Last Updated on November 26, 2025 by Bilal Hasdemir
Prostate cancer can greatly affect a patient’s life, including their bowel habits. The prostate and rectum are close and share nerves, leading to bowel changes in prostate cancer patients. Knowing about these changes is key for those going through treatment. It helps them manage symptoms and feel better overall.
Prostate cancer symptoms can be tough to deal with, and bowel changes make it worse. By looking into how prostate health and bowel habits are connected, we hope to offer insights. These insights can help patients feel more confident during their treatment.
Key Takeaways
- Prostate cancer can affect bowel habits due to its proximity to the rectum.
- Changes in bowel movements are common among prostate cancer patients.
- Understanding these changes is key for managing symptoms.
- Prostate health and colon health are closely linked.
- Recognizing the impact of prostate cancer on bowel habits can improve patient care.
The Anatomical Relationship Between Prostate and Rectum
It’s important to know how close the prostate and rectum are. This closeness is why prostate cancer can change how we go to the bathroom. The prostate is below the bladder and in front of the rectum, affecting bowel function.
Location and Proximity of the Prostate to the Rectum
The prostate and rectum are very close. Any changes in the prostate can affect the rectum. This closeness is why prostate cancer can cause bowel symptoms.
How This Proximity Can Lead to Bowel Symptoms
Prostate cancer can press on the rectum, causing bowel symptoms. Symptoms can be constipation, diarrhea, or even bleeding. The symptoms’ severity depends on the cancer’s stage and location.
Prostate cancer can also spread to nearby tissues, like the rectum. This can make bowel symptoms worse. It shows why treating prostate cancer needs a full approach.
The Pelvic Floor Muscles and Their Role
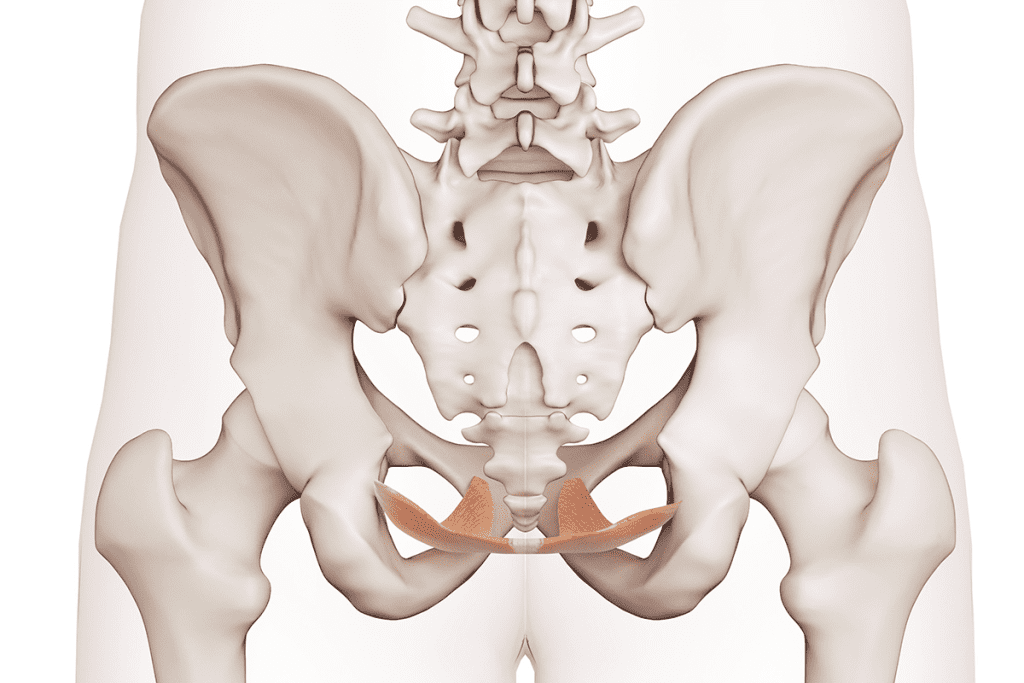
The pelvic floor muscles are key for normal bowel function. They support the rectum and control bowel movements. In prostate cancer, these muscles can be weakened by the cancer or treatments.
