Last Updated on November 26, 2025 by Bilal Hasdemir
Can you live without bladder? It’s a question that often arises when discussing major cancer treatments and surgeries. Understanding how your body works after such procedures is just as important as knowing how cancer spreads ” especially to lymph nodes.
When you’re diagnosed with cancer, learning about your lymph nodes is key. Many patients wonder if they need chemotherapy if their lymph nodes are clear. Studies show that lymph node status plays a major role in diagnosis and treatment.
If your lymph nodes are clear, you may not need chemotherapy. This insight helps doctors create better, more personalized treatment plans ” improving outcomes and quality of life after serious medical procedures like bladder removal.
Key Takeaways
- The status of lymph nodes is a critical factor in determining cancer treatment.
- Clear lymph nodes may reduce the need for chemotherapy in some cases.
- Cancer treatment plans are highly individualized based on lymph node status and other factors.
- Understanding the role of lymph nodes can help patients make informed decisions.
- The presence or absence of lymph node involvement significantly affects prognosis.
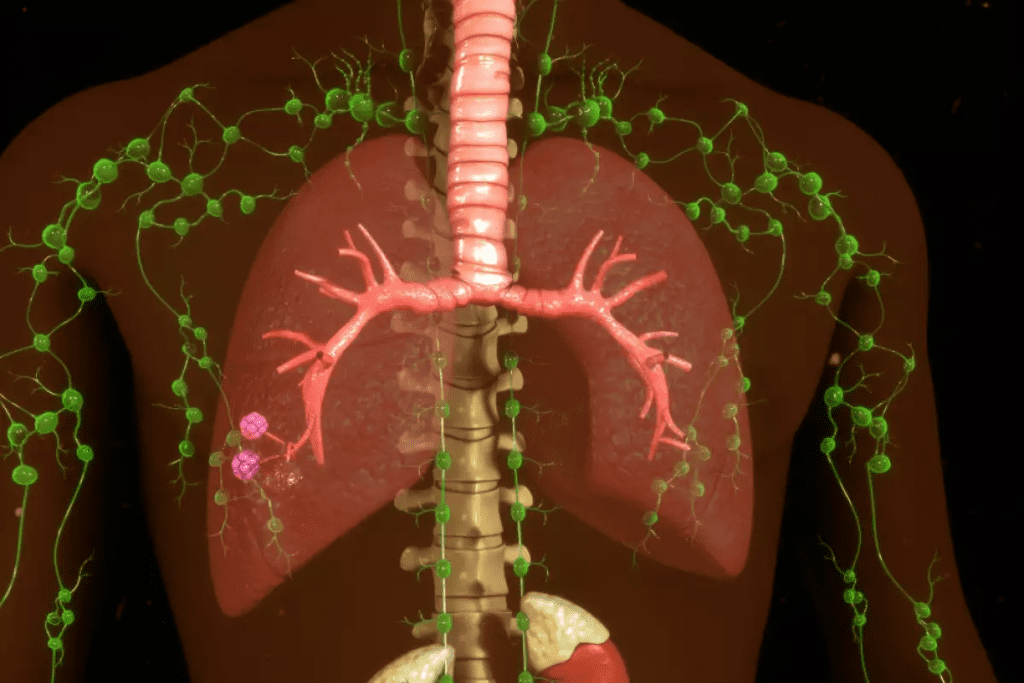
Understanding Lymph Node Status in Cancer Diagnosis
Knowing the status of lymph nodes is key to figuring out how far cancer has spread. Lymph nodes are small, bean-shaped parts of the body’s lymphatic system. They help fight infections and diseases. In cancer diagnosis, checking lymph nodes is important because it shows if cancer has spread.
What lymph nodes reveal about cancer spread
Lymph nodes filter the lymphatic system, catching pathogens like cancer cells. If cancer cells are found in lymph nodes, it means the cancer is getting worse. It might have started to spread to other parts of the body. The presence or absence of cancer cells in lymph nodes helps doctors know the cancer stage and plan treatment.
