
Many people deal with kidney stones that can block the ureter. This causes a lot of pain and can lead to serious problems. A ureteral stent is often used to solve this issue. Explaining the role of a ureteral stent in urine flow and the process of removal of ureteric stent after a procedure.
A ureteral stent is a thin tube that goes into the ureter. It helps urine flow from the kidney. This is key for those with a kidney stone in the ureter. It keeps the stone from blocking the flow and causing infection or kidney damage.
Knowing how a stent works can help patients manage their condition better. It helps them make informed choices about their treatment.
Kidney stones can cause a lot of pain when they block the ureters. These are the tubes that carry urine from the kidneys to the bladder. The urinary system, which includes the kidneys, ureters, and bladder, is key for filtering waste and making urine.
The kidneys make urine, which then goes through the ureters to the bladder. The ureters use muscle contractions to push urine towards the bladder. This is important for keeping urine flowing and preventing infections.
Kidney stones form when minerals in urine crystallize and stick together. These stones can move from the kidneys into the ureters, causing a blockage. This blockage is called a ureter blockage kidney stone. The movement of stones can be very painful and may cause serious problems if not treated.
When kidney stones in the ureter happen, they can cause a lot of pain, nausea, and vomiting. If the stone is big enough, it can block urine flow. This can lead to high pressure and damage to the kidney. It’s important to understand how the kidneys, ureters, and bladder work together to manage kidney stones.
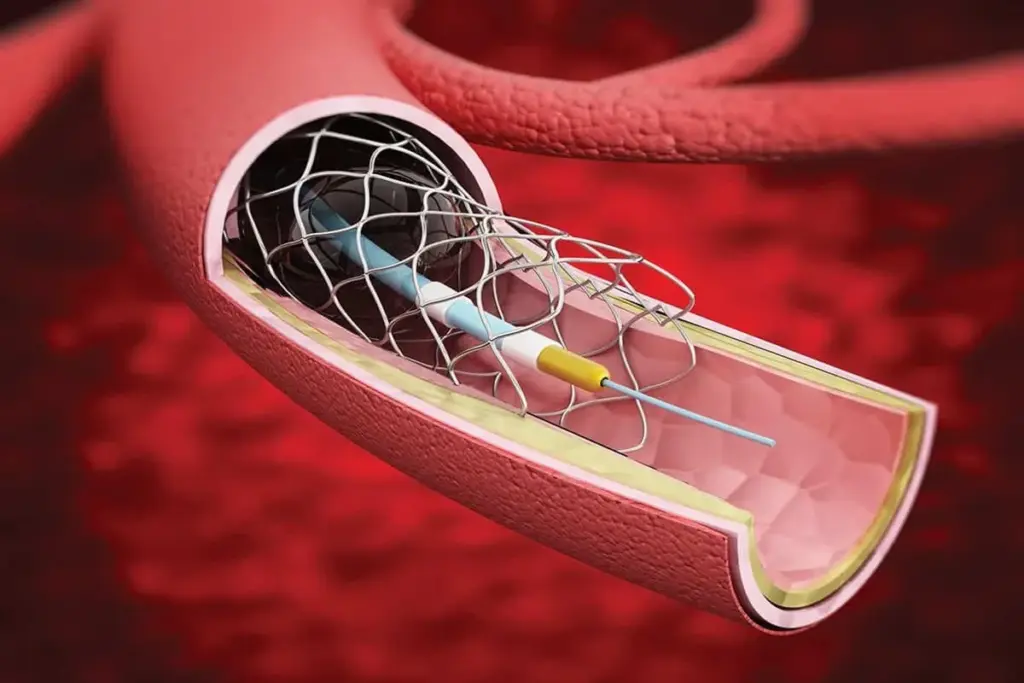
A ureteric stent is a soft, flexible tube that helps urine flow from the kidney to the bladder. It’s very important for people with ureteral obstructions, like those caused by kidney stones.
