
Peripheral Artery Disease (PAD) is a big problem worldwide. It really affects how well people live and their heart health. A shocking fact is that PAD hits about 8.5 million people aged 40 and older in the United States alone.
Knowing the peripheral artery disease stages is key to managing and treating it well. PAD’s severity is divided into clear stages. Each stage has its own signs and what it means for patient care.
Spotting the PAD severity stages lets doctors create plans that fit each person’s needs. This can lead to better results for patients.
It’s important to know about Peripheral Artery Disease (PAD) for early treatment. PAD is a condition where arteries in the legs get narrowed or blocked.
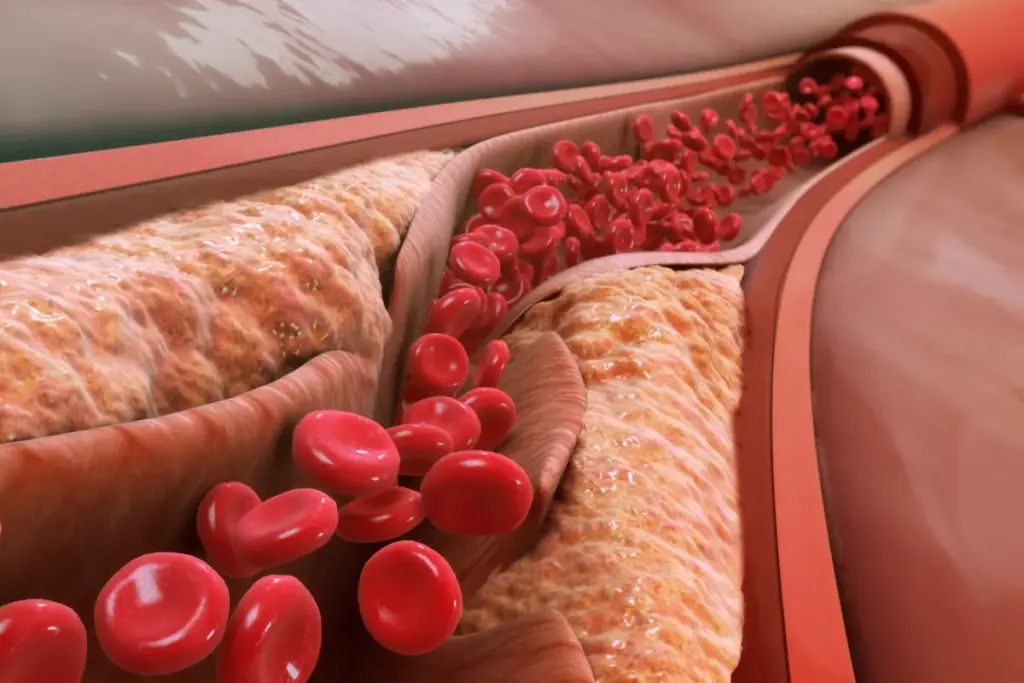
Peripheral Artery Disease (PAD) happens when arteries in the legs get narrowed by atherosclerosis. This reduces blood flow to the limbs. In the United States, about 8.5 million adults aged 40 years and older have PAD. Many cases go unnoticed, making awareness key.
PAD is caused by atherosclerosis narrowing or blocking arteries in the legs. Risk factors include smoking, diabetes, high blood pressure, and high cholesterol. These can lead to intermittent claudication, rest pain, and critical limb ischemia.
Understanding PAD’s effects is vital. It not only affects leg arteries but also the heart. Early treatment is essential to stop the disease from getting worse and to improve health.

It’s important to know the causes and risk factors of PAD. Peripheral Artery Disease is a complex condition. It’s influenced by lifestyle, genetics, and health conditions.
The main cause of PAD is atherosclerosis. This is when plaque builds up in the arteries. It can narrow or block the arteries, reducing blood flow to the limbs.
Atherosclerosis is a key factor in PAD. It’s a progressive condition. It can be influenced by various risk factors.
