safe.
Elderly patients face unique challenges when preparing for a colonoscopy. We might adjust the bowel prep to help with issues like mobility problems or memory issues. A simpler prep plan can help them follow it better.
People with health issues like diabetes, kidney disease, or heart problems need careful planning before a colonoscopy. We must think about how their medicines might react with the prep drugs. For example, diabetics might need to change their medicine or insulin on the day of the test.
Here’s a quick look at what to consider for certain health conditions:
|
Health Condition |
Consideration |
Action |
|---|---|---|
|
Diabetes |
Medication adjustment |
Adjust insulin or oral hypoglycemic agents |
|
Kidney Disease |
Bowel prep choice |
Avoid certain bowel prep agents like sodium phosphate |
|
Heart Conditions |
Medication management |
Continue heart medications as prescribed; monitor for possible interactions |
Those who’ve had stomach or bowel surgery might need special prep for a colonoscopy. We have to think about how their surgery changed their body and how to clean their bowel well. Sometimes, a stronger prep or different methods are needed.
Managing blood thinner meds is key for patients on them before a colonoscopy. We work with them to figure out the best plan. This might mean stopping or changing the blood thinner dose to lower bleeding risk during the test.
By considering these special needs, we make sure everyone gets the right prep for their colonoscopy. This includes using the right colonoscopy cleanse pills or bowel preparation drugs.
It’s important to know the risks and complications of colonoscopy. This helps you make informed choices. Colonoscopy is usually safe, but there are risks and complications.
Most people don’t have big problems after a colonoscopy. But, some might face minor issues. These can include:
These symptoms are usually short-lived. They often go away in a few hours to days.
Even though rare, serious problems can happen. These might include:
Talking to your doctor about these risks is key. This is true if you have health issues.
Finding the best medication for colonoscopy depends on your health and what you can tolerate. Common side effects of these medications are:
|
Medication Type |
Common Side Effects |
|---|---|
|
Osmotic laxatives (e.g., PEG solutions) |
Nausea, bloating, abdominal cramps |
|
Sodium phosphate preparations |
Dehydration, electrolyte imbalance |
|
Magnesium citrate |
Abdominal cramps, nausea |
Over-the-counter colonoscopy meds, like Miralax or magnesium citrate, work well but have different side effects. Always follow your doctor’s instructions.
After a colonoscopy, watch how your body reacts. If you have:
Don’t hesitate to reach out to your doctor if you’re unsure about symptoms.
Many patients wonder about the costs of colonoscopy and what their insurance covers. This screening is key for catching colorectal cancer early. Knowing the financial side of colonoscopy is important for patients.
The price of a colonoscopy can change a lot. It depends on where you are, who does it, and if extra steps are taken. On average, it costs between $1,000 and $3,000, sometimes more.
Good news: colonoscopy is usually covered by insurance under the Affordable Care Act. This applies to people 50 and older, or those with a family history of colorectal cancer. But, it might not cover colonoscopy laxatives or other prep meds.
Even if the colonoscopy itself is covered, you might have to pay for pre-colonoscopy medications. This includes laxatives and other prep agents. Their prices can vary, with some available without a prescription and others needing one.
If money is tight, there are help programs out there. Some drug makers offer aid for prep meds, and non-profits can help with screening costs. It’s a good idea to ask your doctor or insurance about these options.
Understanding colonoscopy, including prep and risks, helps patients make smart health choices. We’ve looked at colonoscopy’s details, like the prep process and the types of medication. This knowledge is key for a smooth procedure.
Getting ready for a colonoscopy is very important. The right medicine can make a big difference. Knowing the prep medication options helps patients prepare better and avoid problems.
Being well-informed about colonoscopy is essential for a good experience. By knowing the important points and considering personal needs, patients can make the best choices. This ensures the best results for their health.
A colonoscopy lets a doctor see inside the whole colon. It’s used to find colorectal cancer, check for symptoms, and remove growths.
Yes, it’s a minimally invasive method. A flexible tube with a camera is inserted through the rectum to see the colon, without surgery.
Good bowel prep is key for a colonoscopy. It makes sure the colon is clean, allowing for clear views and accurate diagnoses.
Many medications are used, like PEG solutions and sodium phosphate. There are also magnesium citrate and bisacodyl tablets or suppositories, available by prescription or over-the-counter.
A split-dose regimen means taking some prep medication the night before and the rest on the day of the procedure. It helps with better prep and patient comfort.
During a colonoscopy, you’ll get sedation. A doctor will insert a colonoscope through the rectum to look at the colon. They might remove polyps or take biopsies.
Risks include bleeding, perforation, and reactions to sedation. But serious problems are rare.
Colonoscopy costs vary. Insurance usually covers it for screening, but you might pay for prep meds.
Yes, patients with diabetes or kidney disease need special prep. Elderly patients also need extra care.
OTC options include Miralax-based products and magnesium citrate. Bisacodyl tablets or suppositories are also available. They work well, but prescription meds might be stronger.
To manage side effects, adjust the laxative dose or type. Stay hydrated and follow diet advice to ease discomfort and improve prep.
After a colonoscopy, you might feel bloated or gassy. These symptoms usually go away fast. You can usually go back to normal activities and diet in a day.
ScienceDirect. Evidence-Based Medical Insight. Retrieved from https://www.sciencedirect.com/science/article/pii/S1042368008000023
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!