Types of blood disease
Did you know that hematology-oncology diseases affect the blood and bone marrow of millions worldwide? Blood cancers like leukemia, lymphoma, and multiple myeloma are just a few examples. These complex disorders are treated by hematologist-oncologists.
We will explore hematology-oncology diseases and various blood disorders. Our aim is to offer top-notch information. We want to help international healthcare seekers find the best care.
Key Takeaways
- Knowing the different types of blood disease is key for good treatment.
- Hematologist-oncologists handle blood cancers and other non-malignant disorders.
- A detailed guide to hematology-oncology diseases helps find the right treatment.
- Learning about the blood disorders list helps spot symptoms and get medical help.
- Medical research keeps getting better, improving treatment for these diseases.
Understanding Hematology and Oncology

A detailed illustration showcasing the convergence of hematology and oncology disciplines. In the foreground, a medical professional examines a microscopic slide, their expression one of deep concentration. The middle ground depicts a 3D molecular model, representing the complex interplay of blood cells and cancer. In the background, a hospital ward comes into view, the hushed atmosphere conveying the gravity of these interconnected fields. Soft, directional lighting illuminates the scene, casting dramatic shadows and highlighting the intricate details. A sense of scientific inquiry and clinical precision permeates the composition, inviting the viewer to ponder the crucial intersection of hematology and oncology in the pursuit of understanding and treating blood-related malignancies.
Exploring blood diseases and cancer needs a deep look into hematology and oncology. These areas are key for diagnosing, treating, and managing blood and cancer issues.
What is Hematology?
Hematology deals with blood and blood-related disorders. It includes blood cells, vessels, lymph nodes, and bone marrow. Hematologists treat anemia, bleeding disorders, and blood cell diseases.
- Diagnosis: Uses tests like complete blood counts (CBC) and bone marrow biopsies.
- Treatment: Offers therapies like transfusions and medications for blood cell production.
- Management: Manages chronic blood conditions over time.
What is Oncology?
Oncology focuses on cancer study, diagnosis, treatment, and management. Oncologists handle various cancers, including blood cancers like leukemia and lymphoma.
- Prevention: Teaches cancer prevention.
- Diagnosis: Uses biopsies, imaging, and molecular testing.
- Treatment: Provides therapies like chemotherapy and targeted therapy.
The Intersection of Hematology and Oncology
Hematology and oncology overlap, especially in blood cancers. Hematologist-oncologists are experts in both, offering full care for blood-related cancers.
- Comprehensive Care: Manages complex cases with blood diseases and cancer.
- Advanced Treatment Options: Offers new therapies from both fields.
- Research and Development: Advances treatments through trials and studies.
Knowing about hematology and oncology helps patients and doctors tackle blood diseases and cancer. This leads to better diagnosis, treatment, and management.
The Blood System: Structure and Function
A detailed cross-section of the human blood system, showcasing its intricate components. A crisp, clean medical illustration, illuminated by soft, directional lighting that accentuates the various structures. In the foreground, red blood cells, white blood cells, and platelets flow through an arteriole and venule, their shapes and functions clearly visible. In the middle ground, the heart and its chambers are depicted, along with the aorta and major veins. In the background, the lymph nodes and spleen are shown, interconnected by a network of lymphatic vessels. The color palette is muted and anatomical, emphasizing the clinical nature of the subject matter. The overall mood is one of scientific precision and educational clarity.
It’s important to know how the blood system works. This system, also called the circulatory system, is key to our health. It helps keep us alive by moving nutrients and oxygen around.
Components of Blood
Blood has several important parts. Red blood cells carry oxygen. White blood cells help fight off infections. Platelets help blood to clot, and plasma carries everything around the body.
Blood Cell Production
Blood cells are made in the bone marrow. This is the soft tissue inside bones. The process of making blood cells is called hematopoiesis. It turns stem cells into different types of blood cells.
- Red blood cells are made through erythropoiesis.
- White blood cells are made through leukopoiesis.
- Platelets are made through thrombopoiesis.
The Role of Bone Marrow
The bone marrow is crucial for making blood cells. It turns stem cells into red blood cells, white blood cells, and platelets. It also gets rid of old or damaged red blood cells.
In short, the blood system is vital. It needs all its parts, including blood cells and bone marrow, to work right. Knowing how these parts work together helps us understand and treat blood disorders.