Cancer cells in lymph nodes can indicate:
- The cancer is becoming more aggressive
- The cancer might spread to other parts of the body
- More aggressive treatments, like chemotherapy or radiation, might be needed
The significance of clear vs. positive lymph nodes
“Clear” or “negative” lymph nodes mean they don’t have cancer cells. “Positive” lymph nodes have cancer cells. Clear lymph nodes suggest the cancer might be in its early stages and easier to treat. Positive lymph nodes mean the cancer has spread, making treatment harder.
| Lymph Node Status | Implication | Treatment Approach |
| Clear/Negative | Cancer is likely localized | Surgery, localized treatment |
| Positive | Cancer has spread to lymph nodes | Chemotherapy, radiation, or combination therapy |
Understanding lymph node status is vital in cancer diagnosis. It affects cancer staging and treatment choices. Knowing if lymph nodes are clear or positive helps doctors create a treatment plan tailored to each patient.
The Role of Lymph Node Assessment in Cancer Staging
Lymph node assessment is key in cancer staging. It gives vital info on cancer’s spread. Cancer staging is complex, looking at how far cancer has spread in the body.
How Cancer Staging Works
Cancer staging checks tumor size, lymph node involvement, and metastasis. This info helps decide the cancer stage. The stage then guides treatment choices.
- Tumor size and extent (T): Evaluating the size and extent of the primary tumor.
- Lymph node involvement (N): Assessing whether lymph nodes are involved.
- Presence of metastasis (M): Determining if cancer has spread to distant parts of the body.
TNM Classification System Explained
The TNM classification system is a common method for cancer staging. It offers a detailed way to check cancer spread extent.
| TNM Component | Description |
| T (Tumor) | Size and extent of the primary tumor |
| N (Node) | Lymph node involvement |
| M (Metastasis) | Presence of distant metastasis |
The TNM system helps doctors figure out cancer stage. This is key for making treatment plans. For example, lymph node status (N) is very important in cancer staging and predicting outcomes.
When Chemotherapy May Be Recommended Despite Clear Lymph Nodes
Even with clear lymph nodes, chemotherapy might be needed. Cancer treatment looks at many factors, not just lymph nodes.
Risk Factors That Influence Treatment Decisions
Several risk factors can lead to chemotherapy, even with clear lymph nodes. These include:
- Tumor size and grade: Big tumors or high-grade ones might need chemotherapy because they grow fast.
- Cancer type and stage: Some cancers, like high-risk or advanced ones, might need chemotherapy, no matter the lymph nodes.
- Genetic mutations: Certain genetic changes can mean a higher risk of cancer coming back.
- Patient’s overall health: A patient’s health and how well they can handle treatment also play a role.
Doctors look at these factors to decide the best treatment for each patient.
Cancer Types That Often Require Chemo Regardless of Lymph Status
Some cancers often need chemotherapy, even with clear lymph nodes. These include:
- Aggressive breast cancers: Like triple-negative breast cancer, which spreads fast.
- High-risk prostate cancers: Prostate cancers with high-risk features might need chemotherapy.
- Advanced ovarian cancers: Ovarian cancers found early on often need chemotherapy.
Knowing the details of a patient’s cancer is key to deciding on chemotherapy.
