Every 40 seconds, someone in the United States has a heart attack. This is often because of a blockage in the coronary artery. If not treated quickly, this can cause permanent damage. Detailing the threshold blockage percentage for stent placement (often 70% or more) and other factors guiding the decision.
Knowing how bad the artery blockage is is key to figuring out the right treatment. This might include using a stent. A stent keeps the artery open, helping blood flow again.
So, how much heart blockage needs a stent? Knowing this is important for both patients and doctors.
It’s important to know about coronary artery disease to understand blockages and their effect on the heart. This disease causes the coronary arteries to narrow or block due to plaque buildup. This can lead to heart attacks.
Blockages in arteries happen over time because of plaque buildup. This plaque is made of fat, cholesterol, and other substances. Factors like high blood pressure, smoking, and high cholesterol can make this happen.
The plaque buildup makes the arteries hard and narrow. This restricts blood flow to the heart. If not treated, it can cause severe blockages. In such cases, stent placement might be needed.
There are different types of coronary blockages:
The severity of a blockage is measured as a percentage of the artery blocked. This is done during a coronary angiogram. A blockage of 70% or more is seen as serious. It might need stent placement based on certain stent placement criteria.

The need for a stent depends on several factors. These include the person’s health and how much the stent will help their life.
Many think a 70 percent blockage means a stent is needed. But, it’s more complex. Doctors look at the blockage’s severity, symptoms, and other health factors.
Moderate blockages, between 40% and 70%, are tricky. Doctors use tests like Fractional Flow Reserve (FFR) or Intravascular Ultrasound (IVUS) to check blood flow.
Key considerations for moderate blockages include:
Severe blockages, over 70%, usually need stents or surgery. A high blockage severely limits blood flow, causing serious symptoms or heart attacks.
For severe blockages, stent placement is often recommended when:
Blockage percentages are very important. While they don’t decide stent use alone, they’re key in the overall assessment.
A cardiology expert says, “The decision to place a stent is multifactorial. It involves not just the percentage of blockage, but also the patient’s clinical presentation and overall cardiovascular risk profile.”
“The percentage of blockage is just one piece of the puzzle; we need to consider the entire clinical picture to make informed decisions about stent placement.”
— Dr. Jane Smith, Cardiologist
It’s vital to understand blockage percentages and their importance. This helps cardiologists and patients make informed decisions about stent placement.
Deciding to use a stent isn’t just about the blockage percentage. Many other medical factors are considered. Doctors look at a range of things when deciding if a stent is needed.
The severity and frequency of symptoms are key in stent decisions. Even with a small blockage, frequent or severe angina might mean a stent is needed. How symptoms affect a patient’s life is also important.
The location and accessibility of the blockage matter a lot. Some blockages, like those in main coronary arteries, might get stented. This is because they could harm heart function. How easy it is to reach the blockage during the procedure also plays a role.
An assessment of overall heart function is essential. Doctors check how well the heart pumps and if all heart muscle gets enough blood. This helps decide if a stent is needed.
Cardiologists use several tests to find out how bad artery blockages are. These tests help decide the best treatment for heart disease.
Coronary angiography is a test to see if heart arteries have blockages. A cardiologist injects dye into the arteries for an X-ray. This shows where and how bad the blockages are.
Intravascular Ultrasound (IVUS) is used to check artery blockages. A small probe is put into the artery to see the walls and plaque. This helps doctors know how bad the blockages are.
Fractional Flow Reserve (FFR) measures pressure across blockages. It checks if a blockage is really blocking blood flow to the heart.
FFR results range from 0 to 1. Values near 1 mean blood flow is normal. Values under 0.8 show a blockage is severe and needs treatment.
These tests are key to understanding how bad artery blockages are. By using them together, doctors can choose the best treatment for each patient.
Knowing the warning signs of severe artery blockage can save lives. A blockage shows through clear symptoms that need quick medical care. These signs include chest pain, shortness of breath, and other indicators.
Chest pain, or angina, is a key sign of artery blockage. It happens when the heart doesn’t get enough oxygen. This pain feels like pressure or squeezing in the chest and can spread to the arms, back, neck, jaw, or stomach. It’s important to recognize angina patterns to spot artery blockage.
Feeling short of breath when you’re active is another sign of artery blockage. This happens when the heart can’t pump enough blood. It’s a serious symptom, even if it happens with little effort.
