Last Updated on October 21, 2025 by mcelik
People with Autoimmune Hemolytic Anemia (AIHA) worry about it coming back. Studies show that relapse rates can be high. This affects how well they manage the condition over time.Worried about an autoimmune hemolytic anemia relapse? Our best guide offers powerful strategies and essential tips for preventing a critical recurrence
Managing AIHA involves not only treatment but also preparing for the possibility of relapse. This condition makes the immune system attack red blood cells. It’s tough for both patients and doctors.
Knowing why AIHA relapse happens is key to better care. By diving into this condition’s details, we can help those affected more.
AIHA happens when the body makes antibodies against its own red blood cells. This leads to their early destruction. It’s important to know how it works, its types, symptoms, and how to diagnose it.
AIHA occurs when the immune system can’t tell the difference between its own red blood cells and invaders. It makes antibodies that mark these cells for destruction. This complex process involves immune cells and red blood cells, causing them to break down.
Key aspects of AIHA pathophysiology include:
AIHA is divided into two types based on when the antibodies work best: Warm AIHA and Cold AIHA.
| Type | Characteristics |
| Warm AIHA | Autoantibodies are most active at body temperature; often associated with other autoimmune diseases or lymphoproliferative disorders. |
| Cold AIHA | Autoantibodies are most active at cold temperatures; can be associated with infections or malignancies. |
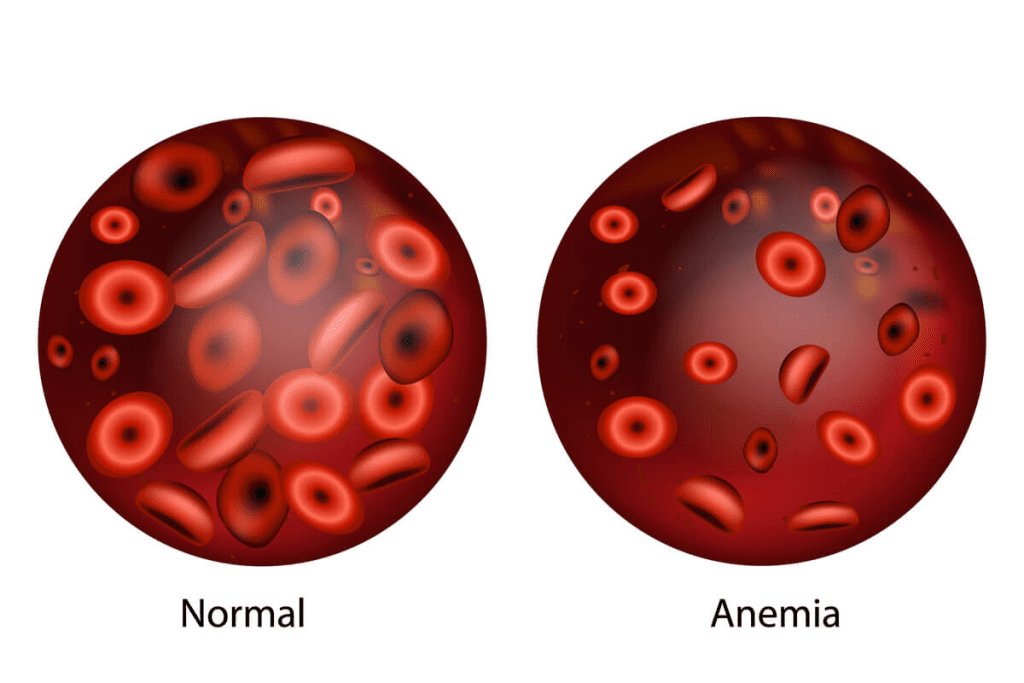
Symptoms of AIHA include fatigue, jaundice, and shortness of breath. These are signs of anemia. Doctors use tests like the direct Coombs test, Complete Blood Count (CBC), and reticulocyte count to diagnose it.
Diagnostic Approaches:
Knowing about AIHA helps doctors manage it better. This improves the lives of those with the condition.