Risk factors for PAD can be divided into two groups. Non-modifiable factors include age, family history, and genetics. Modifiable factors can be changed through lifestyle or medical interventions.
|
Risk Factor |
Type |
Description |
|---|---|---|
|
Smoking |
Modifiable |
A significant risk factor that can be reduced through cessation |
|
Diabetes |
Modifiable |
Managing diabetes can reduce the risk of PAD |
|
Hypertension |
Modifiable |
Controlling high blood pressure can mitigate PAD risk |
|
Family History |
Non-modifiable |
A history of PAD or cardiovascular disease in the family |
|
Age |
Non-modifiable |
Risk increases with age, after 50 |
A vascular specialist said,
“Managing modifiable risk factors is key to preventing the progression of PAD.”
Knowing these risk factors is vital. It helps in developing prevention and treatment plans.
PAD staging is key in patient care. It helps decide the best treatment and improves health outcomes.
Classifying PAD into stages guides doctors in choosing the right treatment. Accurate staging helps find the best treatments, like lifestyle changes or surgery.
Knowing the PAD stage helps doctors prevent future problems. This proactive approach is vital for managing the disease well.
Staging PAD greatly affects patient results. Effective staging leads to early treatment, slowing disease growth and lowering risk of serious problems.
Also, accurate staging helps educate patients about their care. When patients know their condition and treatment, they follow it better. This leads to better health outcomes.
In conclusion, PAD staging is very important in medical care. It’s essential for managing the disease well, affecting both treatment choices and patient results.
PAD classification systems have grown a lot. They help doctors diagnose and treat PAD better. Staging PAD into different stages is key. It helps decide treatment and predict how well a patient will do.
Many PAD classification systems have been created over time. At first, they just looked for the disease’s presence. But as we learned more about PAD, these systems got more detailed and useful.
Early systems were simple, just saying if someone had symptoms or not. But as we understood PAD better, more complex systems were made.
Key Developments in PAD Classification:
Each system has its own good points and weak spots. The Fontaine and Rutherford systems are the most used. They each have their own way of staging PAD.
|
Classification System |
Key Features |
Clinical Utility |
|---|---|---|
|
Fontaine Classification |
Stages PAD based on symptoms, from none to severe. |
Easy to use in everyday practice. |
|
Rutherford Classification |
Includes more stages and uses tests too. |
More detailed, great for research and tough cases. |
Choosing the right system can really affect treatment and results. It’s important to know about each system and when to use them for good PAD care.
Understanding Peripheral Artery Disease (PAD) is easier with the Fontaine system. It stages the disease based on how bad the symptoms are.
The Fontaine system has been around for a long time. It helps doctors understand PAD by its symptoms. This system breaks PAD into clear stages, helping doctors treat it better.
Stage I means PAD without symptoms. It’s hard to find without tests. It’s important to catch it early to stop it from getting worse.
Stage II is when you feel pain in your legs when you walk. This pain goes away when you rest. It’s split into IIa and IIb based on how far you can walk before feeling pain.
|
Stage |
Symptoms |
Clinical Presentation |
|---|---|---|
|
IIa |
Claudication at a distance >200 meters |
Patients can walk more than 200 meters before experiencing pain. |
|
IIb |
Claudication at a distance ≤200 meters |
Patients experience pain within 200 meters of walking. |
Stage III is when PAD gets really bad. You feel pain in your legs even when you’re not moving. This shows your arteries are badly blocked.
The Fontaine system makes it clear how bad PAD is. It helps doctors figure out what to do next. By dividing the disease into stages, doctors can take better care of their patients.
The Rutherford classification system helps doctors understand how serious Peripheral Artery Disease (PAD) is. It makes diagnosing and treating PAD easier. This system is key in vascular medicine.
The Rutherford classification was made to clearly show how bad PAD is. It helps doctors decide on treatments and standardizes PAD reporting in studies. It has been tested to make sure it works well.