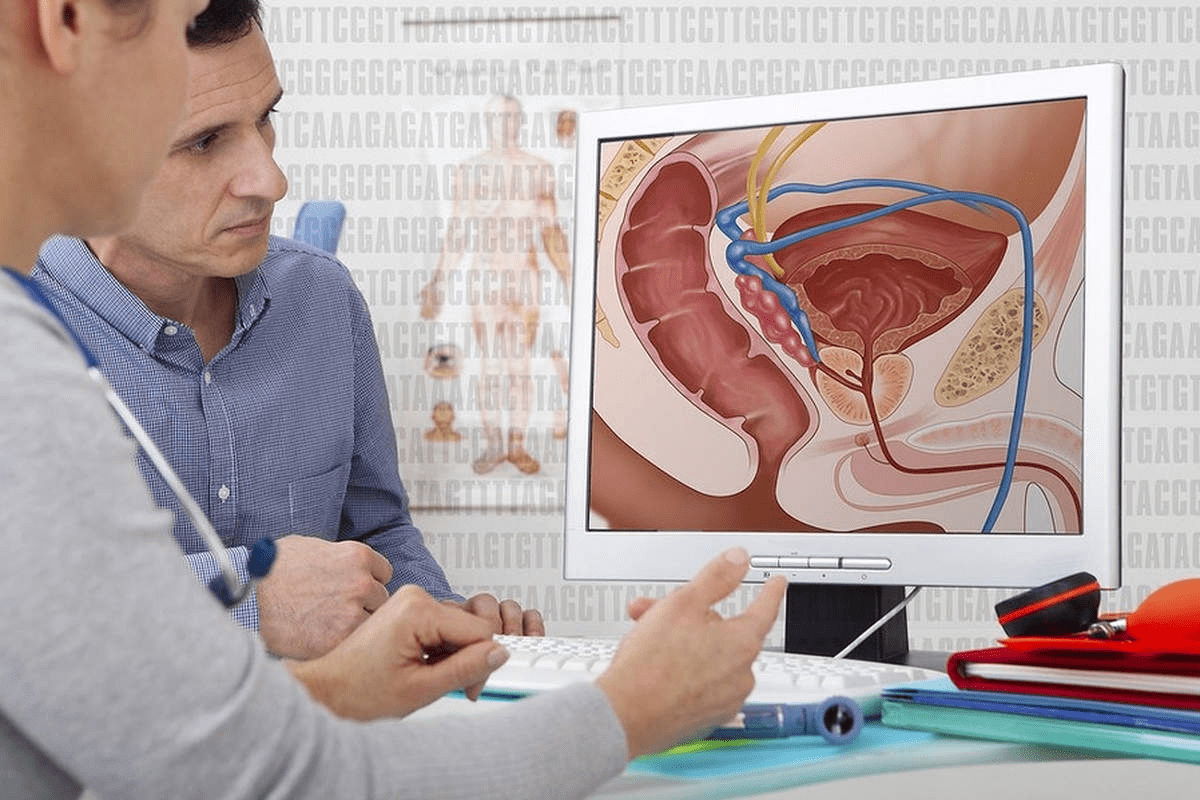
Bladder Cancer: Lymph Node Status and Treatment Decisions
Lymph nodes play a big role in bladder cancer diagnosis and treatment. They filter out harmful substances, including cancer cells. The condition of lymph nodes greatly affects treatment choices and patient results.
How Bladder Cancer Spreads
Bladder cancer starts in the bladder lining and can grow deeper. Cancer cells can break off and travel to lymph nodes. This spread shows how serious the cancer is. Lymph node involvement often means treatments need to be stronger.
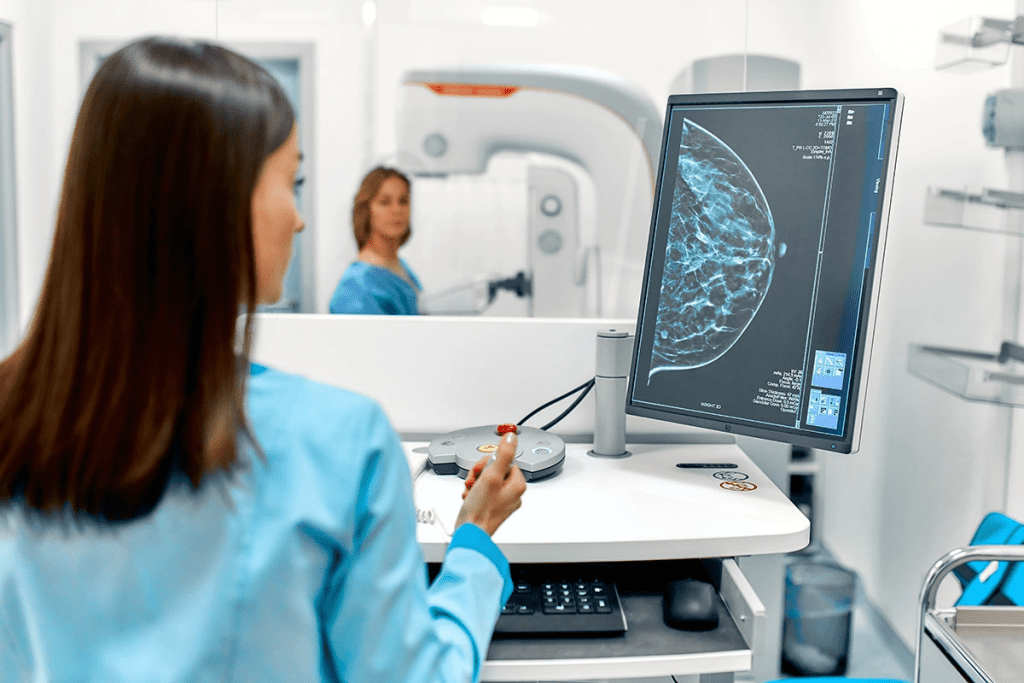
Importance of Lymph Node Evaluation in Bladder Cancer
Checking lymph nodes is key in bladder cancer for a few reasons. It helps in accurate staging, which is important for knowing what to expect. It also guides treatment choices, like whether to use chemotherapy or surgery. A detailed check can spot patients at higher risk, leading to better treatment plans.
The guideline stresses the need for lymph node checks in bladder cancer. It shows how important they are for making treatment plans and improving patient results. Knowing how cancer spreads and the role of lymph nodes helps doctors create better treatment strategies.
Treatment Options for Bladder Cancer Based on Lymph Node Status
Lymph node status is key in choosing the right treatment for bladder cancer. If cancer is found in the lymph nodes, treatments may be more aggressive. This could mean surgery instead of less invasive options.
Non-invasive treatment approaches
For those with no cancer in the lymph nodes, non-invasive treatments might be an option. These include intravesical therapy and immunotherapy. Intravesical therapy involves putting medicine directly into the bladder. Immunotherapy boosts the body’s immune system to fight cancer.
Intravesical therapy is often used for early-stage bladder cancer. It helps lower the chance of cancer coming back. Immunotherapy, like Bacillus Calmette-Guérin (BCG), works by making the body’s immune system attack cancer cells.