Remission, whether complete or partial, is a key goal in treating AIHA. It means a big reduction or stop in hemolysis. This leads to better health and quality of life for patients.
In AIHA, there are two types of remission: complete and partial. Complete remission means hemoglobin levels are normal and there’s no hemolysis. Partial remission shows a big improvement in hemoglobin but not to complete normal levels.
“The difference between complete and partial remission is very important,” says a leading expert in hematology. “It helps decide treatment and predict the future of the disease.”
Doctors measure remission in AIHA by looking at several things. They check hemoglobin levels, reticulocyte count, LDH levels, and DAT results. These tests help see if treatment is working and if a patient is in remission.
The length of initial remission in AIHA varies a lot. It depends on the cause of AIHA, how well the treatment works, and the patient’s health. People with complete remission usually stay in remission longer than those with partial remission.
Understanding remission in AIHA helps patients and doctors make better treatment plans. By watching for signs of remission and keeping track of the disease, we can better manage AIHA. This leads to better results for patients.
Relapse in AIHA can happen at any time. It’s key to know the patterns of recurrence. Autoimmune Hemolytic Anemia makes the immune system attack red blood cells, causing them to break down early. The rate of relapse differs among AIHA types, and knowing these patterns is vital for managing the condition.
AIHA is divided into warm and cold types, each with its own relapse patterns. Warm AIHA, which makes up about 75% of cases, has a more variable relapse rate than cold AIHA. Research shows that warm AIHA relapse rates can be between 20% and 50% in the first few years after treatment.
Cold AIHA, however, tends to follow a more predictable path. Its relapse rate is generally lower, ranging from 10% to 30%. This is often triggered by cold temperatures.
The time when relapses are most likely to happen varies among AIHA patients. The biggest risk is usually within the first two years after diagnosis and treatment. Yet, relapses can happen even years after being in remission, showing the need for ongoing monitoring.
Looking at statistical patterns in AIHA recurrence helps find predictors of relapse. The cause of AIHA, how well it responds to treatment, and any underlying medical conditions are key factors. For example, those with secondary AIHA due to lymphoproliferative disorders might face a higher risk of relapse than those with primary AIHA.
Healthcare providers can create more effective treatment plans and follow-up strategies by understanding these patterns. This approach can help lower the risk of relapse and improve long-term results.
It’s important for patients and doctors to know the signs of AIHA relapse. Spotting these signs early can help manage the condition better. This can make the relapse less severe.
The signs of AIHA relapse are similar to the first time you were diagnosed. Look out for more fatigue, jaundice, and dark urine. It’s key to tell your doctor about these symptoms right away.
Common early warning symptoms include:

Lab tests are vital in spotting AIHA relapse. Look for lower hemoglobin levels, higher lactate dehydrogenase (LDH), and a positive direct Coombs test.
| Laboratory Test | Indicator of AIHA Relapse |
| Hemoglobin (Hb) | Decreasing levels |
| Lactate Dehydrogenase (LDH) | Increasing levels |
| Direct Coombs Test | Positive result |
| Bilirubin | Elevated levels, particularly indirect bilirubin |
Telling AIHA relapse apart from other similar symptoms is key. A thorough check-up, including your medical history and lab tests, is needed.
Key factors to consider when differentiating AIHA relapse include:
Understanding these points helps doctors diagnose AIHA relapse correctly. This leads to the right treatment.
Several risk factors can make AIHA more likely to come back. It’s important to know these factors to manage the condition better. This helps improve patient outcomes.
Certain health conditions can raise the risk of AIHA coming back. For example, people with chronic diseases or other autoimmune disorders might face a higher risk. We’ll look into how these conditions affect AIHA management.
Genetics play a big role in who gets AIHA and how often it comes back. If you have a family history of autoimmune diseases, you might be more likely to experience relapses. Knowing your genetic predispositions helps doctors tailor your treatment.
Some environmental factors, like certain chemicals or infections, can trigger AIHA relapses. It’s key to find and avoid these triggers to manage the condition.
Some medications can increase the risk of AIHA relapse. Certain drugs can cause hemolysis or affect the immune system, leading to a relapse. It’s crucial to manage medications carefully to reduce this risk.