Doing Kegel exercises can help strengthen these muscles. But, it’s important for patients to talk to their doctor about a personalized plan.
| Muscle Group | Function | Impact of Prostate Cancer |
| Pelvic Floor Muscles | Support rectum, control bowel movements | Can be weakened by cancer or its treatment |
| Sphincter Muscles | Control anal opening | May be affected by local invasion or nerve damage |
The relationship between the prostate and rectum is complex. It affects bowel function in prostate cancer patients. Knowing this relationship helps manage bowel symptoms better.
Understanding Prostate Cancer and Its Progression
Prostate cancer is a complex disease that affects the prostate gland and nearby organs. It progresses through different stages. Understanding this progression is key to knowing how it impacts the body.
Overview of Prostate Cancer
Prostate cancer starts when cells in the prostate gland grow out of control. Early-stage prostate cancer often doesn’t show symptoms. This makes regular screenings very important for catching it early.
As the disease gets worse, it can spread to nearby tissues and organs. This can lead to symptoms like changes in bowel habits.
Stages of Prostate Cancer
Prostate cancer goes through several stages, from early to advanced. These stages are usually divided into:
- Localized prostate cancer: Cancer is only in the prostate gland.
- Locally advanced prostate cancer: Cancer has spread to tissues around the prostate.
- Metastatic prostate cancer: Cancer has spread to distant parts of the body, like bones or lymph nodes.
How Advanced Prostate Cancer Can Affect Surrounding Organs

Advanced prostate cancer can harm nearby organs, including the rectum. As it grows, it can put mechanical pressure on the rectum. This can cause symptoms like constipation or diarrhea.
Common Initial Symptoms
The first signs of prostate cancer can be hard to notice. Common symptoms include:
- Changes in urinary habits
- Bowel disturbances, such as constipation or diarrhea
- Pain or discomfort in the pelvic area
Spotting these symptoms early is vital. It helps with timely medical care and managing the disease effectively.
Direct Effects of Prostate Cancer on Bowel Function
Prostate cancer can directly affect bowel function as it progresses. The prostate is close to the rectum and shares nerves. This makes it likely that prostate cancer will impact bowel habits.
Mechanical Pressure on the Rectum
Prostate cancer can press against the rectum as it grows. This can narrow or block the rectum.
This pressure can cause constipation, trouble passing stools, or feeling like you didn’t fully empty your bowels. Sometimes, it can even change the shape or size of your stool.
Local Invasion in Advanced Cases
In advanced cases, prostate cancer can invade nearby tissues and organs, including the rectum. This can cause more severe symptoms like rectal pain, bleeding, or passing tumor fragments.
This invasion makes both the cancer and its treatment more complex. It often requires a team effort to manage symptoms and control the disease.
Nerve Compression and Its Effects
Nerve compression is another way prostate cancer affects bowel function. The nerves controlling bowel movements are near the prostate. As cancer grows, these nerves can be compressed or damaged.
This can lead to constipation, fecal incontinence, or trouble with bowel evacuation. Treating nerve-related symptoms often involves shrinking the tumor and relieving nerve compression.
Metastatic Spread and Bowel Implications
Metastatic spread of prostate cancer can also affect bowel function, though less directly. Spreading to the spine or pelvis can harm nerves controlling bowel function. This can cause symptoms like constipation or fecal incontinence.
| Mechanism | Bowel Symptoms | Potential Complications |
| Mechanical Pressure | Constipation, difficulty passing stools | Narrowing or obstruction of the rectum |
| Local Invasion | Rectal pain, bleeding, passage of tumor fragments | Complicated cancer treatment, bowel obstruction |
| Nerve Compression | Constipation, fecal incontinence, difficulty with bowel evacuation | Chronic bowel dysfunction, decreased quality of life |
| Metastatic Spread | Constipation, fecal incontinence | Neurological deficits, bowel obstruction |
Constipation and Prostate Cancer: The Connection
Constipation is a big problem for many prostate cancer patients. It can come from the cancer itself or its treatment. It’s key to know what causes it.