Types of Blood Disease: A Comprehensive Overview
A detailed anatomical illustration showcasing the different types of blood diseases, displayed in a clean, scientific manner. The foreground features a central diagram with labeled sections for various hematological conditions, including leukemia, lymphoma, anemia, and platelet disorders. The middle ground depicts stylized blood cells and cellular structures, rendered in a crisp, high-contrast style to emphasize the medical and diagnostic nature of the image. The background is a soft, neutral gradient, allowing the focal elements to stand out prominently. The lighting is even and diffused, creating a sense of clinical objectivity. The overall composition conveys a comprehensive, educational overview of blood disease classification, suitable for use in a hematology-oncology reference article.
Blood diseases cover a wide range, from non-malignant to malignant disorders. They can affect red blood cells, white blood cells, and platelets. Causes include genetics, environmental factors, and infections.
Non-Malignant vs. Malignant Blood Disorders
Blood disorders fall into two main categories: non-malignant and malignant. Non-malignant disorders are usually not life-threatening. Examples include anemia and bleeding disorders. Malignant blood diseases, however, are cancers like leukemia and lymphoma.
Key differences between non-malignant and malignant blood disorders:
- Non-malignant disorders are not cancerous and can often be treated with medication or lifestyle changes.
- Malignant disorders are cancerous and require treatments like chemotherapy and bone marrow transplantation.
Classification Systems
There are several ways to classify blood diseases. The World Health Organization (WHO) and the French-American-British (FAB) classification are two main systems. They help doctors diagnose and manage blood diseases by grouping them based on their characteristics.
Common classification systems for blood diseases:
- WHO classification: Used for categorizing hematological malignancies.
- FAB classification: Historically used for classifying acute myeloid leukemia (AML) and other myelodysplastic syndromes.
Prevalence and Demographics
The occurrence of blood diseases varies by condition, location, and demographic. Some diseases are more common in certain age groups or populations. For example, some leukemias are more common in children, while others affect adults more.
Knowing the prevalence and demographics of blood diseases is key for public health planning. It helps in allocating resources and raising awareness about these conditions.
Common Causes and Risk Factors for Blood Disorders
A detailed illustration of the key risk factors for blood disorders, presented in a clean, scientific style. In the foreground, a collection of medical icons and symbols representing common triggers such as genetics, lifestyle factors, infections, and exposure to toxins. The middle ground depicts a 3D model of a human circulatory system, highlighting vulnerable areas. The background features a subtle, muted color palette with a sense of clinical precision, creating an atmosphere of objective analysis. Soft, directional lighting casts a contemplative tone, inviting the viewer to study the interconnected elements that contribute to hematological conditions.
It’s important to know what causes blood disorders to catch them early. These disorders come from genetics, the environment, age, and lifestyle. We’ll look at each factor to understand the risks better.
Genetic and Hereditary Factors
Genetics play a big role in blood disorders. Some conditions, like sickle cell anemia and hemophilia, are passed down from parents. Genetic mutations can mess with blood cell production, causing disorders. For example, hemoglobinopathies happen when genes for hemoglobin are mutated.
People with a family history of blood disorders are at higher risk. Genetic counseling can help. New genetic tests help find risks early and start treatments sooner.
Environmental Exposures
Some environmental factors raise the risk of blood disorders. Toxic chemicals, radiation, and infections are among them. For instance, benzene, used in industries, can lead to leukemia.
- Radiation, from accidents or medical treatments, can harm bone marrow and cause blood disorders.
- HIV and some hepatitis viruses can affect the blood system, raising disorder risks.
- Pesticides and heavy metals are also linked to blood conditions.
Age-Related Factors
Age is a big risk factor for many blood disorders. Conditions like myelodysplastic syndromes and multiple myeloma are more common in older adults. This is because genetic damage builds up over time.
Children are also at risk, especially for acute lymphoblastic leukemia (ALL), the most common childhood cancer.
Lifestyle Influences
Lifestyle choices can affect blood disorder risks. Smoking and drinking too much alcohol can increase these risks. A healthy lifestyle, with a good diet and exercise, can help lower these risks.
- Staying away from harmful substances and following safety rules at work can prevent some blood disorders.
- Regular health checks and screenings can catch and manage blood disorders early.
Red Blood Cell Disorders
A dramatic close-up of red blood cells with visible genetic mutations and deformities, against a blurred backdrop of a hematology laboratory. The cells are rendered in vivid, saturated crimson hues, their irregular shapes and uneven surfaces highlighted by dramatic chiaroscuro lighting that casts long shadows. The overall effect is one of scientific intrigue and clinical precision, conveying the complexity and importance of understanding red blood cell disorders.