The first treatment for Autoimmune Hemolytic Anemia (AIHA) is key to avoiding relapse. We’ll look at how the initial treatment choice and length can affect the chance of it coming back.
Choosing the right first treatment for AIHA is vital to stop it from coming back. Corticosteroids are often the first choice, but not everyone responds well. Some might need rituximab or splenectomy to stay in remission.
| Therapy | Relapse Rate | Duration of Remission |
| Corticosteroids | 40-60% | Variable |
| Rituximab | 20-40% | 1-3 years |
| Splenectomy | 10-30% | Long-term |
The length of the first treatment also matters for avoiding AIHA relapse. Prolonged treatment might be needed for some to stay in remission. We adjust treatment length based on how each patient responds.
How well a patient responds to the first treatment is a big clue for relapse risk. Complete responders face a lower risk than partial responders or those who don’t respond at all. We keep a close eye on how patients react to treatment to adjust their care plans.
Understanding how initial treatment affects AIHA relapse helps us find better ways to manage it. This leads to better outcomes for our patients.
Using steroids to treat AIHA can work at first. But, knowing about relapse after stopping steroids is key. When steroids don’t work or stop working, finding new treatments is needed.
There are many reasons for relapse after steroid treatment. These include how severe AIHA is, how fast steroids are tapered, and how each person reacts. Research shows many patients relapse within a year after stopping steroids.
| Timeframe | Relapse Rate |
| 0-6 months | 30% |
| 6-12 months | 20% |
| 1-2 years | 15% |
For AIHA that doesn’t respond to steroids, looking into other treatments is important. Using drugs that calm down the immune system can help. This way, the immune system doesn’t attack red blood cells as much.
When steroids don’t work, looking into other treatments is crucial. Removing the spleen can be a good option for some. This is because the spleen is where red blood cells are often destroyed.
“The decision to proceed with splenectomy should be made on a case-by-case basis, considering the patient’s overall health and potential risks.” – Hematologist
In summary, managing AIHA after steroid treatment needs a detailed plan. This includes understanding relapse patterns, dealing with steroid resistance, and trying new treatments. With a tailored approach, patients can manage their condition better and live a fuller life.
Rituximab is a promising treatment for AIHA, helping to manage the condition and prevent relapse. It targets CD20-positive B cells, reducing autoantibody production. This makes it a valuable option for AIHA treatment.
Research shows rituximab can lower the risk of AIHA relapse in some patients. It works by reducing B cells, which in turn lowers autoantibody production. The effectiveness of rituximab in preventing AIHA recurrence has been confirmed in several studies.
The time it takes for a relapse after rituximab varies. Some patients stay in remission for a long time, while others relapse sooner. Monitoring patients closely after treatment is key to catching relapse early.
When patients relapse after rituximab, re-treatment is an option. The decision to re-treat depends on how well the patient responded to the first treatment and the severity of the relapse. Re-treatment with rituximab can be effective, but it must be carefully considered.
We suggest that patients and healthcare providers talk about the benefits and risks of rituximab treatment and re-treatment for AIHA.
Splenectomy is a key treatment for Autoimmune Hemolytic Anemia (AIHA). It offers a chance for long-term control. We will look at how this surgery impacts AIHA management, focusing on its success, advantages, and downsides.
Research shows splenectomy can lower AIHA relapse rates. Some studies find the relapse rate after splenectomy is as low as 20%. But, this rate can change based on the AIHA type and patient selection.
Splenectomy works by removing the spleen, a main area for red blood cell destruction. This removal can improve hemoglobin levels and reduce hemolysis.
The good things about splenectomy for recurrent AIHA are:
But, there are also risks:
Choosing the right patients for splenectomy is key. Criteria include AIHA severity, response to treatments, and surgery risks. A hematologist must carefully evaluate each patient.
It’s best to have a team of doctors, including hematologists and surgeons, to decide if splenectomy is right for each patient. This ensures the benefits outweigh the risks.