Can Prostate Cancer Cause Constipation?
Yes, prostate cancer can lead to constipation. The growing tumor can press on the rectum. This can slow down bowel movements. Mechanical pressure on the rectum is a main reason for constipation in these patients.
Mechanisms Behind Prostate-Related Constipation
There are several reasons why prostate cancer patients get constipated:
- Direct pressure from the tumor on the rectum
- Nerve compression affecting bowel function
- Changes in physical activity due to cancer-related fatigue
- Dietary alterations or medication side effects
Knowing these reasons is key to managing constipation well.
Differentiating Between Cancer-Related and Treatment-Related Constipation
It’s important to tell the difference between constipation from the cancer and from treatments. Treatment-related constipation can happen because of:
- Scarring or inflammation from surgery
- Radiation-induced damage to the rectal tissue
- Hormonal changes affecting bowel habits
Impact on Quality of Life
Constipation can really hurt a patient’s quality of life. It can cause discomfort, pain, and emotional distress. We need to tackle this issue to improve their well-being.
Understanding the link between prostate cancer and constipation helps us manage this side effect better. This improves care for prostate cancer patients.
Diarrhea as a Symptom in Prostate Cancer Patients
Prostate cancer patients may have diarrhea for several reasons. This includes the cancer itself or treatments like radiation. Diarrhea, with loose stools or frequent bowel movements, can really affect a patient’s life.
How Prostate Cancer Can Lead to Diarrhea
Diarrhea in prostate cancer patients comes from different sources. The cancer can directly harm the rectum or nerves, causing diarrhea. Treatments like radiation or surgery can also make diarrhea worse.
Radiation therapy can cause inflammation in the rectum, leading to diarrhea. Surgery, like those near the prostate, can also affect bowel habits.
Frequency and Severity Patterns
Diarrhea’s frequency and severity vary among prostate cancer patients. Some may have mild diarrhea now and then, while others face severe and ongoing issues.
It’s important to understand these patterns to manage diarrhea well. Keeping a symptom diary can help track when and how bad diarrhea is, and what might trigger it.
Managing Cancer-Related Diarrhea
Managing diarrhea in prostate cancer patients requires a few steps. Changing what you eat is often the first step. This includes avoiding foods that irritate the bowel and eating foods that help firm up stool.
Medicines like loperamide can also help control diarrhea. Sometimes, changing the treatment plan for prostate cancer is needed to reduce diarrhea symptoms.
When Diarrhea Indicates a Serious Complication
While diarrhea is usually manageable, it can sometimes signal a serious issue. Severe or ongoing diarrhea can cause dehydration and electrolyte imbalances, needing quick medical help.
It’s key to know the warning signs. These include bloody stools, severe stomach pain, or dehydration signs. If you see these, get medical help right away.
Blood in Stool: When to Be Concerned
Prostate cancer patients might see blood in their stool for many reasons. This can worry them about their disease getting worse or if treatments are working. It’s a symptom that can cause a lot of stress.
Causes of Rectal Bleeding in Prostate Cancer Patients
Rectal bleeding in prostate cancer patients can come from several places. The cancer itself, if it’s grown a lot, can cause bleeding because it’s close to the rectum. Also, treatments like radiation can cause bleeding as a side effect. We’ll look into these reasons to know when bleeding might mean something serious.
Distinguishing Between Prostate Cancer and Colorectal Cancer Symptoms
It’s important to tell apart symptoms from prostate cancer and colorectal cancer. Both can cause bleeding, but they have different reasons and meanings. Knowing the difference helps doctors and patients make better choices about treatment.
