Last Updated on November 26, 2025 by Bilal Hasdemir
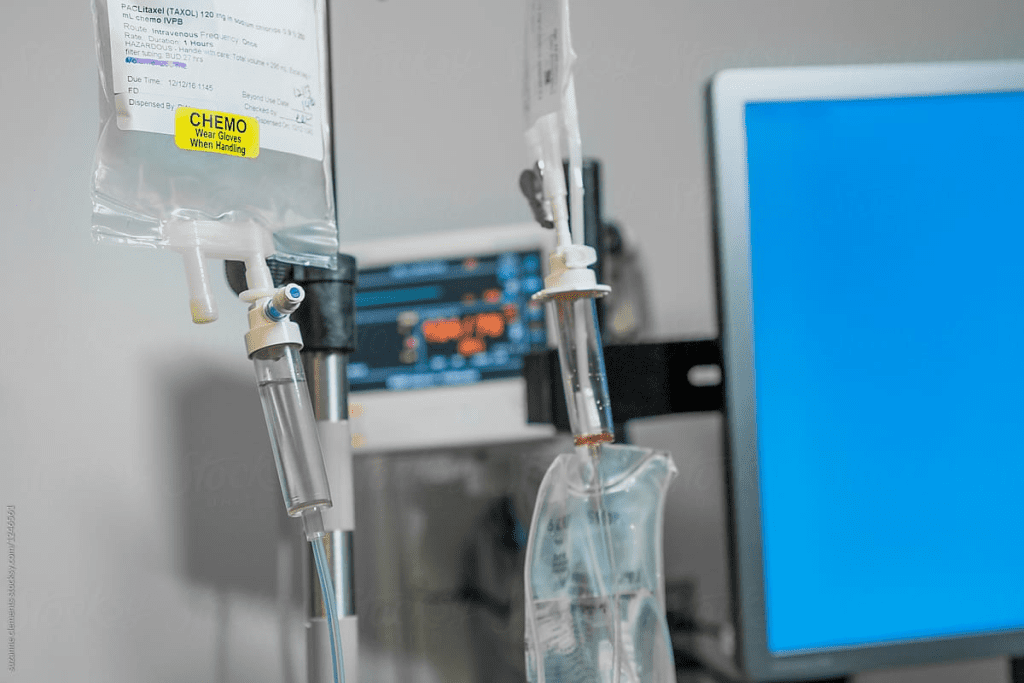
Cancer treatment has grown more complex, with many therapies available. Adjuvant chemotherapy is one, given after primary treatment to lower cancer recurrence risk.
Every year, millions are diagnosed with cancer, making the choice to have chemotherapy tough. Knowing the good and bad of adjuvant therapy is key to smart cancer care choices.
The debate on adjuvant chemotherapy‘s value goes on. Some see big benefits, while others face harsh side effects.
Key Takeaways
- Cancer recurrence can be reduced with adjuvant chemotherapy.
- Understanding the benefits and drawbacks is key for smart choices.
- Chemotherapy can have big side effects.
- The value of adjuvant therapy differs for each patient.
- Smart cancer care choices need careful thought.
Understanding Adjuvant Therapy in Cancer Treatment
In the fight against cancer, adjuvant therapy is key to better patient outcomes and survival. It’s a treatment added to the main therapy to boost its power.
The Definition and Purpose of Adjuvant Therapy
Adjuvant therapy is any treatment added to the main treatment to make it more effective. Its main goal is to get rid of any cancer cells left after the main treatment. This helps lower the chance of cancer coming back.
Adjuvant treatments can be chemotherapy, radiation, hormone therapy, or targeted therapy. The choice depends on the cancer type and the patient’s health. It’s tailored to each person’s needs.
How Adjuvant Treatments Fit into the Cancer Care Timeline
The cancer care timeline includes many stages, from diagnosis to follow-up. Adjuvant therapy comes after the main treatment, like surgery. It aims to kill any cancer cells missed during surgery.
Knowing where adjuvant chemotherapy definition fits in is important. It’s given after surgery to target any remaining cancer cells. This step helps lower the risk of cancer coming back and improves survival chances.