When surgery becomes necessary
If lymph nodes have cancer or the cancer is advanced, surgery is often needed. Radical cystectomy, or removing the bladder, is a common surgery for muscle-invasive bladder cancer. This surgery takes out the bladder and sometimes nearby organs, depending on the cancer’s spread.
Chemotherapy or radiation therapy might be added to surgery for better cancer treatment. The choice to have surgery depends on many things. These include the cancer’s stage, the patient’s health, and what they prefer.
It’s important for bladder cancer patients to know about treatment options based on lymph node status. By looking at both non-invasive and surgical treatments, patients can make better choices. They can do this with the help of their healthcare team.
Can You Live Without Bladder?
Some bladder cancer patients live without a bladder. This is a big change for their health. The bladder is key to the urinary system. Removing it, called cystectomy, is a big surgery.
The Essential Functions of the Bladder
The bladder holds urine made by the kidneys. It’s important for storing urine until we go to the bathroom. The bladder can stretch to hold more urine, which is vital for us.
Key functions of the bladder include:
- Storing urine
- Regulating the flow of urine
- Signaling the need to urinate
How the Body Adapts After Bladder Removal
After a cystectomy, the body finds new ways to handle urine. There are different ways to manage urine, like an ileal conduit or a neobladder.
Life without a bladder means big changes. Patients must learn to care for their new system. This includes managing a stoma or using a new bladder.
It’s important for patients to understand these changes. Knowing about urinary diversion helps them make choices. It prepares them for the life changes they will face.
Radical Cystectomy: The Bladder Removal Procedure
Radical cystectomy is a complex surgery for bladder removal. It’s for those with invasive bladder cancer or severe bladder issues. This surgery needs careful planning and thought.