Category 0 is for people who don’t have any PAD symptoms. Even without symptoms, they might have PAD that tests can find.
Categories 1 to 3 are for people with intermittent claudication. This is when legs hurt during exercise because of bad blood flow. The pain level decides the category, from mild to severe.
Category 4 is for those with pain in their legs even when they’re not moving. This shows PAD is very serious and needs quick medical help.
The Rutherford system is vital for doctors to know how bad PAD is. It helps them plan the best treatment for each patient. This way, patients get better care.
Stage1 PAD is tricky to spot because it doesn’t show symptoms. Yet, finding it early is key to stopping it from getting worse.
Doctors often find Stage1 PAD by accident when checking for other health issues. Tests like the ankle-brachial index (ABI) help find PAD without symptoms.
Diagnostic Approaches:
Managing Stage1 PAD means making lifestyle changes and controlling risk factors. This helps stop the disease from getting worse.
Lifestyle Changes:
|
Management Strategy |
Description |
Benefits |
|---|---|---|
|
Smoking Cessation |
Quitting smoking to reduce cardiovascular risks |
Reduces PAD progression, lowers cardiovascular risk |
|
Regular Exercise |
Engaging in regular physical activity |
Improves circulation, enhances overall cardiovascular health |
|
Healthy Diet |
Adopting a diet rich in fruits, vegetables, and whole grains |
Helps manage cholesterol and blood pressure, supports overall health |
Intermittent claudication is a key sign of Stage 2 PAD. It needs quick medical check-ups to stop the disease from getting worse. This condition makes the legs hurt or feel tired when walking or doing other activities. Resting makes the pain go away.
The main sign of Stage 2 PAD is intermittent claudication. It causes pain, cramping, or tiredness in the legs. This happens when you’re active and goes away when you rest.
Key characteristics of intermittent claudication include:
To diagnose Stage 2 PAD, doctors use a mix of clinical checks, patient history, and non-invasive tests. They look for intermittent claudication and how it affects the patient’s daily activities.
|
Diagnostic Method |
Description |
Relevance to Stage 2 PAD |
|---|---|---|
|
Ankle-Brachial Index (ABI) |
A non-invasive test comparing blood pressure at the ankle with that in the arm. |
ABI values help confirm the presence and severity of PAD. |
|
Treadmill Testing |
A test that measures the distance a patient can walk on a treadmill before experiencing claudication. |
Assesses functional limitation due to claudication. |
Managing Stage 2 PAD requires a variety of treatments. These aim to ease symptoms, improve function, and slow disease growth. Treatments include lifestyle changes, medicines, and exercise.
Supervised exercise therapy is key for managing intermittent claudication. It’s a walking program designed for each patient’s needs and abilities.
Each treatment plan is made just for the patient. It considers their health, PAD severity, and symptoms.
Ischemic rest pain is a serious sign of Stage3 Peripheral Artery Disease (PAD). It means blood flow to the limbs is so low that pain happens even when you’re not moving.
Ischemic rest pain in Stage3 PAD comes from blocked or narrowed arteries. This blocks blood flow to tissues. As a result, tissues don’t get enough oxygen or nutrients, even when you’re not active.
Key factors contributing to rest pain include:
People with Stage3 PAD feel pain in their limbs when they’re not moving. This pain gets worse when the limb is raised. It usually hurts the toes or forefoot.
Doctors check for this by doing a detailed exam. They look at:
|
Assessment Method |
Description |
|---|---|
|
Ankle-Brachial Index (ABI) |
Measures the ratio of blood pressure at the ankle to that in the upper arm |
|
Doppler Ultrasound |
Evaluates blood flow and detects stenosis or occlusions |
|
Angiography |
Provides detailed images of the arterial anatomy |
Managing Stage3 PAD aims to ease symptoms and improve life quality. It also tries to stop the disease from getting worse. Treatment plans include:
Pharmacological Interventions: Using medicines to help with pain and improve blood flow.