Adding adjuvant therapy to cancer treatment plans makes care more complete. It attacks cancer from different sides, improving the chances of a good outcome.
What Makes Chemotherapy an Adjuvant Treatment?
Adjuvant chemotherapy is a treatment given after the main therapy to boost its success. Its main aim is to get rid of any cancer cells left behind. These cells might not be seen or could have spread from the original tumor.
The Role of Adjuvant Chemotherapy After Primary Treatment
After the main treatment, like surgery, adjuvant chemotherapy is used. It targets tiny cancer cells that imaging tests can’t find. These cells can lead to cancer coming back if not treated.
Goals of Adjuvant Chemotherapy
The main goals of adjuvant chemotherapy are to lower the chance of cancer coming back and to increase survival rates. By killing off any leftover cancer cells, it helps stop cancer from returning.
| Treatment Stage | Purpose | Benefit |
| Primary Treatment | Remove the main tumor | Reduces the bulk of the cancer |
| Adjuvant Chemotherapy | Kill any remaining cancer cells | Reduces the risk of recurrence |
Adjuvant vs. Neoadjuvant Chemotherapy: Key Differences
It’s important to know the difference between adjuvant and neoadjuvant chemotherapy. Both are types of chemotherapy but are used at different times and for different reasons. This knowledge helps patients understand their treatment options better.
Timing and Purpose of Each Approach
Neoadjuvant chemotherapy is given before the main treatment, like surgery or radiation. Its main goals are to make the tumor smaller and kill cancer cells that might have spread. This helps doctors see how well the cancer responds to the treatment.
Adjuvant chemotherapy is given after the main treatment. Its main goal is to kill any cancer cells left behind. This reduces the chance of cancer coming back.
When Doctors Choose One Over the Other
The choice between neoadjuvant and adjuvant chemotherapy depends on many factors. These include the cancer type and stage, the patient’s health, and the treatment goals. For example, neoadjuvant chemotherapy might be used for big tumors that are hard to remove. Adjuvant chemotherapy is often used when there’s a high risk of cancer coming back.
Doctors make this choice based on each patient’s unique situation. They consider the patient’s condition and treatment goals carefully.
Common Types of Adjuvant Chemotherapy Drugs
Adjuvant chemotherapy drugs are key in fighting cancer. They help get rid of any cancer cells left after the first treatment. This lowers the chance of cancer coming back.
Alkylating Agents and Platinum Compounds
Alkylating agents attach to DNA in cancer cells, stopping them from copying. Cyclophosphamide and chlorambucil are examples. Platinum compounds, like cisplatin and oxaliplatin, also damage DNA, causing cancer cells to die.
These drugs are used in many cancer treatments. They help with ovarian, testicular, and some lung cancers.
Antimetabolites and Topoisomerase Inhibitors
Antimetabolites act like DNA or RNA parts, stopping cancer cells from making new DNA or RNA. Fluorouracil (5-FU) and gemcitabine are examples. Topoisomerase inhibitors, like doxorubicin and etoposide, mess with enzymes cancer cells need to grow.
These drugs treat many cancers, including breast, lung, and stomach cancers.
Antimicrotubule Agents and Targeted Therapies
Antimicrotubule agents, like paclitaxel and docetaxel, stop cancer cells from dividing. Targeted therapies, such as trastuzumab for HER2-positive breast cancer and bevacizumab for various cancers, target specific cancer molecules.
Using these drugs in adjuvant chemotherapy has greatly helped cancer patients.
The Science Behind Adjuvant Chemotherapy’s Effectiveness
Adjuvant chemotherapy works by getting rid of tiny cancer cells left after the main treatment. This method is key in cutting down cancer coming back and boosting survival chances for many cancers.
Eliminating Micrometastases
Micrometastases are tiny cancer groups that have spread but are too small to find with usual tests. Adjuvant chemotherapy goes after these tiny cells, lowering the chance of cancer coming back. By getting rid of these tiny cancer groups, adjuvant chemotherapy greatly boosts disease-free survival rates.