What the Surgery Entails
During radical cystectomy, the bladder, lymph nodes, and sometimes other organs are removed. Men might lose the prostate and seminal vesicles. Women could lose the uterus, ovaries, and part of the vagina.
The surgery is done under general anesthesia and can last several hours. The surgeon might choose an open surgery or a minimally invasive method. This depends on the patient’s health and the surgeon’s skills.
The procedure involves several key steps:
- Making an incision in the abdomen to access the bladder
- Carefully dissecting the bladder from surrounding tissues and organs
- Removing the bladder and potentially other affected organs
- Creating a new way for urine to exit the body, known as urinary diversion
Candidates for Bladder Removal
Those with muscle-invasive bladder cancer or high-risk non-muscle invasive cancer are candidates. Also, people with severe bladder dysfunction or damage might need this surgery.
The choice to have radical cystectomy depends on many factors. These include the patient’s health, cancer stage and grade, and personal wishes.
It’s vital for patients to talk about their options with their healthcare team. They need to understand the surgery’s benefits and risks.
Urinary Diversion Options After Bladder Removal
Urinary diversion is key after bladder removal surgery. It gives patients several choices. The body needs a new way to handle urine after a radical cystectomy.
The right choice depends on health, lifestyle, and personal wishes. There are three main options: ileal conduit diversion, neobladder reconstruction, and continent urinary reservoir.
Ileal Conduit Diversion
Ileal conduit diversion is a common choice. It uses a piece of intestine to make a conduit. This conduit connects to the ureters, letting urine flow out.
The conduit is placed on the abdomen’s surface. A pouch or bag is attached to collect urine.
Neobladder Reconstruction
Neobladder reconstruction makes a new bladder from intestine. It connects to the urethra for natural urination.
Not everyone can have a neobladder. Health, cancer extent, and surgeon skill matter in choosing this option.
Continent Urinary Reservoir
A continent urinary reservoir is a pouch inside the body. It stores urine, which is drained with a catheter.
This method needs regular catheter use. It’s an alternative to wearing an external pouch.
Each method has its pros and cons. Patients should talk to their healthcare provider to find the best choice for them.
- Ideal Conduit: Simple and quick, but needs an external pouch.
- Neobladder: Offers natural voiding, but may need more surgeries and has specific criteria.
- Continent Reservoir: Stores urine internally, but requires regular catheter use.
Physical Adjustments to Life Without a Bladder
Living without a bladder means big changes. After surgery, you’ll need to learn new ways to handle urine.
Immediate Recovery Period
The first days after surgery are key. You might feel pain, discomfort, and swelling in your belly. Effective pain management is key during this time. Doctors often give medicine to help with pain.
You might find it hard to move around or do everyday tasks. It’s important to watch for signs of infection or other problems.
Long-term Physical Adaptations
Over time, you’ll get used to new ways of dealing with urine. This could mean learning about ileal conduits or neobladders. Proper stoma care is vital for those with an ileal conduit to avoid issues.
Exercising can boost your health and lower the chance of problems. It’s important to stick to a personalized recovery plan made just for you.
Psychological Impact of Bladder Removal
The psychological effects of bladder removal are very important. This surgery can deeply affect a person’s mental and emotional health.
Patients might feel many emotions after surgery, like relief, anxiety, or sadness. It’s key to understand these feelings to help them fully.
Body Image Concerns
Body image issues are a big challenge for patients after bladder removal. Changes in how they urinate and scars can change how they see themselves.
Support from doctors, family, and groups can help. Counseling and therapy are also important for adjusting to these changes.
Body Image Concerns After Bladder Removal
| Concerns | Potential Impact | Support Measures |
| Urinary diversion changes | Altered self-perception | Counseling, support groups |
| Scarring | Emotional distress | Psychological therapy |
| Loss of bladder control | Anxiety, depression | Medical support, lifestyle adjustments |
Sexual Function Changes
Sexual function changes are also a big part of the psychological impact. Patients might see changes in sexual desire or have trouble with erections.