Revascularization Procedures: These are surgeries or less invasive methods to get blood flowing again.
Good wound care and pain management are key. They help improve patient outcomes and lower the risk of serious problems.
Stage 4 Peripheral Artery Disease (PAD) is the most severe form. It causes tissue loss and critical limb ischemia. This stage greatly affects a patient’s quality of life, needing quick and effective treatments.
Critical limb ischemia (CLI) means the limbs don’t get enough blood. This leads to severe pain, tissue loss, and could result in losing a limb if not treated quickly. It’s a key sign of Stage 4 PAD and needs urgent medical help to stop getting worse.
Key characteristics of CLI include:
In Stage 4 PAD, tissue loss can show up as ulcers or gangrene. This raises the risk of amputation if not treated right. Signs include:
|
Manifestation |
Description |
|---|---|
|
Ulcers |
Open sores that can be painful and hard to heal |
|
Gangrene |
Tissue death due to lack of blood, might need amputation |
It’s important to spot and treat these signs early to avoid more problems.
“Prompt intervention is critical in managing Stage 4 PAD, as delays can result in significant morbidity and mortality.” –
A leading vascular specialist
For Stage 4 PAD, urgent actions aim to improve blood flow, manage pain, and stop more tissue loss. Treatments might include:
Managing Stage 4 PAD well needs a team effort. Vascular specialists, wound care experts, and other healthcare pros work together for the best results.
Accurate diagnosis of Peripheral Artery Disease (PAD) is key for effective treatment. Several methods are used to stage PAD, each with its own strengths and weaknesses.
Non-invasive tests are often the first step in diagnosing PAD. These include:
When non-invasive tests are not clear or more detailed info is needed, invasive procedures are used.
These invasive tests give detailed info needed for treatment planning.
Managing Peripheral Artery Disease (PAD) needs a full plan for each stage. This plan includes medicines and big lifestyle changes. These steps help control symptoms and slow the disease.
Medicine is key in treating PAD. Antiplatelet therapy helps lower heart risks. Doctors often give aspirin and clopidogrel for this.
Statins are used to keep cholesterol in check. This also lowers heart risks. Cilostazol helps with walking and improves life quality for patients.
Changing your lifestyle is vital in managing PAD. Quitting smoking is very important. Smoking makes PAD worse.
Regular exercise, like walking, is also key. It helps symptoms and heart health. Eating right is another big part of treatment. A heart-healthy diet is recommended.
Managing diabetes and hypertension is also important. This can be done with lifestyle changes and medicines.
Combining medicines with lifestyle changes gives a full plan for PAD. This plan helps manage the disease at all stages.
Endovascular and surgical interventions are key in treating PAD. The choice of treatment depends on the disease stage. As PAD gets worse, treatments become more complex and severe.
Angioplasty and stenting are common treatments for PAD. Angioplasty uses a balloon to widen narrowed arteries. Stenting places a metal tube to keep arteries open. These methods work well for those with claudication or at risk of limb ischemia.
“Drug-coated balloons and stents have changed endovascular treatments,” says a top vascular surgeon. “They lower restenosis risk and improve long-term results.”
Bypass surgery creates a detour around blocked or narrowed arteries. A graft is used, which can be from another part of the body or synthetic. It’s often chosen for severe PAD or when endovascular treatments fail.
New techniques in PAD treatment are emerging. Atherectomy devices remove plaque, and drug-coated balloons reduce restenosis risk.
A study found, “New endovascular technologies have greatly improved PAD treatment outcomes. They offer hope for those with advanced disease.”
The future of PAD treatment will combine these new methods. Tailored to each patient’s needs, research will lead to more effective, less invasive treatments.
Managing PAD is not a one-size-fits-all approach. It needs tailored plans for different patient groups. Diabetic patients and those with heart disease need special care because of their unique health needs.
Diabetic patients with PAD face a big challenge. Diabetes greatly increases the risk of PAD. This condition also raises the risk of heart problems and losing a limb.
