
Getting ready for a medical test can make you nervous, and wondering about the pain is normal. Men thinking about a cystoscopy often ask, does a cystoscopy hurt? It’s a common concern.
A cystoscopy lets a doctor check the bladder and urethra’s lining. They use a cystoscope through the urethra and into the bladder. Most men say they feel some pain, but it’s generally mild and brief.
We’ll look into how much pain you might feel, what to expect during the procedure, and tips to reduce discomfort. With the right preparation, a cystoscopy can be a manageable experience.
Key Takeaways
- Cystoscopy is a common procedure for examining the bladder and urethra.
- Men’s experiences with pain during cystoscopy can vary.
- Most men report moderate discomfort during the procedure.
- Understanding what to expect can help reduce anxiety.
- There are ways to minimize discomfort during and after cystoscopy.
What Happens During a Male Cystoscopy Procedure
A male cystoscopy is a simple procedure. It lets doctors see inside the bladder and urethra. This is key for finding urological problems. We’ll explain the steps, including the types of cystoscopes used.
Definition and Purpose of Cystoscopy
Cystoscopy involves using a thin tube with a camera and light. It’s inserted into the urethra to look at the bladder and urethra. The main goal is to find and sometimes treat problems in the lower urinary tract.
Doctors can see inside the urinary tract. This helps them spot issues like stones, tumors, or inflammation.
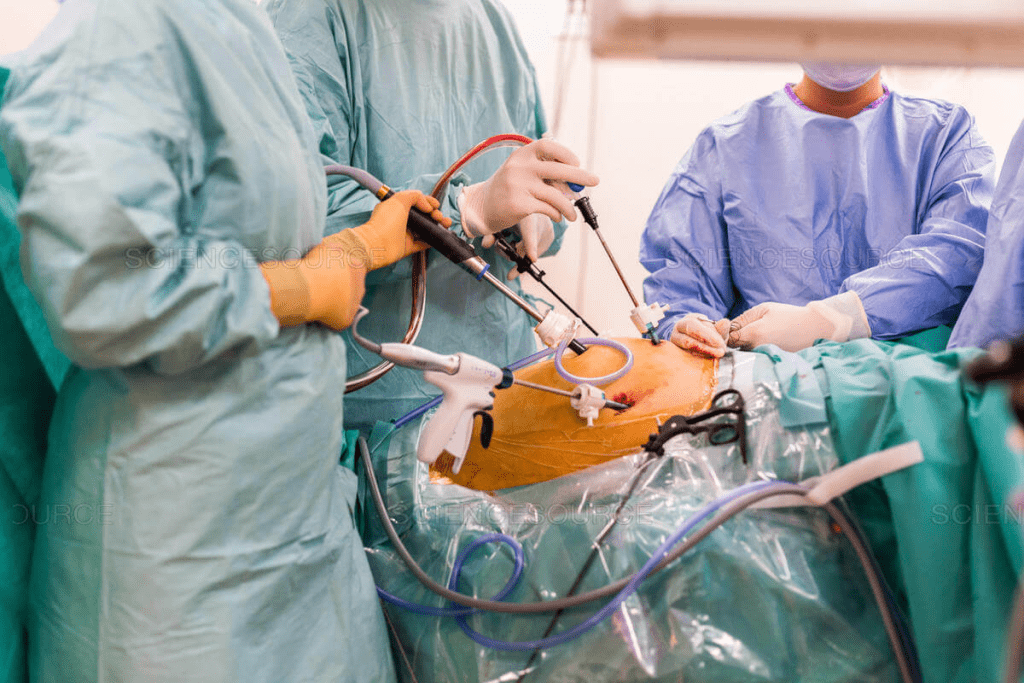
Step-by-Step Procedure Walkthrough
The patient lies on an examination table, with legs up. The genital area is cleaned with an antiseptic. Local anesthesia or sedation might be used to reduce pain.
The cystoscope is then inserted into the urethra and moved into the bladder. Saline solution is used to fill the bladder, making it easier to see. The doctor looks for any problems in the bladder walls and urethra.
The whole process usually takes 5 to 15 minutes. This time can vary based on how detailed the examination needs to be.
Flexible vs. Rigid Cystoscopy Instruments
Cystoscopy can be done with either a flexible or rigid cystoscope. Flexible cystoscopy uses a thin, bendable tube. It’s more comfortable for some patients and is often used for checking things out.
Rigid cystoscopy uses a straight, rigid tube. It’s used for more detailed exams or when more procedures are needed. The choice depends on the situation and the patient’s health.
Knowing the difference between these tools helps patients prepare. They can understand what to expect. Each type can cause different levels of discomfort, which we’ll look at next.
Does a Cystoscopy Hurt? The Truth About Pain Levels
Men preparing for cystoscopy often wonder about the pain level. We’ll look at recent studies on pain during cystoscopy. We’ll also talk about the parts of the procedure that might hurt the most.