When to Seek Immediate Medical Attention
Not every case of rectal bleeding needs quick action, but some do. We’ll talk about the signs that mean you should see a doctor right away. This way, patients know when to get help fast.
Diagnostic Procedures for Rectal Bleeding
Figuring out why there’s bleeding in the rectum involves tests and exams. We’ll cover the usual tests used to find out why prostate cancer patients bleed. These include endoscopy, imaging, and biopsy.
The Colon and Prostate: Understanding Their Interconnection
The colon and prostate are connected in a way that affects health. This connection comes from their close location and shared functions.
Shared Nerve Supply and Blood Vessels
The colon and prostate are linked by shared nerve supply and blood vessels. The pelvic plexus, a network of nerves, serves both organs. This can cause pain or symptoms in one to affect the other.
The common blood supply from the inferior mesenteric artery and its branches strengthens this bond. Problems in one organ can affect the other through this blood link.
How Problems in One Organ Can Affect the Other
Problems in the prostate can cause bowel symptoms because of their close location. For example, an enlarged prostate can press on the rectum, leading to constipation or discomfort. On the other hand, colon issues like diverticulitis can cause prostatitis or affect prostate function.
This connection shows why a comprehensive approach is needed for diagnosing and treating pelvic organ issues. Doctors must look at both the colon and prostate when evaluating symptoms. This ensures accurate diagnoses and effective treatments.
Common Risk Factors for Both Prostate and Colon Issues
Prostate and colon issues share common risk factors like age, diet, and lifestyle. As men get older, the risk of prostate cancer or BPH and colon cancer increases. Eating too much processed meat and not enough fiber also raises the risk of both cancers.
- A sedentary lifestyle
- Obesity
- Smoking
These factors can make problems in both organs worse.
Importance of Screening for Both Cancers
Screening for both prostate and colon cancers is key because of their connection. Early detection of prostate cancer through PSA testing and digital rectal exams can greatly improve outcomes. Colon cancer screening, like colonoscopy, can also find cancer early.
Men over 50 should talk to their doctors about combined screening strategies. This could include both prostate and colon cancer screening in one plan.
Radiation Therapy for Prostate Cancer and Its Impact on Bowel Health
Radiation therapy for prostate cancer can cause short-term and long-term bowel problems. It’s key to know how these effects happen and how to manage them.
Acute Bowel Side Effects During Treatment
Patients may get diarrhea, urgency, and discomfort during treatment. This is because radiation irritates the rectum’s lining, causing inflammation and changes in bowel habits.
Managing Acute Side Effects: Eating a low-fiber diet and using medications for diarrhea can help. Drinking plenty of water is also important.
Long-Term Bowel Problems After Radiotherapy
Some patients face long-term bowel issues after treatment. These can include diarrhea, rectal bleeding, and fecal incontinence. The severity and how long these symptoms last vary.
Strategies to Minimize Radiation-Induced Bowel Damage
Radiation oncologists use advanced methods to target tumors precisely. Intensity-modulated radiation therapy (IMRT) is one method that helps reduce bowel side effects.
| Strategy | Description | Benefit |
| IMRT | Delivers precise radiation doses to the tumor | Reduces exposure to surrounding healthy tissues |
| Dietary Adjustments | Low-fiber diet during treatment | Helps manage diarrhea and discomfort |
| Medications | Anti-diarrheal medications | Controls diarrhea and urgency |
New Radiation Techniques and Bowel Sparing Approaches
New methods like proton beam therapy and stereotactic body radiation therapy (SBRT) aim to reduce bowel damage. They allow for more precise tumor targeting, lowering the risk of bowel side effects.
Understanding radiation therapy’s bowel side effects and using strategies to lessen them is vital. This way, patients and healthcare providers can improve treatment outcomes and quality of life.