Patients with PAD often have heart disease too. This makes managing their condition more complex. Heart disease raises the risk of bad outcomes for PAD patients.
|
Clinical Aspect |
PAD in Diabetic Patients |
PAD with Concurrent Cardiovascular Disease |
|---|---|---|
|
Primary Risk |
Limb loss, cardiovascular events |
Cardiovascular events, mortality |
|
Management Focus |
Glycemic control, limb preservation |
Risk factor modification, cardiovascular risk reduction |
|
Key Interventions |
Regular screening, multidisciplinary care |
Antiplatelet therapy, risk factor modification |
Understanding the special needs of PAD patients, including diabetics and those with heart disease, helps doctors create better treatment plans. This personalized approach improves patient outcomes and lowers the risk of complications.
PAD prevention is about using many strategies to slow the disease. It includes both primary and secondary prevention. Early detection and prevention are vital for managing Peripheral Artery Disease and improving patient outcomes.
Primary prevention aims to lower PAD risk factors. It involves lifestyle changes like quitting smoking and eating healthy. Smoking cessation is very important because smoking greatly increases PAD risk.
Eating a diet full of fruits, vegetables, and whole grains helps manage cholesterol and blood pressure. These are risk factors for PAD. Regular walking improves circulation and heart health.
For those with PAD, secondary prevention is key to slow the disease and manage symptoms. This includes pharmacological interventions to control high blood pressure and cholesterol.
Supervised exercise therapy programs can also help. They improve walking distances and quality of life for PAD patients. Regular check-ups with healthcare providers are important to adjust treatment plans.
Screening for PAD includes checking risk factors and doing ankle-brachial index (ABI) tests. Early detection through screening leads to timely interventions and better outcomes.
Peripheral Artery Disease (PAD) is a complex condition that needs a deep understanding to manage well. The four stages of PAD show how important early detection and treatment are.
A pad summary of the stages shows early detection can greatly improve patient results. By knowing the symptoms and clinical signs at each stage, doctors can create treatment plans that fit each patient’s needs. This helps lower the risk of the disease getting worse.
In conclusion, knowing the four stages of PAD is key to managing it effectively. This knowledge helps doctors create specific treatment plans. It improves patient outcomes and quality of life. As a pad conclusion, awareness and education on PAD stages are essential for both doctors and patients.
PAD is divided into four stages. These are based on the Fontaine or Rutherford systems. They range from no symptoms to severe limb ischemia.
PAD is a condition where blood vessels outside the heart narrow or block. This reduces blood flow to the limbs.
Atherosclerosis, or plaque buildup, is the main cause of PAD. Risk factors include smoking, diabetes, high blood pressure, and high cholesterol.
PAD is staged to show how severe it is. This helps doctors decide on treatment and predict outcomes.
The Fontaine system stages PAD into four levels. These include no symptoms, intermittent pain, rest pain, and gangrene or ulcers.
The Rutherford system categorizes PAD into seven levels. It’s based on symptoms and how severe they are.
Stage1 PAD is managed by changing lifestyle and reducing risk factors. Monitoring is also key to prevent it from getting worse.
Stage2 PAD causes pain in the legs during exercise. This pain goes away when you rest.
Stage3 PAD causes pain in the legs even when you’re not moving. This is a sign of severe limb ischemia.
Stage4 PAD is when you have critical limb ischemia. This means you have tissue loss or gangrene, needing urgent care to avoid amputation.
PAD is diagnosed with non-invasive tests like the ankle-brachial index (ABI) and duplex ultrasound. Angiography is also used.
PAD treatments include medicine and lifestyle changes. More severe cases may need angioplasty, stenting, or bypass surgery.
Preventing PAD involves managing risk factors and making lifestyle changes. This slows down disease progression.
Diabetic patients with PAD need special care. Their risk factors are higher, so aggressive treatment and monitoring are necessary.
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4622220/
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!