These changes can be hard to deal with and affect their life quality. It’s important for doctors to talk about these issues and offer help.
“The impact of bladder removal on sexual function can be significant, and it’s essential that patients receive complete support to address these changes.”
Understanding and helping with the psychological effects of bladder removal is key. This includes body image and sexual function changes. Healthcare providers can give better care by focusing on these areas.
Quality of Life After Bladder Removal Surgery
After bladder removal surgery, patients and doctors worry about the quality of life. This surgery, or radical cystectomy, is often needed for bladder cancer. It’s a big deal.
Patients face big challenges, both physically and emotionally. Knowing these challenges helps manage expectations and improve care after surgery.
Research Findings on Post-Surgery Quality of Life
Many studies have looked into life after bladder removal surgery. They show that while it changes a lot, many people adjust well.
A study in the Journal of Urology found that patients get better over time. They face challenges at first but then see improvements in their quality of life.
“The quality of life after radical cystectomy is influenced by multiple factors, including the type of urinary diversion used and the patient’s overall health.”
– Journal of Urology
Factors That Influence Adjustment
Several things affect how well a patient adjusts after bladder removal surgery. These include the type of urinary diversion, age, health, and support system.
- Type of urinary diversion: Ileal conduit, neobladder, or continent urinary reservoir.
- Patient’s overall health and presence of comorbidities.
- Support from family, friends, and healthcare providers.
How long it takes to adjust varies a lot. Some people need more time, while others adjust faster.
| Factor | Influence on Quality of Life |
| Type of Urinary Diversion | Affects physical comfort and lifestyle adjustments. |
| Overall Health | Impacts recovery time and ability to adapt. |
| Support System | Provides emotional support and practical assistance. |
Bladder-Sparing Approaches: When Removal Can Be Avoided
Not all bladder cancer patients need to have their bladder removed. Thanks to new treatments, some can keep their bladder while fighting cancer.
Trimodal Therapy Options
Trimodal therapy is a new way to save the bladder. It uses transurethral resection of the bladder tumor (TURBT), radiation therapy, and chemotherapy. This method tries to kill the tumor without harming the bladder.
A study in a top medical journal says trimodal therapy is a good choice for some bladder cancer patients. It helps those who don’t want to give up their bladder.
Candidate Selection for Bladder Preservation
Choosing the right patients for bladder-saving treatments is key. Doctors look at the cancer’s stage and grade, the patient’s health, and what they want. A top oncologist says, “Finding the right patients for trimodal therapy is the secret to saving the bladder.”
Good candidates usually have early-stage cancer that responds well to treatment. A team of doctors will decide the best treatment plan for each patient.
Choosing bladder-sparing treatments can help patients avoid surgery’s side effects. As research grows, picking the right patients and treatments will get even better.
Making Treatment Decisions: Beyond Lymph Node Status
Choosing the right treatment for cancer involves many factors. It’s not just about the lymph nodes. Understanding these factors helps patients make informed choices.
Tumor Characteristics That Influence Treatment
The tumor’s features are key in picking the best treatment. Tumor size, grade, and histology are important to doctors when planning treatment.
- Tumor size affects if surgery is possible and if other treatments like chemo or radiation are needed.
- The tumor’s grade, or how much it looks like normal cells, guides how aggressive the treatment should be.
- Studying the tumor’s tissue, or histology, helps doctors understand the cancer type and how it might behave.
Patient Health and Preferences
A patient’s health and what they prefer also shape their treatment plan. Comorbidities, or existing health issues, can make some treatments harder to handle.
What the patient values and their goals are also important. Doctors talk about the good and bad of each treatment. They also consider how it might affect the patient’s life quality.
| Factor | Influence on Treatment |
| Tumor Size | Affects surgical feasibility and need for additional treatments |
| Tumor Grade | Influences treatment aggressiveness |
| Patient Comorbidities | Affects tolerance to certain treatments |
Discussing Treatment Options With Your Healthcare Team
Choosing cancer treatment means working closely with your healthcare providers. It’s important to talk openly to understand your treatment plan. This way, you can make choices that are best for you.