Red blood cell disorders affect how red blood cells are made, work, and last. They are key for carrying oxygen around the body. These issues can really change someone’s life, so finding the right treatment is very important.
Anemia and Its Various Forms
Anemia means not having enough healthy red blood cells. This makes it hard for the body to get enough oxygen. It can happen for many reasons, like not getting enough iron or vitamins.
Iron deficiency anemia is the most common type. It often comes from not eating enough iron, losing blood too much, or needing more iron when pregnant.
Other types include vitamin deficiency anemia from not having enough B12 or folate. And anemia of chronic disease happens with long-term illnesses like arthritis or cancer.
Polycythemia
Polycythemia means having too many red blood cells. This can make blood thicker and increase the risk of blood clots. Polycythemia vera is a rare blood cancer that makes too many red and white blood cells and platelets.
Hemoglobinopathies
Hemoglobinopathies are genetic problems with hemoglobin, the protein in red blood cells. Sickle cell disease and thalassemia are well-known examples. Sickle cell disease makes red blood cells look like sickles, while thalassemia means not enough hemoglobin.
“Understanding the genetic basis of hemoglobinopathies is crucial for diagnosis and management, allowing for early intervention and improved patient outcomes.”
In summary, red blood cell disorders are complex and need careful handling. Knowing the causes, signs, and treatments helps doctors give better care. This can greatly improve how patients feel and live.
White Blood Cell Disorders
A microscopic view of white blood cells in various states of disorder, illuminated by a soft, diffused light. In the foreground, abnormally shaped and sized cells, with irregular nuclei and cytoplasmic inclusions, convey the disrupted cellular architecture. The middle ground features clusters of white cells in diverse stages of activation and deformation, hinting at the dysregulated immune response. The background presents a subtle, hazy landscape of cellular components, highlighting the complex, intricate nature of hematological disorders.
White blood cells are key to our immune system. Problems with these cells can cause health issues. They help fight off infections and invaders.
Neutropenia
Neutropenia means you have too few neutrophils, a type of white blood cell. Severe neutropenia makes it hard to fight infections.
It can happen due to chemotherapy, some medicines, or bone marrow issues. Treatment aims to fix the cause and boost neutrophil numbers.
Leukocytosis
Leukocytosis is when you have too many white blood cells. It’s a normal response to infection or stress. But, persistent or severe leukocytosis might mean there’s a bigger issue.
It can be caused by infections, inflammation, or leukemia. Doctors use blood tests and other checks to find the cause.
Immunodeficiency Disorders
Immunodeficiency disorders happen when the immune system doesn’t work right. They make you more likely to get sick. Treatment depends on the type.
Examples include severe combined immunodeficiency (SCID) and conditions caused by HIV/AIDS or treatments that weaken the immune system.
| Condition | Description | Common Causes |
| Neutropenia | Low neutrophil count | Chemotherapy, certain medications, bone marrow disorders |
| Leukocytosis | High white blood cell count | Infections, inflammatory diseases, leukemia |
| Immunodeficiency Disorders | Impaired immune function | Primary immunodeficiencies, HIV/AIDS, immunosuppressive therapy |
It’s important to understand and manage white blood cell disorders. This helps keep our immune system strong and our health good.
Platelet and Clotting Disorders
In the foreground, a close-up view of abnormal platelet shapes and sizes, rendered in high-contrast, realistic detail. The middle ground depicts the process of clot formation, with platelets aggregating and interacting with other blood components. In the background, a schematic representation of the underlying cellular and molecular mechanisms responsible for platelet function and dysfunction. The color palette is muted, with shades of red, purple, and gray, conveying the seriousness and complexity of the subject matter. Soft, indirect lighting casts subtle shadows, enhancing the three-dimensional quality of the illustration. The overall composition is balanced and educational, designed to effectively communicate the key aspects of platelet disorders to a medical audience.
The blood’s clotting mechanism is key to stopping bleeding. Disorders in this system can be serious. These conditions affect how the body handles bleeding and clotting.
Thrombocytopenia
Thrombocytopenia means you have too few platelets. This can cause bleeding problems. Causes include bone marrow issues or some medicines. Symptoms include easy bruising and bleeding.
Thrombocytosis
Thrombocytosis is when you have too many platelets. This raises the risk of blood clots. Managing this condition is key to avoiding blood clots.
Hemophilia and Other Clotting Factor Deficiencies
Hemophilia is a genetic disorder that makes clotting hard. It’s needed to stop bleeding. Other clotting factor issues can also cause bleeding problems. Treatment often involves replacing the missing clotting factor.