Secondary AIHA brings special challenges for managing relapse, especially with conditions like lymphoma or autoimmune diseases. It’s important to understand how these conditions affect AIHA relapse patterns.
Patients with lymphoma-associated AIHA face a tougher time due to their cancer. Treatment for lymphoma might help AIHA, but it can also cause relapses. It’s crucial to keep a close eye on these patients to manage their care well.
AIHA can be linked to autoimmune diseases like systemic lupus erythematosus (SLE). When AIHA comes back in these patients, it’s often because their autoimmune disease is active. Immunosuppression is often used to control both the AIHA and the autoimmune disease.
| Underlying Condition | Impact on AIHA Relapse | Management Strategy |
| Lymphoma | Influenced by lymphoma activity and treatment | Treatment of lymphoma, close monitoring |
| Autoimmune Diseases (e.g., SLE) | Linked to disease activity | Immunosuppression for both AIHA and underlying disease |
| Infections | Can trigger AIHA relapse | Prompt treatment of infections, potentially adjusting AIHA treatment |
Infections can cause AIHA relapse in people who are at risk. The body’s fight against infection can sometimes lead to autoantibodies against red blood cells. It’s key to prevent infections through vaccines and quick treatment when they happen to manage AIHA.
Early detection of AIHA relapse needs a good monitoring plan. We suggest a plan that includes regular check-ups, important lab tests, and teaching patients how to monitor themselves.
It’s key to have a regular check-up schedule for AIHA patients. How often you need to visit depends on your health and past relapses.
At these visits, your doctor will check how you’re doing, look at lab results, and change your treatment if needed.
Lab tests are crucial for watching AIHA and catching early signs of relapse. Here are some tests often used:
| Laboratory Test | Purpose |
| Complete Blood Count (CBC) | Checks hemoglobin levels, red blood cell count, and other blood stuff. |
| Direct Antiglobulin Test (DAT) | Finds antibodies or complement proteins on red blood cells. |
| Reticulocyte Count | Looks at bone marrow activity and red blood cell making. |
| Lactate Dehydrogenase (LDH) | Checks for hemolysis by looking at LDH levels. |
These tests help doctors spot relapse early, so they can act fast.
Teaching patients how to monitor themselves is key for managing AIHA. They should know the signs of relapse, like:
Patients should keep a journal of their symptoms. This helps doctors make better treatment plans during visits.
As one patient said,
“Keeping a symptom journal has been a game-changer for me. It helps me remember important details to discuss with my doctor.”
Managing relapsed Autoimmune Hemolytic Anemia (AIHA) requires understanding different treatments. When AIHA comes back, we need to rethink the treatment plan. This ensures we choose the best approach.
When AIHA relapses, we first check the patient’s current health and past treatments. We look at how severe the relapse is and what might have caused it. Knowing what treatments worked before helps us decide what to do next.
For those who relapse after first treatment, we look at second-line options. These might include drugs like cyclophosphamide or azathioprine to lower antibody levels. Rituximab, a monoclonal antibody, is also considered. It targets B cells, which play a big role in the autoimmune process.
| Treatment Option | Description | Potential Benefits |
| Rituximab | Monoclonal antibody targeting B cells | Effective in reducing antibody production and inducing remission |
| Cyclophosphamide | Immunosuppressive drug | Can significantly reduce disease activity |
| Azathioprine | Immunosuppressive drug | Useful for long-term management |
For those with hard-to-treat AIHA, new treatments offer hope. Complement inhibitors target the complement system, which causes hemolysis. BTK inhibitors also show promise by controlling B cell activity.
In some cases, mixing treatments can be beneficial. This might mean combining drugs with rituximab or new therapies. The aim is to get a longer-lasting remission by tackling the disease from different angles.
When mixing treatments, weighing benefits against risks is key. This includes looking at possible side effects. Choosing the right patient and closely monitoring them is vital.
Making lifestyle changes can help with AIHA treatment. These changes can lower the chance of AIHA coming back. While medicine is key, some lifestyle tweaks can also help manage the condition.
Eating well is important for health and managing AIHA. We suggest:
Some people might need to avoid certain foods that can make symptoms worse. But, how well you can handle these foods can vary.