Surgery for Prostate Cancer: Possible Bowel Problems
It’s important to know about bowel problems after prostate cancer surgery. This surgery, like radical prostatectomy, can change a patient’s life a lot. It can affect how they go to the bathroom.
Bowel Issues Following Radical Prostatectomy
Radical prostatectomy is a common surgery for prostate cancer. It removes the prostate gland. But, it can cause bowel problems because of where the prostate is near the rectum and the nerves that control bowel movements. Common issues include constipation, diarrhea, and fecal incontinence.
A study in the Journal of Urology found that bowel problems after this surgery can really affect a patient’s life. It shows how important talking to the doctor before surgery and getting help after it.
| Bowel Issue | Prevalence | Management Strategies |
| Constipation | 20-30% | Dietary changes, laxatives |
| Diarrhea | 10-20% | Anti-diarrheal medications, dietary adjustments |
| Fecal Incontinence | 5-15% | Pelvic floor exercises, biofeedback therapy |
Temporary vs. Permanent Changes in Bowel Function
Bowel changes after prostate surgery can last a short time or forever. Temporary changes usually get better over time. But, permanent changes might need ongoing care.
A study in European Urology found that some men get better bowel function within a year. But, others might keep having problems.
Recovery Timeline and Expectations
How long it takes for bowel function to get better after prostate cancer surgery varies. Most patients see some improvement in the first few months. It can take up to a year or more for full recovery.
“The recovery process after prostate surgery is unique to each individual. While some men may experience a quick return to normal bowel function, others may require more time and support.” – A Urologist
Minimally Invasive Surgery and Bowel Outcomes
Minimally invasive surgery, like robotic-assisted laparoscopic prostatectomy, might have fewer bowel problems than traditional surgery. These methods use smaller cuts and cause less damage. This could mean a quicker recovery and fewer bowel issues.
Knowing about bowel problems after prostate cancer surgery helps patients prepare better. It lets them make informed choices about their treatment.
Hormone Therapy and Its Effects on Digestive Health
Hormone therapy is a common treatment for prostate cancer. It can greatly affect digestive health. We need to know how androgen deprivation therapy (ADT) impacts the digestive system. We also need to find ways to manage these effects.
How Androgen Deprivation Therapy Affects the Digestive System
ADT is a key treatment for advanced prostate cancer. It lowers male hormone levels to slow cancer cell growth. But, this change can cause side effects, including digestive issues. Some patients may experience constipation or diarrhea due to hormonal changes.
Managing Bowel Changes During Hormone Treatment
It’s important to manage bowel changes during hormone therapy. Here are some tips:
- Eat more fiber from fruits, vegetables, and whole grains to help with bowel movements.
- Drink plenty of water all day to stay hydrated.
- Do regular physical activity to help bowel function.
- Consider probiotics or supplements with a healthcare provider’s advice.
Long-Term Digestive Issues with Extended Hormone Therapy
Long-term use of hormone therapy can cause digestive problems. These may include ongoing bowel changes, weight issues, or other stomach symptoms. It’s key to watch for these effects and adjust treatment plans as needed to protect digestive health.
Intermittent vs. Continuous Hormone Therapy
The choice between intermittent and continuous hormone therapy depends on several factors. These include the cancer stage and the patient’s health. Intermittent therapy, with its cycles of treatment, may reduce side effects like digestive issues. But, the best choice should be made with a healthcare provider, considering the patient’s specific needs and cancer type.
Understanding hormone therapy’s effects on digestive health is vital. By managing these effects, patients can better handle their treatment. It’s important to talk openly with healthcare providers about any concerns or symptoms during treatment.
Chemotherapy for Prostate Cancer: Bowel Side Effects
Patients with prostate cancer who get chemotherapy often face bowel side effects. These can really impact their life quality. Chemotherapy is key in treating prostate cancer but can cause stomach problems.
Common Digestive Issues During Chemotherapy
Patients may deal with diarrhea, constipation, and nausea during treatment. These symptoms can be tough to handle and affect daily life. Diarrhea can cause dehydration if not managed right. Constipation can lead to discomfort and pain.