Other signs include feeling tired, dizzy, or having irregular heartbeats. In the worst cases, a heart attack can happen. It brings intense chest pain, nausea, and cold sweats. Seeking medical help right away is vital if you notice these signs.
Knowing these symptoms helps people get medical help early. This can prevent serious problems.
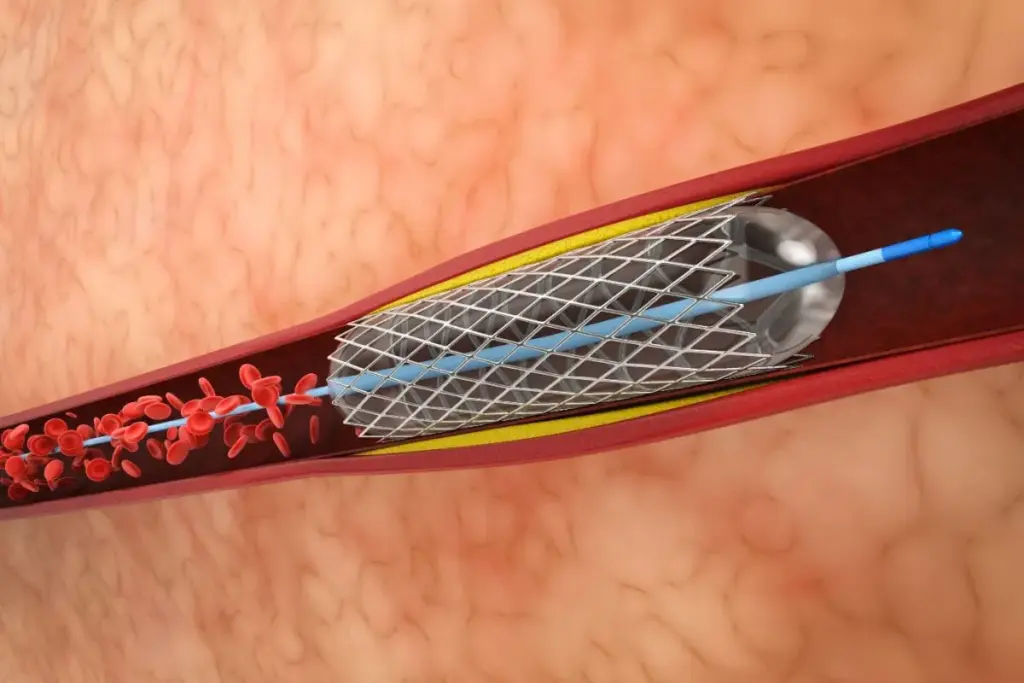
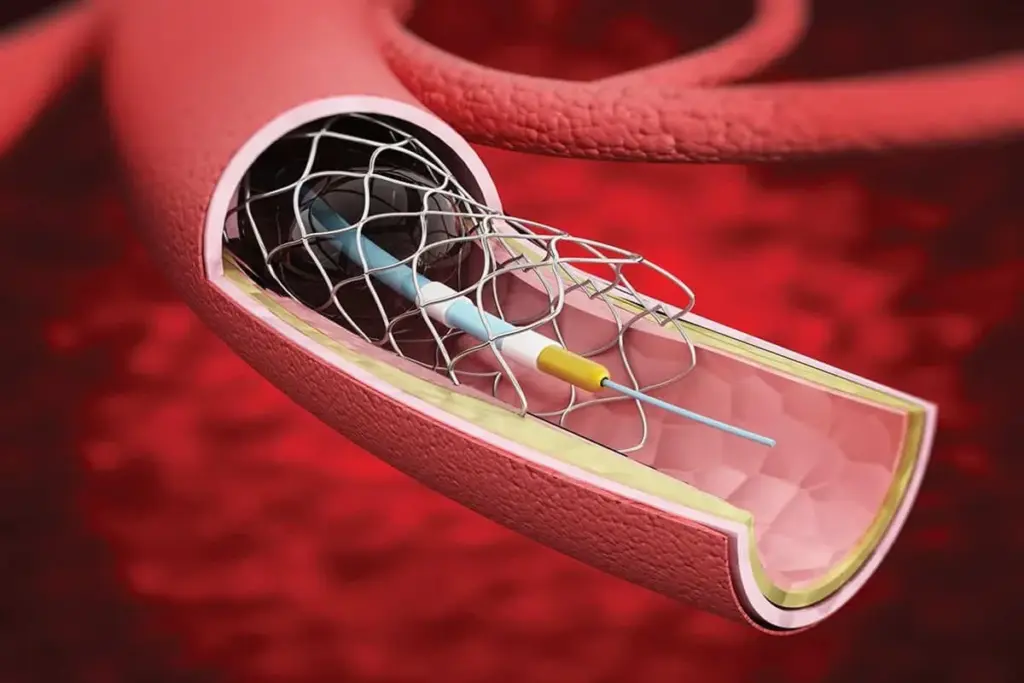
Choosing the right stent is key when treating blocked arteries. Stents are tiny, mesh-like tubes that open up narrowed or blocked arteries. This helps blood flow to the heart. There are many types of stents, each for different needs and conditions.