Von Willebrand Disease
Von Willebrand disease is the most common hereditary coagulation abnormality. It affects the blood’s clotting ability. It’s caused by a lack or mutation of the von Willebrand factor.
| Condition | Description | Common Symptoms |
| Thrombocytopenia | Low platelet count | Bleeding, bruising |
| Thrombocytosis | High platelet count | Risk of blood clots |
| Hemophilia | Clotting factor deficiency | Prolonged bleeding |
| Von Willebrand Disease | Deficiency of von Willebrand factor | Bleeding, heavy menstrual periods |
Blood Cancers: Leukemias
Leukemia is a cancer that affects the blood cells. It’s a big deal in hematology-oncology. It happens when white blood cells, key for our immune system, grow abnormally.
Knowing the different types of leukemia is key. It helps doctors create the best treatment plans.
Acute Myeloid Leukemia (AML)
AML is a fast-growing leukemia that hits the myeloid cells in the bone marrow. It’s more common in adults and needs quick action. If not treated, AML can be very aggressive and hard to beat.
Acute Lymphoblastic Leukemia (ALL)
ALL is a fast-moving leukemia that attacks the lymphoid cells. It’s the top leukemia in kids but can also hit adults. Quick diagnosis and treatment are crucial to boost survival chances.
Chronic Myeloid Leukemia (CML)
CML grows slowly and affects the myeloid cells. It’s marked by the Philadelphia chromosome, a genetic swap. CML mostly affects adults and can be managed with special drugs.
Chronic Lymphocytic Leukemia (CLL)
CLL grows slowly and hits the lymphoid cells. It’s more common in older adults. It often needs watching rather than immediate treatment. CLL can stay silent for years, but regular check-ups are a must.
Diagnosing and treating leukemia involves many tests and treatments. Knowing the exact type of leukemia is vital for picking the right treatment.
| Type of Leukemia | Characteristics | Common Age Group | Typical Treatment Approach |
| Acute Myeloid Leukemia (AML) | Rapidly progressing, affects myeloid cells | Adults | Chemotherapy, targeted therapy |
| Acute Lymphoblastic Leukemia (ALL) | Aggressive, affects lymphoid cells | Children and adults | Chemotherapy, stem cell transplant |
| Chronic Myeloid Leukemia (CML) | Slowly progressing, affects myeloid cells | Adults | Targeted therapy |
| Chronic Lymphocytic Leukemia (CLL) | Slow-progressing, affects lymphoid cells | Older adults | Monitoring, chemotherapy, targeted therapy |
Leukemia treatment has made big strides, leading to better patient outcomes. By grasping the various leukemia types and their traits, doctors can tailor treatments. This approach improves patient care.
Blood Cancers: Lymphomas
Lymphomas are blood cancers that come in two types: Hodgkin and non-Hodgkin. Hodgkin lymphoma has Reed-Sternberg cells, while non-Hodgkin is more varied. These cancers start in lymphocytes, important white blood cells for our immune system.
Hodgkin Lymphoma
Hodgkin lymphoma is known for Reed-Sternberg cells, big abnormal lymphocytes. Symptoms include swollen lymph nodes in the neck or under the arms. You might also feel fever, night sweats, and lose weight.
To find out how far the disease has spread, we use a staging system. This helps decide the best treatment. Today, we mainly use chemotherapy and radiation. But, we’re also looking into new treatments to lessen side effects.
Non-Hodgkin Lymphoma
Non-Hodgkin lymphoma is a wide range of cancers without Reed-Sternberg cells. Symptoms are similar, like swollen lymph nodes. But, it behaves differently and has various types.
How we treat non-Hodgkin lymphoma depends on the type and how far it has spread. Some types need careful watching, while others need strong treatments. New treatments like targeted and immunotherapies are giving patients new hope.
In summary, lymphomas are complex blood cancers needing accurate diagnosis and specific treatments. Thanks to ongoing research and new therapies, we’re seeing better results for patients.
Blood Cancers: Multiple Myeloma and Related Disorders
Understanding multiple myeloma and related disorders is key to better treatment and care. These conditions can greatly affect patients’ lives. They need comprehensive care to manage their health.
Multiple Myeloma
Multiple myeloma is a cancer of plasma cells in the bone marrow. It causes abnormal proteins, leading to bone damage, anemia, and kidney problems.