We suggest patients keep a symptom diary. This helps healthcare providers give better care.
Blood in Stool While on Chemotherapy
Blood in the stool is a serious symptom during chemotherapy. It could be from the treatment or another issue like hemorrhoids. If you see blood, tell your doctor right away.
This symptom can be scary. Quick action is needed to find out why and how to treat it.
Supportive Care During Treatment
Supportive care is key in handling bowel side effects during chemotherapy. This includes diet changes, medicines, and other ways to improve life quality.
- Dietary changes, like more fiber or avoiding certain foods, can help symptoms.
- Medicines like anti-diarrheal drugs or laxatives can control bowel movements.
- It’s important to stay hydrated, mainly if you have diarrhea.
Recovery of Bowel Function After Chemotherapy
After chemotherapy, bowel function usually goes back to normal. But, this can differ for each person. Some might have ongoing bowel problems that need ongoing care.
We keep a close eye on bowel health after treatment. We also guide patients on managing any lasting effects.
Enlarged Prostate (BPH) vs. Prostate Cancer: Differences in Bowel Symptoms
It’s important to know the difference between an enlarged prostate and prostate cancer. Both can affect your bowel habits. But, the reasons and effects are quite different.
Can Enlarged Prostate Cause Constipation?
Yes, an enlarged prostate, or BPH, can lead to constipation. The prostate is close to the rectum. So, when it gets bigger, it can press on the rectum and slow down bowel movements.
We’ll look into how BPH causes constipation more closely.
Distinguishing Between BPH and Cancer Symptoms
BPH and prostate cancer can both cause bowel problems. But, the symptoms and how severe they are can differ. For example, prostate cancer can cause more serious symptoms because it can spread or grow bigger.
Prostate cancer might also cause urinary problems, pain, or weight loss. BPH usually just causes urinary issues like needing to go often or having a weak stream.
| Symptom | BPH | Prostate Cancer |
| Constipation | Possible due to prostate size and pressure on rectum | Possible, if advanced or metastatic |
| Urinary Symptoms | Common (frequency, urgency, weak stream) | Common, may include obstruction or retention |
| Pain | Rarely associated directly with BPH | May be present, with advanced disease |
| Systemic Symptoms | Not typical for BPH | May occur with advanced prostate cancer (weight loss, fatigue) |
When Bowel Changes Warrant Further Investigation
If bowel changes last or come with other worrying signs like bleeding, pain, or big changes in bowel habits, see a doctor.
It’s best to get checked if you notice these symptoms to make sure there’s no serious issue.
Treatment Options for BPH-Related Bowel Issues
Treatments for BPH bowel problems usually aim to shrink the prostate. This can be done with medicines or surgery.
Changing your diet can also help with constipation. We’ll talk about these changes in more detail to help manage BPH bowel symptoms.
Psychological Impact of Bowel Changes in Prostate Cancer Patients
Bowel changes from prostate cancer can cause a lot of emotional pain for patients. It’s hard to deal with changes in bowel function. It can affect many parts of a patient’s life.
Coping with Altered Bowel Function
Dealing with bowel changes needs a wide approach. Learning about your condition and the changes you might see is helpful. Knowing why and how bowel changes happen can help you manage your symptoms better.
Keeping a symptom diary is a good idea. It helps spot patterns and what might cause problems. This way, you can focus on what works best for you.
Social and Emotional Challenges
Dealing with bowel changes can be tough socially and emotionally. Patients might feel embarrassed, anxious, or depressed because of their bowel issues.
It’s important to remember you’re not alone. Getting support from family, friends, and groups can really help. It makes facing these challenges easier.
Support Resources and Counseling Options
There are many ways to cope with the emotional side of bowel changes. Counseling and therapy offer strategies and support.