Bare metal stents are made from metal and were the first used in angioplasty. They support the artery but don’t release medication.
Drug-eluting stents have a coating that slowly releases medicine. This greatly lowers the chance of the artery narrowing again. They’re best for those at high risk of this happening.
Bioresorbable vascular scaffolds are a newer option. They dissolve over time, which might reduce long-term problems. They help support the artery walls as they heal.
Choosing a stent depends on many things. These include the blockage’s location and severity, the patient’s health, and past stent use. Here’s a comparison of the different stent types:
|
Stent Type |
Key Features |
Typical Applications |
|---|---|---|
|
Bare Metal Stents |
Permanent metal mesh, no drug elution |
Simple lesions, low risk of restenosis |
|
Drug-Eluting Stents |
Metal mesh with drug coating, reduces restenosis |
Complex lesions, high risk of restenosis |
|
Bioresorbable Vascular Scaffolds |
Dissolvable scaffold, temporary support |
Patients requiring temporary scaffolding, complex cases |
Learning about the stent placement procedure can ease worries for those with coronary artery disease. It’s a key treatment for blocked arteries, with several important steps.
Before the stent placement procedure, tests are done to find out where and how bad the blockage is. Blood-thinning meds are stopped a few days before to lower bleeding risks.
A catheter is guided through an artery to the blockage. Angioplasty uses a balloon to widen the artery. Then, a stent is put in to keep it open, improving blood flow.
Recovery after stent placement usually means a short stay in the hospital for checks. Patients get advice on post-procedure care. This includes meds to prevent clots and lifestyle changes for heart health.
Stenting is a common treatment for blockages in the heart’s arteries. But, there are other options based on how severe the blockage is. The right treatment depends on the patient’s health, the blockage’s location and severity, and other factors.
For mild to moderate blockages, doctors often start with medication. This approach aims to control symptoms and slow the disease’s progress. It uses different medicines to help.
|
Medication Type |
Purpose |
Examples |
|---|---|---|
|
Antiplatelet drugs |
Prevent clot formation |
Aspirin, Clopidogrel |
|
Statins |
Lower cholesterol |
Atorvastatin, Simvastatin |
|
Beta-blockers |
Reduce heart rate and blood pressure |
Metoprolol, Atenolol |
For severe or complex blockages, CABG might be needed. This surgery bypasses the blocked artery with a graft. It helps restore blood flow to the heart.
Lifestyle changes are important for all blockage levels. They help manage the disease, improve heart health, and lower the risk of further problems.
Key Lifestyle Changes:
By making these lifestyle changes, patients can see better results and enjoy a better life.
Stent placement comes with its own set of risks and benefits. It’s a common procedure that is usually safe. But, it’s not without its dangers.
Complications can include infection, reclosure of the artery, and stent dislodgement. These risks are low but need careful thought and watch after the procedure.
Infection can be treated with antibiotics, but it’s important to get medical help quickly. If the artery closes again, it might need more treatment, like another stent.
The results of stent placement can differ based on how bad the blockage is. For severe blockages (>70%), stenting can greatly improve blood flow and symptoms. This can lead to better long-term health.
For moderate blockages (40-70%), the benefits are also good. But, the decision to stent depends on many factors, not just the blockage percentage.
Many people see a big boost in their quality of life after stenting. It helps restore blood flow, reducing chest pain and shortness of breath. This makes it easier to do daily activities.