Stress can make AIHA symptoms worse. Good ways to handle stress include:
We suggest trying different stress management methods to see what works best for you.
Being active is good for health and stress. For those with AIHA, it’s important to:
Talking to a healthcare provider before starting a new exercise routine is a good idea.
Getting sick can make AIHA symptoms come back. To avoid infections:
We also advise talking to a healthcare provider about travel plans to lower infection risks.
Living with recurrent Autoimmune Hemolytic Anemia (AIHA) is tough. It affects more than just the body. It’s about dealing with emotional and psychological challenges too.
Dealing with recurrent AIHA can deeply affect your mind. You might feel anxious, scared of another episode, and unsure about the future. Watching your condition closely can make you feel drained.
The emotional toll of recurrent AIHA should not be underestimated. Healthcare providers need to see this and offer help for both body and mind.
Finding ways to cope is key when dealing with recurrent AIHA. Mindfulness, meditation, and therapy can help. They can make you feel more in control and better overall.
These methods can help you feel more in charge of your life and improve your well-being.
Having a strong support system is crucial for those with recurrent AIHA. This includes family, friends, doctors, and support groups.
| Support System Component | Description | Benefits |
| Family and Friends | Emotional support and practical help | Reduces feelings of isolation, provides practical assistance |
| Healthcare Professionals | Medical guidance and treatment | Ensures appropriate medical care, offers reassurance |
| Support Groups | Connection with others experiencing AIHA | Provides community, shares experiences and advice |
Creating a strong support network helps patients face the challenges of recurrent AIHA better.
Managing recurrent AIHA needs a mix of medical care, lifestyle changes, and emotional support. Understanding the mental impact, using coping strategies, and having a solid support system can greatly improve life quality.
Managing Autoimmune Hemolytic Anemia (AIHA) for the long term needs a mix of medical care, lifestyle changes, and emotional support. We’ve looked into AIHA’s types, symptoms, how it’s diagnosed, and treatment choices. It’s key to know the risks of it coming back and to spot early signs.
Handling AIHA long-term means using a wide strategy. This includes medicines, lifestyle changes, and keeping an eye on how the condition is doing. A focus on the patient can make life better for those with AIHA.
Medical treatments like steroids, rituximab, and removing the spleen can help manage AIHA. Making lifestyle changes, like eating right, managing stress, and avoiding infections, also helps. These steps can lower the chance of AIHA coming back and improve health overall.
AIHA is when the immune system attacks and destroys red blood cells. Yes, it can come back after treatment. The chance of it happening again depends on several things, like the type of AIHA and the treatment used.
Symptoms of AIHA relapse include anemia, jaundice, and fatigue. You might also feel short of breath and have dark urine. Lab tests show it too, like low hemoglobin and high LDH.
Remission is checked by looking at your blood and how your body is doing. The first remission can last from months to years. It depends on the AIHA type and treatment.
Certain conditions and genetic factors can make AIHA come back. So can some medicines and environmental things. Knowing these can help lower the risk.
Rituximab can help prevent AIHA relapse in some people. The time it takes for relapse after treatment can vary. It can be months to years.
Splenectomy can help control AIHA and lower relapse risk. But, it’s a surgery with risks like infection and bleeding. The decision to have it should be carefully thought over.
Patients can keep an eye on their condition with regular check-ups and blood tests. They should also watch for symptoms and tell their doctor if anything changes.
For relapsed AIHA, doctors might use other treatments or new therapies. These include targeted treatments and combinations. New options are being explored for hard-to-treat cases.
Yes, making lifestyle changes can help. This includes eating right, managing stress, exercising, and preventing infections. Talk to your doctor about what’s best for you.
AIHA can affect your mind, causing anxiety, depression, and stress. To cope, build a support network, manage stress, and seek help when needed.
Hansen, D. L., et al. (2024). Overall survival and treatment patterns among patients with primary and secondary warm autoimmune hemolytic anemia. British Journal of Haematology. https://pmc.ncbi.nlm.nih.gov/articles/PMC11613582
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!