- Professional counseling services
- Support groups for prostate cancer patients
- Online resources and forums
Communication Strategies with Healthcare Providers
Talking openly with your healthcare team is key. You should be able to share your bowel changes and any emotional struggles.
Writing down questions and concerns before visits helps make sure everything is covered. Don’t forget to ask about support services and resources too.
Dietary Strategies for Managing Bowel Issues in Prostate Cancer Patients
Dietary changes can greatly improve bowel health in prostate cancer patients. They offer a way to manage symptoms effectively. We will look at different dietary strategies to help with bowel issues linked to prostate cancer.
Foods That May Help Alleviate Constipation
Constipation is common in prostate cancer patients. Eating foods high in fiber can help. We suggest eating more:
- Fruits such as berries, apples, and pears
- Vegetables like broccoli, carrots, and leafy greens
- Whole grains including brown rice, quinoa, and whole-wheat bread
- Legumes such as beans, lentils, and chickpeas
These foods not only help with constipation but also provide essential nutrients.
Dietary Modifications for Diarrhea Management
Some prostate cancer patients may have diarrhea. This can be due to the cancer or treatment. To manage diarrhea, we recommend:
- Eating smaller, more frequent meals
- Avoiding high-fiber foods that can worsen diarrhea
- Incorporating foods that are easy to digest, such as bananas, rice, and toast
- Staying hydrated with plenty of fluids, preferably electrolyte-rich beverages
These dietary changes can help manage diarrhea and prevent dehydration.
Nutritional Support During Cancer Treatment
Nutritional support is key during prostate cancer treatment. A balanced diet is essential. It should include:
- Adequate protein to maintain muscle mass and strength
- Healthy fats for energy and nutrient absorption
- Complex carbohydrates for sustained energy
- Vitamins and minerals to support overall health
A well-balanced diet helps patients tolerate treatment better and recover more effectively.
Hydration and Fiber Considerations
Hydration and fiber intake are vital for bowel health. We recommend:
- Drinking plenty of water throughout the day
- Gradually increasing fiber intake to allow the gut to adjust
- Monitoring bowel movements and adjusting diet as needed
By focusing on hydration and fiber, patients can better manage their bowel health.
When to Seek Medical Help for Bowel Changes
Bowel changes can be a big worry for people with prostate cancer. It’s important to know when to get help. As prostate cancer grows or is treated, patients might face bowel symptoms that affect their life quality.
Warning Signs That Require Immediate Attention
Some bowel changes need quick medical help. These include:
- Severe abdominal pain that doesn’t go away
- Rectal bleeding or blood in the stool
- Constipation lasting more than a few days
- Diarrhea that keeps coming back or causes dehydration
- Incontinence or loss of bowel control
If you see any of these signs, call your doctor right away.
Tracking and Reporting Bowel Symptoms
Writing down your bowel symptoms helps your healthcare team understand you better. Keep track of:
| Symptom | Frequency | Severity |
| Constipation | Daily | Moderate |
| Diarrhea | Twice a day | Severe |
| Bloating | Intermittent | Mild |
This info is key to managing your symptoms well.
Questions to Ask Your Healthcare Provider
When talking about bowel changes with your doctor, ask:
- What could be causing my bowel symptoms?
- Are my symptoms linked to my prostate cancer or its treatment?
- What treatments can help with my bowel symptoms?
- Are there lifestyle changes that can help my symptoms?
Being active in your care can help manage bowel changes better.
Coordinating Care Between Oncology and Gastroenterology
For prostate cancer patients with bowel changes, team care is key. Your healthcare team can:
- Check how prostate cancer treatment affects your bowel health
- Make a plan to handle bowel symptoms
- Keep an eye on your condition and change treatments as needed
Together, patients get care that covers both cancer treatment and bowel health.
Conclusion: Maintaining Bowel Health During Prostate Cancer Journey
Maintaining bowel health is key for prostate cancer patients. The prostate and rectum are closely linked. Changes in bowel habits can signal prostate cancer.