Symptoms and Diagnosis: Symptoms include bone pain, tiredness, and frequent infections. Doctors use blood tests, bone marrow biopsies, and imaging to diagnose.
Treatment Approaches: Treatment has improved a lot. It includes targeted therapies, immunotherapy, and stem cell transplants. The right treatment depends on the patient’s health and disease details.
Waldenstrom Macroglobulinemia
Waldenstrom macroglobulinemia is a rare lymphoma. It causes too much IgM protein, leading to symptoms like dizziness and vision problems.
Clinical Features: Symptoms include anemia, tiredness, and swollen lymph nodes. Doctors diagnose it through blood tests and bone marrow biopsies.
Management Strategies: Treatment aims to reduce IgM levels. It includes chemotherapy, targeted therapy, and plasmapheresis to manage symptoms.
Amyloidosis
Amyloidosis is a condition where amyloid fibrils build up in tissues. In plasma cell dyscrasias, it happens when abnormal proteins from plasma cells accumulate in organs.
Clinical Manifestations: Symptoms depend on the organs affected. They can include kidney failure, heart problems, and nerve damage. Diagnosis involves tissue biopsies and amyloid characterization.
Treatment and Prognosis: Treatment aims to lower abnormal protein production. Chemotherapy and treatments targeting plasma cells can be effective. Prognosis depends on organ involvement and treatment response.
Myeloproliferative Neoplasms
Myeloproliferative neoplasms are conditions where blood cells grow too much. This can cause problems like blood clots and lead to worse diseases. We’ll look at the main types, their signs, and how to manage them.
Polycythemia Vera
Polycythemia vera makes too many red and white blood cells and platelets. It raises the risk of blood clots and can turn into more serious diseases.
Essential Thrombocythemia
Essential thrombocythemia means too many platelets. This can cause blood clots and other issues. The goal is to prevent clots and watch for disease growth.
Primary Myelofibrosis
Primary myelofibrosis scars the bone marrow. This leads to anemia, a big spleen, and other problems. Treatment aims to ease symptoms and improve life quality.
Chronic Neutrophilic Leukemia
Chronic neutrophilic leukemia makes too many neutrophils, a white blood cell type. It can cause infections and harm organs.
Diagnosing and treating myeloproliferative neoplasms needs a detailed plan. This includes blood tests, bone marrow biopsies, and genetic tests. Treatment depends on the disease type and the patient’s health.
| Disease | Key Characteristics | Common Complications |
| Polycythemia Vera | Overproduction of red blood cells, white blood cells, and platelets | Blood clots, disease progression |
| Essential Thrombocythemia | Overproduction of platelets | Thrombosis, bleeding |
| Primary Myelofibrosis | Scarring of the bone marrow | Anemia, splenomegaly |
| Chronic Neutrophilic Leukemia | Overproduction of neutrophils | Infections, organ damage |
Myelodysplastic Syndromes
Myelodysplastic syndromes are a group of blood disorders. They make it hard for the body to make myeloid blood cells. This can cause anemia, infections, and bleeding problems. Knowing about MDS is key for early diagnosis and treatment.
Classification of MDS
The way we classify myelodysplastic syndromes has changed over time. The World Health Organization (WHO) system is widely used. It sorts MDS based on cell shape, genetic changes, and the number of blasts in the blood and bone marrow.
The WHO system helps doctors understand how serious MDS is. It also guides treatment choices. It includes types like MDS with single lineage dysplasia and MDS with excess blasts.
Risk Factors and Causes
Knowing the risk factors for MDS is important. Exposure to chemicals like benzene and past treatments with chemotherapy or radiation are risks. Age is also a big factor, with MDS more common in older people.
Genetics can also play a part in MDS. Some people may be more likely to get MDS because of their genes. But often, the exact cause is not known.
Treatment Approaches
Treatment for myelodysplastic syndromes depends on many things. It includes supportive care like blood transfusions and more aggressive treatments like immunosuppressive therapy and hypomethylating agents.
For some high-risk MDS patients, a stem cell transplant might be an option. This could be a cure. Researchers are always looking for new ways to help MDS patients.
Diagnostic Approaches in Hematology-Oncology
Diagnosing blood diseases involves several steps. We use blood tests, bone marrow exams, and imaging studies. These methods help us accurately diagnose and manage blood disorders.
Blood Tests and Complete Blood Count
Blood tests are key in diagnosing blood diseases. A Complete Blood Count (CBC) is a common test. It shows details about blood components like red and white cells and platelets.