Reducing Recurrence Risk
Adjuvant chemotherapy’s main goal is to lower the chance of cancer coming back. Research shows it can cut down the risk of coming back in cancers like breast, colon, and lung. This is because it kills off any leftover cancer cells that could cause cancer to come back.
Impact on Disease-Free Survival
Disease-free survival is a key way to measure how well cancer treatment works. Adjuvant chemotherapy helps by getting rid of micrometastases and lowering the risk of cancer coming back. This means better survival rates and quality of life for cancer patients.
A study on osteosarcoma patients showed how important good adjuvant treatments are. It found that treatments before diagnosis can lead to worse results. This shows how vital adjuvant chemotherapy is in fighting cancer and helping patients do better.
Measuring the Benefits: Survival Statistics and Quality of Life
Measuring the Benefits of Adjuvant Chemotherapy
Adjuvant chemotherapy is a treatment given after primary therapy to reduce the risk of cancer recurrence. It’s important for patients and healthcare providers to understand its benefits.
Understanding the Metrics
Several key metrics are used to evaluate adjuvant chemotherapy. These include absolute risk reduction, relative risk reduction, and quality-adjusted life years.
Absolute Risk Reduction (ARR)
Absolute risk reduction shows the actual difference in risk between the treatment and control groups. For example, if the risk of recurrence without treatment is 20% and with treatment is 15%, the ARR is 5%.
Relative Risk Reduction (RRR)
Relative risk reduction expresses the reduction in risk as a proportion of the original risk. Using the same example, the RRR would be 25%.
Interpreting the Data
To understand the data, it’s important to look at both ARR and RRR. ARR shows the actual risk reduction. RRR shows how effective the treatment is compared to the original risk.
| Metric | Description | Example |
| Absolute Risk Reduction (ARR) | Difference in risk between treatment and control groups | 5% |
| Relative Risk Reduction (RRR) | Proportional reduction in risk | 25% |
Quality-Adjusted Life Years (QALYs)
QALYs measure the value of health outcomes by combining quality and quantity of life. It’s a useful metric for evaluating the effectiveness of adjuvant chemotherapy.
Conclusion
In conclusion, understanding the benefits of adjuvant chemotherapy requires a look at various statistical measures. These include absolute and relative risk reductions, and quality-adjusted life years. By considering these metrics, patients and healthcare providers can make informed decisions about treatment.
Adjuvant Chemotherapy in Breast Cancer Treatment
For many breast cancer patients, adjuvant chemotherapy is key. It’s tailored to their cancer stage and type. This approach has greatly improved patient outcomes by lowering the chance of cancer coming back.
Effectiveness Based on Cancer Stage and Type
The success of adjuvant chemotherapy in breast cancer treatment depends on the cancer’s stage and type. For example, patients with hormone receptor-positive breast cancer might need different treatments than those with triple-negative breast cancer.
- Early-stage breast cancer: Adjuvant chemotherapy is often recommended for patients with high-risk features, such as large tumor size or lymph node involvement.
- Advanced-stage breast cancer: The role of adjuvant chemotherapy may be more nuanced, with treatment decisions guided by factors like overall health and previous treatments.
Genomic Testing to Guide Treatment Decisions
Genomic testing has changed how we approach adjuvant chemotherapy in breast cancer. It gives insights into the tumor’s genetic makeup. Tests like Oncotype DX help predict who will benefit from chemotherapy, leading to more personalized treatment plans.
Genomic testing helps identify patients who will likely benefit from adjuvant chemotherapy. This means avoiding unnecessary treatment for those at low risk of recurrence.
Duration and Regimens
The length and type of adjuvant chemotherapy for breast cancer vary a lot. Common treatments include combinations of anthracyclines, taxanes, and other agents. Treatment usually lasts from 3 to 6 months.
- AC-T regimen: A common chemotherapy regimen involving anthracyclines and taxanes.
- TC regimen: A regimen that combines taxanes and cyclophosphamide, often used for patients with lower-risk disease.