A ureteral stent is a thin, hollow tube made of materials that are safe for the body. Its main job is to keep the ureter open for urine to flow properly. The stent has a few key parts:
There are many types of ureteric stents, but the Double J stent is very common. It has a unique “J” shape at both ends to keep it in place. Other types include:
How long a ureteral stent stays in can vary. It depends on the patient’s situation and why the stent was put in. Usually, stents are taken out after a few days to weeks. But sometimes, they might stay longer.
Kidney stones can block the ureter, causing severe pain. A ureteric stent is often used to fix this. It helps urine flow normally again.
A ureteric stent relieves the blockage caused by kidney stones. It reduces the pressure behind the stone. This helps lessen the pain and discomfort.
Effective ureteral obstruction treatment means placing the stent right. It lets urine go around the blockage.
Stents also help kidney stones pass. They don’t push the stone out but keep the ureter open. This makes it easier for the stone to move.
This is very helpful in treatment for blocked ureter cases. When the stone blocks a lot.
After some treatments for kidney stones, a stent is placed. It helps the ureter heal. It prevents it from narrowing or scarring.
This is key in kidney stone blockage treatment. It helps avoid future problems.
Ureteric stents are a common tool in urology. Doctors say they can stay in for weeks, months, or even years. They keep the ureter open and urine flowing.
|
Function |
Description |
Benefit |
|---|---|---|
|
Relieving Obstruction |
Ensures urine can bypass the blockage |
Reduces pain and discomfort |
|
Facilitating Stone Passage |
Keeps the ureter open for stone movement |
Eases the passage of kidney stones |
|
Supporting the Ureter |
Prevents narrowing or scarring after procedures |
Ensures ureter remains patent and functional |
“The placement of a ureteral stent is a critical step in managing ureteral obstruction caused by kidney stones, allowing for the restoration of normal urinary flow.”
Ureteral stent placement is key for those with kidney stones. It helps clear blockages in the ureter.
A healthcare provider will explain the stent use and ask for your okay before starting. You might need tests and stop some meds.
A cystoscope, a thin tube with a camera, is used to insert the stent. It goes through the urethra. This lets the urologist see the ureter and place the stent right.
You might feel some pain during the procedure, but it’s usually done with sedation or local anesthesia. Afterwards, you might feel some irritation or discomfort. This usually goes away with time.
Knowing what to expect can ease your worries. It makes the ureteral stent placement process easier for patients.
Living with a ureteric stent means making some changes. But with the right info, patients can get through it easier. This stent helps when kidney stones block the flow of urine.
People with a ureteric stent might feel different things. They might feel kidney stent discomfort or bladder stent discomfort. This can feel like pain or pressure in the lower back or belly.
Some might also feel urinary stent discomfort. This can be feeling the need to pee a lot or a burning feeling when they do.
Seeing blood in the urine is common too. It might scare you, but it’s usually okay.
With a ureteric stent, some activities might not be safe. You should avoid heavy lifting, bending, or hard exercises. Knowing what you can and can’t do helps plan your day and avoid pain.
It can be hard to manage bowel movements and urination with a stent. You might need to change your diet to avoid constipation. Drinking lots of water is key to prevent infections and keep the stent working right.
Some people might pee more often or feel like they need to pee right away. Talking to a doctor can help manage these changes.
It’s usually okay to have sex with a ureteric stent, but be careful. Talk to your doctor about any ureteral stent and sex concerns. Knowing about any possible discomfort or problems is important.
Understanding life with a ureteric stent helps. It’s about managing bowel movement with ureteral stents and knowing about possible discomforts. This way, patients can handle their treatment better.
Ureteric stents come with risks. They help manage kidney stones and other urinary issues but can have side effects. It’s important to know these risks.
People with ureteric stents may feel discomfort. This can be mild or severe. They might experience pain in their lower abdomen, back, or bladder.
They might also feel the need to urinate more often or urgently. Some may see blood in their urine.
Ureteric stents can raise the risk of urinary tract infections (UTIs). Bacteria on the stent can cause serious infections. Other serious issues include stent encrustation, migration, or breaking apart.