A CBC can spot issues like anemia, infection, and leukemia. For example, low red blood cells might mean anemia. High white blood cells could point to infection or leukemia.
| Component | Normal Range | Abnormal Indication |
| Red Blood Cells | 4.32-5.72 million cells/μL | Anemia or Polycythemia |
| White Blood Cells | 3.5-12.5 thousand cells/μL | Infection, Leukemia, or Leukopenia |
| Platelets | 150-450 thousand cells/μL | Thrombocytopenia or Thrombocytosis |
Bone Marrow Biopsy and Aspiration
Bone marrow biopsy and aspiration are vital for diagnosing blood disorders. These procedures remove a bone marrow sample for examination.
They help us see the marrow’s structure and cell content. This gives a full view of the marrow’s health, aiding in diagnosis and monitoring.
Molecular and Genetic Testing
Molecular and genetic testing are crucial in diagnosing and managing blood diseases. These tests find genetic mutations linked to blood disorders.
For instance, genetic testing can spot the BCR-ABL fusion gene in CML patients. This helps us create specific treatment plans based on the disease’s genetic makeup.
Imaging Studies
Imaging studies like X-rays, CT scans, MRI, and PET scans help us see disease extent and treatment response. They show us how lymph nodes, organs, and tissues are affected.
A PET scan can pinpoint active disease areas in lymphoma patients. This guides our treatment choices.
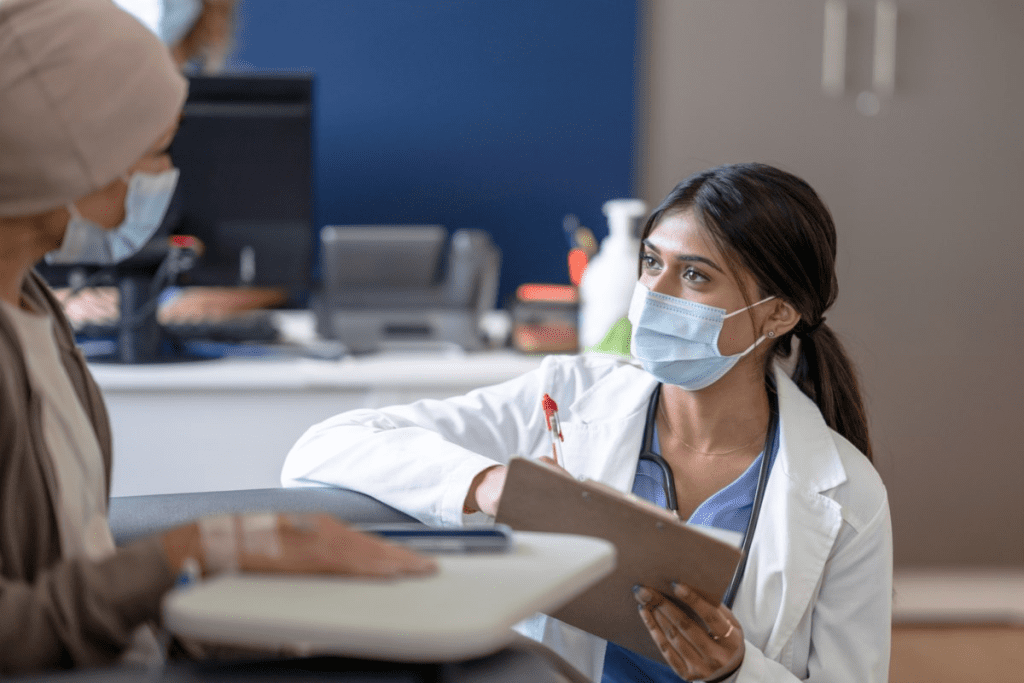
When to See a Hematologist or Oncologist
Knowing when to see a hematologist or oncologist is key, especially if you have a family history of blood disorders. These doctors are vital in diagnosing and treating blood diseases. This includes anemia, bleeding disorders, and blood cancers like leukemia and lymphoma.
Warning Signs and Symptoms
Some symptoms mean you should see a hematologist or oncologist. These include:
- Persistent fatigue or weakness
- Unexplained bruising or bleeding
- Frequent infections
- Swollen lymph nodes
- Unexplained weight loss
If you notice any of these signs, talk to your primary care doctor. They might send you to a specialist.
Screening Recommendations
Screening for blood disorders is important, especially if you have a family history or risk factors. Screening tests might include a complete blood count (CBC), blood smear, or genetic tests. Talk to your healthcare provider about your risk to figure out when to get screened.