It’s important for patients and healthcare providers to understand adjuvant chemotherapy in breast cancer treatment. This knowledge helps make informed decisions about care.
Adjuvant Chemotherapy for Colorectal Cancer
Adjuvant chemotherapy is key in treating colorectal cancer, mainly for stage III patients. It aims to kill any cancer cells left after the first treatment. This helps lower the chance of cancer coming back.
Stage-Specific Recommendations
Choosing adjuvant chemotherapy depends on the cancer’s stage. For stage III colorectal cancer, chemotherapy is usually advised. Guidelines also suggest it for high-risk stage II patients, but this is decided individually.
- Stage III: Adjuvant chemotherapy is standard.
- High-risk Stage II: Consider adjuvant chemotherapy.
- Stage I: Generally not recommended.
Common Drug Combinations
Adjuvant chemotherapy for colorectal cancer often uses a mix of drugs. The most common are:
- FOLFOX (5-fluorouracil, leucovorin, and oxaliplatin)
- CAPOX (capecitabine and oxaliplatin)
These combos have shown to boost survival rates in stage III colorectal cancer patients.
Predictive Biomarkers
Predictive biomarkers are key in choosing adjuvant chemotherapy for colorectal cancer. Biomarkers like microsatellite instability (MSI) and KRAS/NRAS mutations help find who benefits most from certain treatments. For example, patients with microsatellite-stable (MSS) tumors might get more from certain chemotherapy.
| Biomarker | Significance |
| Microsatellite Instability (MSI) | Predicts response to certain chemotherapies |
| KRAS/NRAS Mutations | Influences the effectiveness of targeted therapies |
Other Cancers Where Adjuvant Chemotherapy Shows Promise
Adjuvant chemotherapy is being explored for lung, pancreatic, and ovarian cancers. These cancers are tough to treat because they’re often found late. The goal of using adjuvant chemotherapy is to lower the chance of cancer coming back and to help patients live longer.
Lung Cancer
In lung cancer, adjuvant chemotherapy helps patients with non-small cell lung cancer (NSCLC) live longer. Adjuvant chemotherapy lung cancer treatment usually includes platinum-based drugs. Research shows it can cut down on cancer coming back and improve survival rates.
Choosing the right chemotherapy for lung cancer depends on several things. These include the cancer’s stage, the patient’s health, and the tumor’s characteristics.
Pancreatic Cancer
For pancreatic cancer, adjuvant chemotherapy is a key treatment after surgery. Adjuvant chemotherapy pancreatic cancer often uses gemcitabine or 5-FU. Studies have found it can greatly increase survival chances for patients with resected pancreatic cancer.
Adjuvant chemotherapy is very important for pancreatic cancer because it has a high chance of coming back after surgery. Researchers are working on better chemotherapy options to improve results.
Ovarian Cancer
In ovarian cancer, adjuvant chemotherapy is used after surgery to kill any cancer cells left behind. Adjuvant chemotherapy ovarian cancer treatment usually includes platinum drugs, sometimes with taxanes. It has been shown to improve how long patients live without their cancer getting worse.
The length and type of adjuvant chemotherapy for ovarian cancer can change based on several factors. These include the cancer’s stage, how well the patient responds to treatment, and other individual factors.
Side Effects and Complications of Adjuvant Chemotherapy
Patients getting adjuvant chemotherapy often face many side effects. These can make their life quality worse. The side effects can be mild or severe and last a short or long time.
Short-Term Side Effects
Short-term side effects include feeling very tired, nausea, vomiting, hair loss, and getting sick easier. These usually go away once treatment ends.
Common Short-Term Side Effects:
- Fatigue
- Nausea and vomiting
- Hair loss
- Increased risk of infections
- Mucositis
Long-Term and Late Effects
Long-term and late effects can be serious and last a long time or even years. They include heart disease, getting new cancers, and brain problems.
| Long-Term Effect | Description |
| Cardiovascular Disease | Increased risk of heart disease and related conditions |
| Secondary Cancers | Development of new cancers due to chemotherapy |
| Cognitive Impairments | Difficulty with memory, concentration, and other cognitive functions |
A study in the Journal of Clinical Oncology says, “The risk of long-term toxicity is a critical consideration in the adjuvant setting, where the goal is to prevent cancer recurrence in patients who may already be cured.”