Median Pain Scores for Men
Studies show that men’s pain during flexible cystoscopy averages 2.82 on a 0-10 scale. This means most men feel mild to moderate pain. One study participant said,
“The procedure was uncomfortable, but the pain was manageable.”
Many studies agree, showing that pain can vary greatly from person to person.
image is to be replaced’
The Most Painful Moment: Passing the Membranous Urethra
The most painful part is when the scope goes through the membranous urethra. This area is very sensitive, causing distress for some. But remember, this pain is usually short-lived, and there are ways to lessen it.
Percentage of Men Reporting Significant Pain
While the average pain score gives a general idea, it’s also key to know how many men feel a lot of pain. About 5.7% of men say their pain is over 5 on the 0-10 scale. This shows that pain can vary a lot and highlights the importance of tailored care during cystoscopy.
Anxiety and past experiences can also affect how much pain you feel. Talking about these with your doctor can help you prepare and might make the procedure less painful.
5 Factors That Affect Cystoscopy Pain in Men
Knowing what affects cystoscopy pain can help men get ready for it. Different things can make the pain level vary from person to person.
Male Urethral Anatomy Considerations
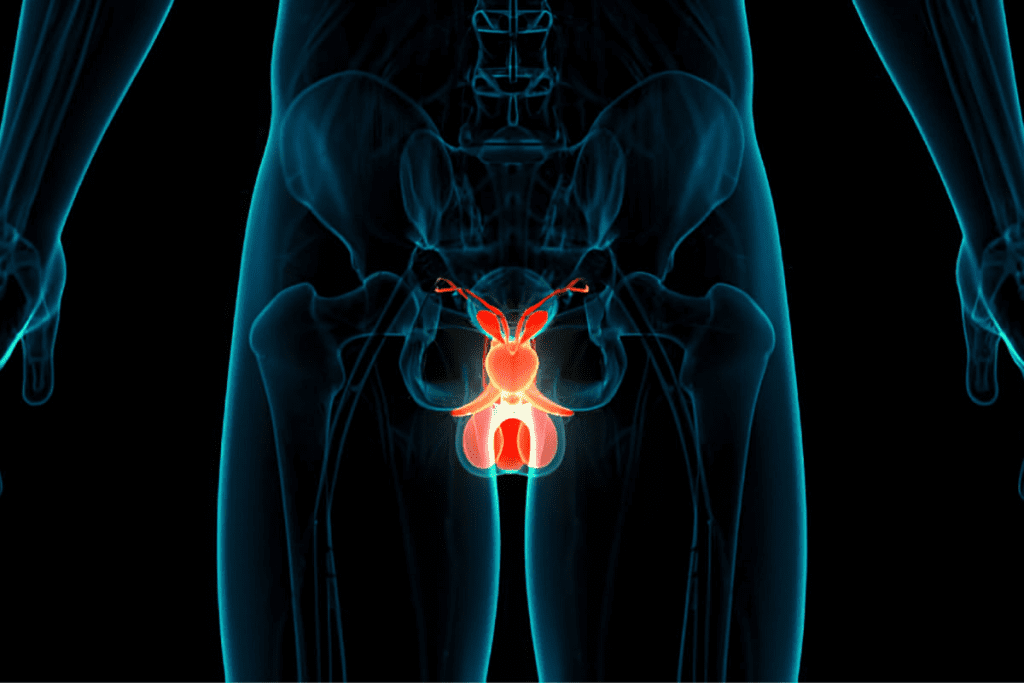
The shape and size of the male urethra matter a lot for cystoscopy pain. The urethra’s length, shape, and any narrow spots can make it harder to insert and move the cystoscope. Men with urethral strictures or an enlarged prostate may feel more pain because it’s harder to pass the cystoscope.
image is to be replaced’
Anxiety and Its Impact on Pain Perception
Anxiety also plays a big role in how much pain a man feels during cystoscopy. Men who are more worried about the procedure might feel more pain because they are more tense. Talking to the patient and making them feel comfortable can help lower their anxiety and possibly reduce pain.
Previous Urological Experiences
What a man has gone through before can also change how he feels pain during cystoscopy. Men who have had cystoscopies or other urethral procedures before might have different pain expectations. Bad experiences in the past can make a man more anxious and feel more pain.
Age and Prostate Size
Age and prostate size are also important for cystoscopy pain. Older men or those with a bigger prostate might have a different urethra that can make the procedure less comfortable. We think about these things when we plan to make the procedure as painless as possible.
By knowing these factors, we can make the cystoscopy experience better for each patient. This way, we can ensure it’s as comfortable as possible for them.
Flexible vs. Rigid Cystoscopy: Pain Comparison
Choosing between flexible and rigid cystoscopy is important because it affects how much pain you might feel. Patients worry about the discomfort of cystoscopy. The type of cystoscope used is a big factor in this.
Flexible cystoscopy is usually less painful than rigid cystoscopy. Flexible cystoscopy has a pain level of 2.5 ±1.4. Rigid cystoscopy has a pain level of 3.4 ±1.6. This shows that flexible cystoscopy is generally more comfortable.