Referral Process
The referral process starts with your primary care doctor. If they think you might have a blood disorder, they’ll send you to a hematologist or oncologist. It’s important to follow up on this referral to get timely care.
What to Expect at Your Appointment
At your first visit, expect a thorough check-up. This includes:
- A detailed medical history
- Physical examination
- Review of previous test results
- Discussion of symptoms and concerns
Depending on your condition, you might need more diagnostic tests. This could be bone marrow biopsies or imaging studies. We’re here to support you through this process with care and understanding.
Seeing a hematologist or oncologist early can make a big difference. By knowing when to seek specialized care, you’re taking a big step in managing your health.
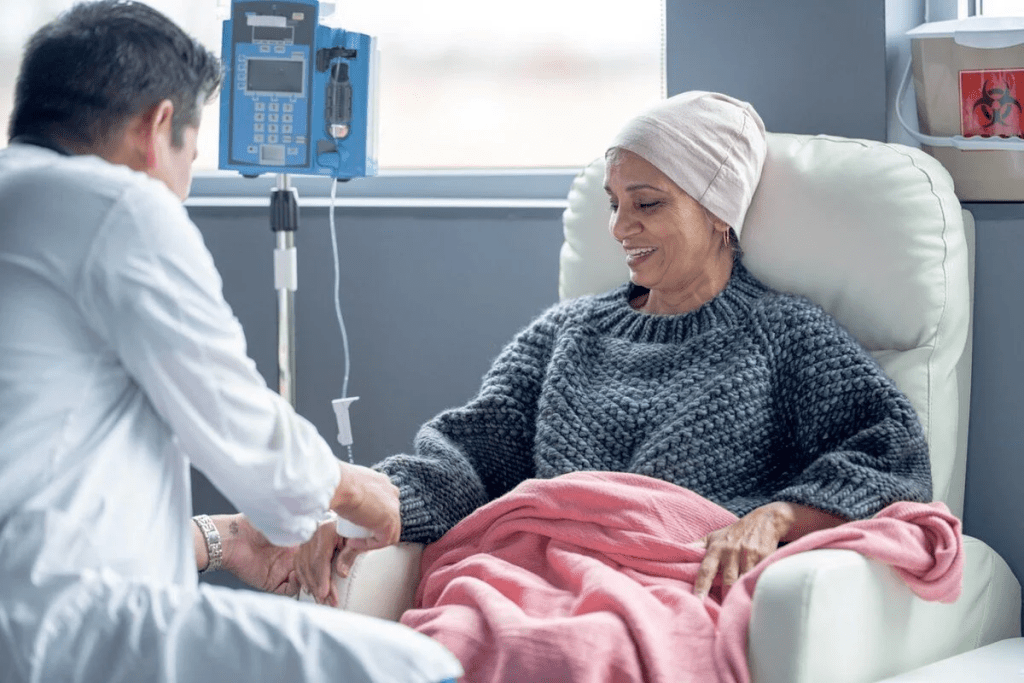
Treatment Modalities for Blood Disorders
Medical science has made big strides in treating blood disorders. Now, we have many ways to help patients, each one fitting a specific need.
Chemotherapy
Chemotherapy is key in fighting blood cancers and disorders. It uses drugs to kill or slow cancer cells. Chemotherapy can be taken by mouth or through an IV, based on the drug and treatment plan.
Choosing the right chemotherapy depends on the disease type, stage, and patient health. We often mix chemotherapy with other treatments to make it work better.
Radiation Therapy
Radiation therapy is vital for some blood disorders, especially those affecting the lymphatic system or bone marrow. It uses high-energy rays to kill or slow cancer cells. Radiation therapy can target specific areas, protecting healthy tissues.
We use different types of radiation therapy, like external beam and systemic. The choice depends on the disease’s nature and spread.
Targeted Therapies
Targeted therapies are a precise way to treat blood disorders. They use drugs that target cancer cells or molecules involved in cancer growth. Targeted therapies are often more effective and have fewer side effects than traditional chemotherapy.
Examples include tyrosine kinase inhibitors and monoclonal antibodies. As we learn more about blood disorders, we’re developing new targeted therapies.
Immunotherapy
Immunotherapy uses the immune system to fight blood cancers and disorders. It involves drugs that boost the immune system’s ability to attack cancer cells. Immunotherapy has shown great promise in treating some blood cancers, offering hope to patients.
Immunotherapy includes checkpoint inhibitors, CAR-T cell therapy, and cancer vaccines. We’re always looking for new ways to improve immunotherapy for blood disorders.