“The challenge lies in balancing the benefits of adjuvant chemotherapy with its possible long-term toxicities.”
Managing Chemotherapy-Related Toxicity
It’s important to manage the side effects of adjuvant chemotherapy. This helps patients feel better and live better lives. Ways to do this include changing the dose, using supportive care, and making lifestyle changes.
Strategies for Managing Toxicity:
- Dose adjustments to minimize side effects
- Supportive care medications to manage symptoms
- Lifestyle modifications, including diet and exercise
Knowing about the side effects and complications of adjuvant chemotherapy helps patients and doctors. Together, they can find ways to manage these issues. This improves treatment results and life quality.
Beyond Chemotherapy: Other Adjuvant Treatments
Adjuvant treatments go beyond chemotherapy, giving patients more ways to fight cancer. While chemotherapy is well-known, other treatments are just as important. They help improve how well patients do after treatment.
Adjuvant Radiation Therapy
Adjuvant radiation therapy uses high-energy rays to kill cancer cells. It’s often used after surgery to get rid of any cancer left behind. This therapy is great for cancers that are close together or at high risk of coming back. It helps keep cancer from coming back, which can make patients live longer without cancer.
Adjuvant Hormonal Therapy
Adjuvant hormonal therapy treats cancers that grow because of hormones. It lowers hormone levels or blocks their effects on cancer cells. It’s often used for breast and prostate cancers. By controlling hormones, it lowers the chance of cancer coming back and helps patients live longer.
Adjuvant Immunotherapy
Adjuvant immunotherapy boosts the body’s immune system to fight cancer better. It’s very helpful for certain cancers that respond well to immune treatments. This method not only lowers the chance of cancer coming back but also helps the body keep fighting cancer over time.
In summary, treatments like radiation, hormonal, and immunotherapy are key parts of cancer care. They help doctors create treatment plans that fit each patient’s needs. This can lead to better outcomes and a better quality of life for patients.
Decision-Making: When Is Adjuvant Chemotherapy Worth It?
When thinking about adjuvant chemotherapy, patients and doctors must look at both sides. They need to see if the good it does is worth the possible downsides.
| Benefits | Risks |
| Reduced risk of cancer coming back | Fatigue and weakness |
| Higher chances of living longer | Nausea and vomiting |
| Better quality of life | Hair loss and other physical changes |
It’s very important for patients and doctors to work together. This way, they can decide on the best treatment plan.
Recent Advances in Adjuvant Therapy Approaches
The field of adjuvant therapy is changing fast. We’re seeing new ways to make treatments better and safer. These changes aim to help patients get better faster and with fewer side effects.
De-escalation Strategies
De-escalation means making treatments less intense. This helps reduce side effects without losing effectiveness. It’s good for patients who are likely to do well.
- Reducing chemotherapy doses or cycles
- Omission of certain toxic agents
- Use of less intensive radiation therapy
Precision Medicine Applications
Precision medicine is changing how we treat cancer. It makes treatments fit each patient and their cancer better. This is thanks to biomarkers and genetic tests.
Key aspects of precision medicine in adjuvant therapy include:
- Genomic testing to identify predictive biomarkers
- Targeted therapies based on tumor molecular characteristics
- Risk stratification to guide treatment intensity
Novel Drug Combinations
Researchers are working on new drug combinations. These aim to make treatments work better, fight resistance, and be less harsh.
Examples include:
- Combining immunotherapy with chemotherapy or targeted therapy
- Using PARP inhibitors in BRCA-mutated cancers
- Exploring CDK4/6 inhibitors in hormone receptor-positive breast cancer
These new developments in adjuvant therapy are changing cancer treatment. They offer hope for better outcomes and a better quality of life for patients.