The good news of stent placement, like better blood flow and fewer symptoms, often outweighs the risks. But, doctors must carefully look at each patient’s situation. They should talk about the risks and benefits in detail.
Life after getting a stent means taking medicine, making lifestyle changes, and getting regular check-ups. Knowing these steps is key for a good recovery and keeping your heart healthy.
Patients often take antiplatelet meds after a stent to stop clots. These meds help keep the artery open. Usually, doctors prescribe a mix of aspirin and a P2Y12 inhibitor like clopidogrel.
How long you need these meds depends on the stent type and your health risks. Most doctors say to take them for at least a year. Sticking to your meds is important to avoid stent problems.
Right after getting a stent, you should avoid hard work for a few days. But, most people can go back to normal in about a week. It’s best to start slow with exercise and talk to your doctor before doing anything too tough.
|
Activity |
Recommended Timing |
Guidelines |
|---|---|---|
|
Light Exercise (e.g., walking) |
Within a few days |
Start with short sessions and gradually increase duration |
|
Strenuous Exercise |
After 7-10 days |
Consult with a healthcare provider before resuming strenuous activities |
|
Heavy Lifting |
After 1-2 weeks |
Avoid heavy lifting until cleared by a healthcare provider |
Regular visits with your cardiologist are important after a stent. They check how well the stent is working and your heart health. This helps catch any problems early.
Also, watch out for signs like chest pain or trouble breathing. If you notice these, get help right away.
Understanding what you need for meds, activity, and check-ups helps you manage your health better. This way, you can live a better life after getting a stent.
Different patient groups, like the elderly and those with diabetes or multiple blockages, need special care. Their health issues make it important to tailor stent placement for the best results.
Elderly patients face unique challenges due to health problems and less physical strength. Careful pre-procedural assessment is key to reduce risks. They might need special medication adjustments and closer watch during the procedure.
Diabetic patients are more likely to face complications after stent placement. Strict glycemic control is vital for better results. They might also benefit from drug-eluting stents, which can lower restenosis risk.
Those with many or widespread blockages need a detailed treatment plan. Multivessel stenting or a mix of stenting and CABG might be options. The choice depends on the blockage’s complexity, the patient’s health, and the procedure’s benefits and risks.
Here are the main points to keep in mind for these patients:
Managing coronary artery disease often means using stents to open blocked arteries. Doctors decide if a stent is needed based on the patient’s health and the benefits and risks. This choice is made for each patient individually.
A summary of stent placement shows how key it is to know the blockage level. Blockages between 40-70% might be treated with medicine or lifestyle changes. But, blockages over 70% usually need a stent.
Dealing with coronary artery disease requires a full plan. This includes tests like coronary angiography and ultrasound. These help doctors understand how bad the blockages are and the heart’s function. This way, they can decide the best course of action for stent placement.
In short, stents are a key way to fix blocked arteries. By looking at each patient’s situation and weighing the pros and cons, doctors can manage heart disease well. This helps improve patient outcomes.
A blockage of 70% or more is often significant and may need a stent. But, other factors like symptoms and heart function also matter. The location of the blockage is also important.
Tests like coronary angiography and intravascular ultrasound measure blockage severity. Fractional flow reserve (FFR) measurement is also used. These help doctors decide the best treatment.
Signs include chest pain, shortness of breath, and fatigue. Dizziness is another warning sign. It’s important to recognize these symptoms to get medical help quickly.
There are bare metal stents, drug-eluting stents, and bioresorbable vascular scaffolds. The right stent depends on the blockage and the patient’s health.
The process includes preparation, angioplasty, and stenting. After, there’s recovery and aftercare. Patients are watched for hours and might stay overnight in the hospital.
Yes, for mild blockages, medication is used. For complex blockages, bypass grafting is an option. Lifestyle changes help with all blockage levels. The treatment choice depends on the blockage and the patient.
Risks include bleeding and infection. But, stents can reduce symptoms and prevent heart attacks. The outcome depends on the blockage and the patient’s health.
Patients need to take clotting medicine and follow activity rules. They also need to go to follow-up appointments. Monitoring is key to ensure the stent works right.
The elderly, diabetics, and those with complex blockages face unique challenges. Treatment decisions and outcomes can be influenced by these factors.
Diet, exercise, and quitting smoking are key. These changes can help manage blockages and improve heart health.
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://pubmed.ncbi.nlm.nih.gov/25249586/
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!