In conclusion, treating blood disorders is complex and involves many approaches. We choose the best treatment based on the patient’s condition and health. Knowing the different treatment options helps patients and doctors make the best decisions.
Living with Blood Disorders: Management and Support
Living with a blood disorder means you need to tackle it from many angles. This includes medical care, making lifestyle changes, and getting emotional support. By doing these things well, you can really improve your life.
Symptom Management
Handling symptoms is key when you have a blood disorder. You’ll need to use medicine and make lifestyle changes. For example, if you have anemia, you might take iron pills and eat certain foods to boost your red blood cells.
Keeping an eye on your treatment is also important. Going to regular doctor visits helps you see if your treatment is working. If not, you can change it to better fit your needs.
Nutritional Considerations
What you eat is very important when you have a blood disorder. Eating right can help lessen symptoms and keep you healthy. For instance, people with some blood cancers might need to eat a special diet to avoid getting sick.
- Eat a variety of fruits and veggies
- Include lean proteins and whole grains
- Stay away from foods that make symptoms worse
Psychological Support
Having a blood disorder can really affect your mind. Getting emotional support from loved ones, friends, and groups can help a lot. Also, talking to a therapist can be very helpful.
Groups that help patients with blood disorders are full of useful info. They offer support, the latest treatment news, and help you find others who understand what you’re going through. Connecting with others can be very empowering.
Patient Advocacy and Resources
Being an advocate for yourself is very important when you have a blood disorder. Advocacy groups can guide you through the healthcare system. They can help you find new treatments and support networks.
We suggest looking for these resources to improve your care and support. By doing so, you can manage your condition better and feel better overall.
Conclusion
It’s important to know about hematology-oncology diseases to help those affected. We’ve looked at different blood disorders, their causes, and how to diagnose them. This knowledge is key to giving good care.
Managing blood disorders needs a team effort. Hematologists, oncologists, and others work together. This teamwork helps patients get better and live better lives.
Good care for these diseases does more than just treat the illness. It also looks at the patient’s physical, emotional, and social needs. We must keep learning to give the best care possible.
FAQ
What is hematology-oncology?
Hematology-oncology is a medical field. It focuses on blood diseases and cancers. This includes issues with blood cells, bone marrow, and the lymphatic system.
What are the main types of blood cancers?
Blood cancers include leukemias, lymphomas, and multiple myeloma. Leukemias affect white blood cells. Lymphomas target the lymphatic system. Multiple myeloma impacts plasma cells in the bone marrow.
What are the symptoms of blood disorders?
Symptoms vary by condition. Common signs are fatigue, weakness, and pale skin. Other symptoms include shortness of breath, frequent infections, and easy bleeding or bruising.
How are blood diseases diagnosed?
Doctors use blood tests, bone marrow biopsies, and imaging studies to diagnose. A complete blood count (CBC) is often the first step.
What are the treatment options for blood cancers?
Treatments include chemotherapy, radiation, and targeted therapies. Immunotherapy and bone marrow transplantation are also options. The right treatment depends on the cancer type, stage, and patient health.
Can blood disorders be prevented?
Some disorders can’t be prevented, but risk factors can be managed. Avoid toxins, eat well, and manage stress. Genetic counseling helps those with a family history.
How can I manage symptoms of a blood disorder?
Managing symptoms involves medical treatment and lifestyle changes. Nutritional counseling, pain management, and psychological support improve quality of life.
When should I see a hematologist or oncologist?
See a specialist if you have symptoms or a diagnosis. Your primary care doctor can refer you.
What is the role of a hematologist-oncologist?
Hematologists-oncologists diagnose and treat blood diseases and cancers. They provide comprehensive care, including treatments and supportive care.
Are there support resources available for patients with blood disorders?
Yes, many resources are available. These include patient advocacy groups, support groups, and online resources. They offer information, emotional support, and connections to others.
References
- Cambridge University Hospitals NHS Foundation Trust. (n.d.). Bladder care and management. Retrieved October 7, 2025, from https://www.cuh.nhs.uk/patient-information/bladder-care-and-management/
- Atkinson, M. (2020, September 10). What are blood disorders? Medical News Today. Retrieved October 7, 2025, from https://www.medicalnewstoday.com/articles/316706
- National Center for Biotechnology Information. (2010). Disorders of hemostasis and thrombosis. Hematology/Oncology Clinics of North America, 24(4), 865-889. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2852629/