Conclusion: Weighing the Value of Adjuvant Chemotherapy
Adjuvant chemotherapy is key in cancer treatment. It helps get rid of cancer cells left behind and lowers the chance of cancer coming back. It’s important to understand its benefits and risks to make good choices about cancer care.
The good things about adjuvant chemotherapy depend on the cancer type and stage, and the patient’s health. Looking at survival rates, how well a person feels, and possible side effects helps make choices. This is something patients and doctors do together.
New ways to use adjuvant therapy, like precision medicine and new drug mixes, have made treatments better. As research keeps going, we’ll learn more about how to treat cancer even better.
Deciding on adjuvant chemotherapy should be a careful thought. It’s about knowing the good and bad sides, and what each person needs. By thinking about these things, patients can choose the best care for themselves. This helps them get the best results and feel better during treatment.
FAQ
What is adjuvant chemotherapy?
Adjuvant chemotherapy is a treatment given after primary therapy. It aims to lower the chance of cancer coming back. It’s a key part of cancer care, helping to get rid of any cancer cells left after the first treatment.
What is the purpose of adjuvant therapy in cancer treatment?
Adjuvant therapy’s main goal is to cut down the chance of cancer coming back. It’s a big part of cancer treatment. There’s ongoing debate about its value.
How does chemotherapy become an adjuvant treatment?
Chemotherapy is used as an adjuvant treatment after the first treatment. It aims to get rid of any cancer cells left behind. The main goal is to lower the risk of cancer coming back.
What is the difference between adjuvant and neoadjuvant chemotherapy?
Neoadjuvant chemotherapy is given before the main treatment. Adjuvant chemotherapy is given after. The choice depends on the cancer type and stage.
What are the common types of adjuvant chemotherapy drugs?
Common adjuvant chemotherapy drugs include alkylating agents and platinum compounds. Also, antimetabolites, topoisomerase inhibitors, antimicrotubule agents, and targeted therapies are used.
How does adjuvant chemotherapy work?
Adjuvant chemotherapy works by getting rid of tiny cancer cells. This lowers the risk of cancer coming back. It also improves survival without cancer.
How are the benefits of adjuvant chemotherapy measured?
Benefits are measured by survival rates and quality of life. Survival curves are also used. Metrics like absolute and relative risk reduction help evaluate its effectiveness.
Is adjuvant chemotherapy used in breast cancer treatment?
Yes, it’s a key part of breast cancer treatment, mainly for high-risk patients. Treatment choices depend on cancer stage and type. Genomic testing helps guide these decisions.
Is adjuvant chemotherapy used in colorectal cancer treatment?
Yes, it’s recommended for stage III colorectal cancer patients. Drug combinations and biomarkers guide treatment decisions.
What are the possible side effects of adjuvant chemotherapy?
Side effects range from mild to severe. They include short-term, long-term, and late effects. Ways to manage these side effects are available.
Are there other adjuvant treatments beyond chemotherapy?
Yes, treatments like radiation therapy, hormonal therapy, and immunotherapy are used. They may be used alone or with chemotherapy to improve effectiveness.
How is the decision to use adjuvant chemotherapy made?
Deciding on adjuvant chemotherapy involves weighing risks and benefits. Patient-specific factors and shared decision-making with healthcare providers are considered.
What are the recent advances in adjuvant therapy approaches?
Advances include de-escalation strategies and precision medicine. New drug combinations aim to make treatments more effective and less toxic.
References
- Dhesy-Thind, S., O’Malley, F., Seno, M. G., & Vora, S. R. (2018). Adjuvant chemotherapy for stage I-III colorectal cancer: An update. Current Oncology, 25(Suppl 1), S89“S98.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6013214/ - Early Breast Cancer Trialists’ Collaborative Group (EBCTCG). (2018). Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: An overview of the randomised trials. The Lancet, 392(10159), 1845“1859.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6265780/ - Gandara, D. R., Li, T., Wistuba, I. I., Al-Kadhimi, A., Tufail, S., and Kelly, K. (2020). Adjuvant and neoadjuvant therapy for non-small cell lung cancer. Seminars in Oncology, 47(3), 162“171.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7483863/