Prostate cancer and its treatments can cause bowel problems. These include constipation, diarrhea, and rectal bleeding. Knowing these side effects helps manage them better.
Patients can manage their prostate cancer journey by understanding the link between colon and prostate health. They can use dietary strategies to handle bowel issues. It’s also important to know when to seek medical help and the role of both oncology and gastroenterology in care.
As we improve prostate cancer treatment, focusing on bowel health is vital. This approach helps improve the well-being of patients. It supports them every step of the way.
FAQ
Can prostate cancer cause changes in bowel habits?
Yes, prostate cancer can change your bowel habits. This is because it’s close to the rectum. It can also affect nerves and tissues nearby.
How does an enlarged prostate affect bowel movements?
An enlarged prostate can make bowel movements hard. It puts pressure on the rectum and nerves around it.
Can radiation therapy for prostate cancer cause bowel problems?
Yes, radiation therapy can lead to bowel problems. These include diarrhea, rectal bleeding, and bowel obstruction.
What are the bowel side effects of hormone therapy for prostate cancer?
Hormone therapy can change your bowel habits. You might experience constipation, diarrhea, or changes in appetite.
Can chemotherapy for prostate cancer cause bowel issues?
Yes, chemotherapy can cause bowel issues. These include diarrhea, constipation, and blood in stool.
How can I manage bowel changes during prostate cancer treatment?
To manage bowel changes, try dietary changes and stay hydrated. Also, talk to your healthcare provider about your symptoms.
What is the connection between prostate cancer and constipation?
Prostate cancer can cause constipation. It does this by putting pressure on the rectum and affecting nerves and bowel habits.
Can prostate cancer cause diarrhea?
Yes, prostate cancer can cause diarrhea. This is more common during treatment, due to radiation, hormone, or chemotherapy.
When should I seek medical attention for bowel changes during prostate cancer treatment?
Seek medical attention for severe bowel changes. This includes bloody stools, severe diarrhea, or bowel obstruction.
How can I differentiate between bowel symptoms caused by prostate cancer and other conditions?
To tell if symptoms are from prostate cancer or other conditions, get a thorough medical check-up. This includes tests and reviewing your medical history.
What are the shared risk factors for prostate and colon cancer?
Risk factors for both prostate and colon cancer include age, family history, and certain genetic mutations.
Can an enlarged prostate cause constipation?
Yes, an enlarged prostate can cause constipation. It does this by putting pressure on the rectum and affecting nerves.
How does prostate cancer affect the rectum?
Prostate cancer can affect the rectum. It does this by putting pressure on it, invading tissues, and changing bowel habits.
What are the dietary strategies for managing bowel issues during prostate cancer treatment?
To manage bowel issues, increase fiber intake and stay hydrated. Also, avoid foods that make symptoms worse.
Can prostate cancer cause blood in stool?
Yes, prostate cancer can cause blood in stool. This is more likely if the cancer has invaded the rectum or if you’re experiencing bleeding from treatments.
References
- Kishan, A. U., Nikitas, J., et al. (2025, February 2). Men with early urinary or bowel issues after prostate radiation therapy face higher long-term risks of complications. UCLA Health Jonsson Comprehensive Cancer Center. https://www.uclahealth.org/news/release/ucla-led-study-establishes-link-between-early-side-effects
- Forslund, M., et al. (2019). Effects of a nutrition intervention on acute and late bowel symptoms after radiotherapy for prostate cancer. Radiotherapy and Oncology, 137, 172-178. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7256032/
- Heemsbergen, W. D., et al. (2025). Post-treatment changes in bowel and urinary function after prostate cancer therapy: A longitudinal study. Radiotherapy and Oncology, 180, 140-147. https://www.sciencedirect.com/science/article/pii/S240563082500045X
- Prostate Cancer UK. (2024, October 31). Bowel problems. https://prostatecanceruk.org/prostate-information-and-support/living-with-prostate-cancer/bowel-problems/