“The risk of urinary tract infection (UTI) is a significant concern for patients with ureteric stents.”
If you have severe pain, fever, or trouble urinating, get medical help right away. These signs might mean you have a serious problem.
|
Complication |
Description |
|---|---|
|
Stent Encrustation |
Deposits forming on the stent, potentially causing blockage. |
|
Stent Migration |
The stent moves from its original position, potentially causing discomfort or obstruction. |
|
Stent Fragmentation |
The stent breaks into pieces, which can be difficult to remove. |
Knowing about these complications helps patients and doctors make better choices about using ureteric stents.
Learning about the process and preparation for removing a ureteric stent can ease worries. Removing a ureteric stent is a big step for those with kidney stones.
The right time to remove a ureteric stent varies. It depends on why the stent was placed, the stent type, and your health. Usually, stents come out after a few days to weeks. Your doctor will decide when it’s best for you.
There are various ways to remove a ureteric stent. The method chosen depends on the stent type and your situation. Some stents have a string outside your urethra for easy removal.
Some stents have strings for self-removal. But, not all stents can be removed this way. Your doctor will tell you the best way to remove yours.
If you need a doctor to remove your stent, you’ll need to get ready. You might need to arrive with a full bladder. Your doctor will give you specific instructions.
It’s key to follow your doctor’s advice for a smooth stent removal. If you have questions or concerns, ask your healthcare team.
Knowing what to expect during stent removal can ease your worries and discomfort. This procedure usually happens in a urologist’s office or clinic.
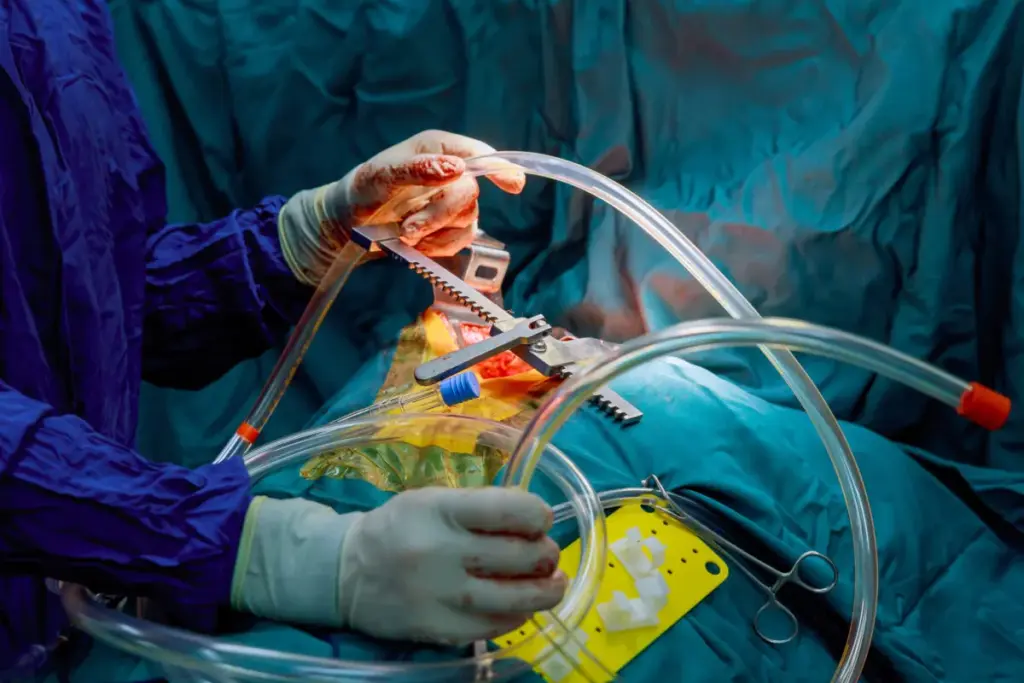
Your urologist will first numb the area with a topical anesthetic. They use a cystoscope, a thin, flexible tube with a camera, to find the stent. This tube goes through the urethra.