Pain Levels: Flexible Cystoscopy
Flexible cystoscopy is often chosen for its lower discomfort. The flexible cystoscope moves more naturally through the urethra. This reduces irritation and discomfort. Patients usually report lower pain scores, making it a more comfortable option.
Pain Levels: Rigid Cystoscopy
Rigid cystoscopy is more uncomfortable but sometimes needed for certain procedures. It requires the rigidity of the instrument for therapeutic interventions. The higher pain levels of rigid cystoscopy (3.4 ±1.6) are a consideration. But, most patients can tolerate it.
Clinical Situations Requiring Each Type
The choice between flexible and rigid cystoscopy depends on several factors. These include the purpose of the procedure and the patient’s condition. For example:
- Flexible Cystoscopy: Ideal for diagnostic purposes, such as examining the bladder lining or collecting biopsy samples.
- Rigid Cystoscopy: Often used for therapeutic interventions, like removing bladder stones or tumors.
Understanding these differences helps patients prepare for their cystoscopy procedure. They know what to expect based on the type of cystoscopy they are scheduled for.
In conclusion, both flexible and rigid cystoscopy have their roles in urological diagnostics and treatment. The pain levels differ between the two. By choosing the right type of cystoscopy for the clinical situation, healthcare providers can reduce patient discomfort.
7 Effective Ways to Reduce Cystoscopy Discomfort
Cystoscopy is important for men’s health but can be uncomfortable. We’re here to help you find ways to feel better. There are many strategies to lessen the pain of cystoscopy.
Pre-procedure Preparation Techniques
Getting ready before the procedure can make a big difference. Relaxation techniques like meditation or deep breathing can calm you down. Talking to your healthcare provider about your anxiety can also help.
Voiding During Insertion
Voiding during the insertion of the cystoscope can help reduce pain. Studies show it can lower pain scores from 5.16 to 3.06. This makes a big difference in how you feel.
Topical Anesthetics and Lubricants
Topical anesthetics and lubricants are key to lessening discomfort. They numb the area and reduce friction. This makes the cystoscope insertion less painful. Lidocaine gel and other numbing agents are common choices.
Breathing and Relaxation Techniques
Breathing and relaxation techniques can also be very helpful. Methods like progressive muscle relaxation, visualization, or guided imagery can distract you from pain. They help you relax.
To make cystoscopy more comfortable, try these tips:
- Arrive early to the appointment to complete any necessary paperwork and get settled before the procedure.
- Communicate openly with your healthcare provider about your anxiety or any concerns you may have.
- Use the relaxation techniques you’ve practiced beforehand to help you stay calm.
By using these strategies, you can greatly reduce cystoscopy discomfort. While some discomfort is normal, there are many ways to make it less. This makes the procedure more bearable.
Conclusion: Managing Expectations for Your Cystoscopy
Knowing what to expect during a cystoscopy can make a big difference. It helps men feel better during the procedure. Understanding how pain works, like how the urethra is different in men, can help prepare you.
It’s key to follow the latest medical advice to feel more comfortable. Things like getting ready before the procedure, taking breaks to pee, and using special creams can help. These steps can make the process less painful.
Healthcare teams should focus on making patients the center of care. Using the newest medical guidelines helps a lot. This way, patients get the best care and feel less pain, making the whole experience better.
FAQ
Does a cystoscopy hurt?
Some discomfort is common, but pain levels vary. Men’s median pain score is about 2.82 on a 0-10 scale.
Is a cystoscopy painful for males?
Pain levels during cystoscopy vary. Anxiety, past urological experiences, and cystoscope type affect how much pain you feel.
How painful is a cystoscopy for men?
The most painful part is when the cystoscope goes through the membranous urethra. But, with the right prep and relaxation, you can feel less discomfort.
What type of cystoscopy is less painful?
Flexible cystoscopy is less painful than rigid. It has a mean pain score of 2.5 ±1.4, compared to 3.4 ±1.6 for rigid.
How can I reduce discomfort during cystoscopy?
To feel less discomfort, try pre-procedure prep, voiding during insertion, and using anesthetics and lubricants. Also, use breathing and relaxation techniques.
Are there any specific preparations I should make before undergoing a cystoscopy?
Yes, to reduce discomfort, arrive relaxed, use topical anesthetics, and follow pre-procedure instructions.
Can anxiety affect the level of pain experienced during cystoscopy?
Yes, anxiety can make pain worse. Knowing this and using relaxation techniques can help manage anxiety and discomfort.
What is the difference between flexible and rigid cystoscopy?
Flexible cystoscopy uses a flexible tube with a camera. Rigid cystoscopy uses a rigid tube. The choice depends on the situation and patient needs.
References
Taghizadeh, A. K., Hassan, M., Jequier, S., & Muneer, A. (2006). When does it hurt? Pain during flexible cystoscopy in men. Urologia Internationalis, 76(4), 328-331. PubMed