Questions to Ask About Chemotherapy
Thinking about chemotherapy? There are key questions to ask your healthcare team. Knowing the good and bad can help you decide.
- What are the goals of chemotherapy in my treatment plan?
- What are the possible side effects, and how can they be managed?
- How will chemotherapy affect my daily life and activities?
Knowing what to expect can lessen your worries. It helps you get ready for treatment.
Understanding Your Personalized Treatment Plan
Every person’s situation is different, and your treatment should match your needs. Your healthcare team will look at many things when making your plan.
| Factors Considered | Description |
| Cancer Type and Stage | The type and stage of cancer are key in choosing treatment. |
| Overall Health | Your health and any existing conditions are important in planning your treatment. |
| Personal Preferences | Your personal wishes and values are considered to make sure the treatment fits you. |
Knowing these factors and how they shape your treatment plan can make you feel more in charge of your care.
Conclusion
Lymph nodes are key in deciding if cancer patients need chemotherapy. It’s important to know the difference between clear and positive lymph nodes. This helps in making the right treatment choices.
Key points show how important lymph nodes are in cancer treatment. For bladder cancer, many things affect the need for chemotherapy. These include lymph node status, tumor details, and overall health.
It’s vital for patients to talk with their doctors about treatment options. They should consider their own treatment plan and any questions about chemotherapy or other treatments.
Understanding how lymph nodes affect treatment choices helps patients make better decisions. This can improve their quality of life and treatment results.
FAQ
What does it mean if my lymph nodes are clear?
Clear lymph nodes mean no cancer cells were found in the nodes checked. This suggests the cancer might not have spread to these areas.
Do I need chemotherapy if my lymph nodes are clear?
Whether you need chemotherapy depends on many things. These include the cancer type and stage, tumor details, and your overall health. Even with clear lymph nodes, chemotherapy might be needed based on your specific situation.
How does lymph node status affect cancer staging?
Lymph node status is key in cancer staging. It’s part of the TNM system, which looks at the tumor size, lymph node involvement, and metastasis.
Can bladder cancer be treated without removing the bladder?
Yes, some bladder cancer patients might not need a bladder removal. Treatments like trimodal therapy could be suitable, depending on the tumor’s stage and type.
What are the urinary diversion options after bladder removal?
After removing the bladder, you have several options. These include ileal conduit, neobladder reconstruction, and continent urinary reservoir. Each has its own benefits and considerations.
How does the body adapt after bladder removal?
The body adjusts to bladder removal through various urinary diversion methods. Patients may need to make lifestyle changes to manage their new urinary system.
What is the impact of bladder removal on quality of life?
Bladder removal can be challenging, but many patients adapt well. Their quality of life depends on their health and support systems.
What are the psychological effects of bladder removal?
Bladder removal can affect body image and sexual function. It’s important to have support and counseling to cope with these changes.
How do I discuss treatment options with my healthcare team?
It’s vital to ask questions about chemotherapy and understand your treatment plan. Discussing factors like tumor characteristics and your health is also important.
What are the treatment options for bladder cancer based on lymph node status?
Treatment for bladder cancer varies based on lymph node status. Options include non-invasive methods and surgery, depending on cancer spread.
Can I live without a bladder, and what are the alternatives for bladder function?
Yes, living without a bladder is possible. Urinary diversion options provide alternatives for bladder function, helping patients adapt to life after removal.
What is radical cystectomy, and who is a candidate for bladder removal?
Radical cystectomy is the removal of the bladder. It’s for patients with bladder cancer or other conditions requiring bladder removal.
Reference
- Witjes, J. A., Bruins, H. M., Cathomas, R., Compérat, E. M., Cowan, N. C., Gakis, G., … & Ribal, M. J. (2021). European Association of Urology Guidelines on Muscle-invasive and Metastatic Bladder Cancer: Summary of the 2020 Guidelines. European Urology, 79(1), 82“104. https://pubmed.ncbi.nlm.nih.gov/32919981/