Once the stent is found, it’s carefully pulled out. This whole process is quick, usually taking just a few minutes.
The procedure is similar for both men and women, but there are differences. Men need a longer cystoscope because their urethra is longer. Women might feel a different sensation because of their shorter urethra.
Managing pain during stent removal is key. The topical anesthetic helps reduce discomfort. Some people might feel a bit of pain or urgency after, but it goes away fast.
Your urologist will give you tips on handling any pain after the procedure. Overall, removing a ureteric stent is a simple process that most people find okay. Knowing what to expect can help you prepare better.
Knowing what to expect after a ureteric stent removal can make recovery easier. Removing the stent is a key part of treating kidney stones or ureteral blockages.
Right after the procedure, you might feel drowsy from the anesthesia. You could feel some pain or relief as the stent is removed. It’s important to follow your doctor’s instructions for care after removal to avoid problems.
How long it takes for your urine to feel normal can vary. Usually, people start to feel better within a few days. But, some might feel mild discomfort or need to urinate more often for a bit.
Though rare, problems can happen after the stent is removed. These might include infection, bleeding, or urinary tract issues. Watching your symptoms and knowing when to see a doctor is key.
If you have severe pain, fever, or trouble urinating after the stent is removed, call your doctor right away. These signs could mean you need urgent medical help.
Understanding the recovery and watching out for complications can help you get through the post-stent removal period more smoothly and confidently.
There are new hopes for patients with ureteral obstruction. Ureteral stenting is a common, but not the only, solution. It’s a minimally invasive surgery.
Medication is key for those with kidney stones causing ureteral obstruction. Alpha-blockers help relax the ureter muscles, making it easier for stones to pass. Pain meds also help reduce discomfort.
Sometimes, surgery is needed for ureteral obstruction. Ureteroscopy with laser lithotripsy is a method where a small scope finds the stone. A laser breaks it into smaller pieces for easier passage. Percutaneous nephrolithotomy is used for bigger stones, a more invasive approach.
Urology is always improving, with new treatments for ureteral obstruction. Biodegradable stents are a big step, as they don’t need to be removed. Other new tech includes better lithotripsy and more precise diagnostic tools.
Knowing about these options helps both patients and doctors make better choices for ureteral obstruction treatment.
Understanding kidney stone stents is key for those with ureteral blockages. A ureteral stent is a small tube that helps urine flow from the kidney to the bladder.
Choosing the right treatment for kidney stones, like stents, needs a full understanding of the options. Knowing how stents work and their possible side effects helps patients make better choices.
Talking to doctors is vital to find the best treatment for kidney stones. They can tell if a stent is needed and how it fits into the treatment plan.
Being well-informed and active helps people make choices that fit their needs. This leads to better kidney stone management and overall health.
A ureteric stent is a thin, flexible tube. It’s put into the ureter to help urine flow from the kidney to the bladder.
The main goal of a ureteric stent is to ease blockages and pressure from kidney stones. It helps stones pass and supports the ureter after procedures.
The time a ureteral stent stays in varies. It depends on the case and the stent type. Usually, it’s a few days to weeks.
Having a ureteric stent can cause urinary frequency, urgency, and pain in the bladder or kidney area.
Removing a ureteric stent is simple. It’s often done with a cystoscope. Sometimes, a string-based method is used.
Removing a ureteric stent is usually painless. But, some might feel mild discomfort or urgency.
Complications include infection, stent migration, and irritation or damage to the ureter or bladder.
It’s best to avoid sex with a stent. Or, take precautions to prevent discomfort or complications.
Alternatives include medications, surgical options like lithotripsy or ureteroscopy, and new technologies.
Recovery time varies. But, most people can get back to normal urination in a few days.
You’ll undergo a cystoscopy. The stent is inserted through the bladder into the ureter.
A ureteric stent doesn’t directly affect bowel movements. But, some might notice changes or discomfort.
To manage urinary issues, stay hydrated, avoid certain foods, and follow your healthcare provider’s advice.
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/28279314/
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!