Last Updated on October 21, 2025 by mcelik
Getting a cancer diagnosis can be scary. But knowing when to see an oncologist can really help. Did you know over 1.9 million people in the U.S. get cancer every year? While seeing an oncologist is common for cancer, it’s not the only reason.
So, what is an oncologist? An oncologist is a doctor who deals with cancer. They help diagnose, treat, and manage it. We’ll look at what oncologists do, their education, and what happens during an oncologist consultation.
It’s key to know what an oncologist does for those facing cancer. An oncologist is a doctor who deals with cancer. They diagnose, treat, and manage it.
An oncologist is a doctor with deep knowledge in oncology. This is the study of cancer. They give full care to patients, from start to finish.
There are many kinds of oncologists, each with their own area:
The oncology care team is a team effort. It includes oncologists, nurses, and more. Everyone works together for the best care.
To be an oncologist, you need a lot of education and training:
Knowing about an oncologist and the oncology care team helps patients on their cancer path.
Many people worry that seeing an oncologist means they have cancer. But, this isn’t always true.

Seeing an oncologist doesn’t always mean you have cancer. This is not true. Oncologists deal with cancer, but they also manage other conditions.
There are many reasons to see an oncologist. These include:
Oncologists also manage conditions not related to cancer. For example, they might be involved in:
Getting referred to an oncologist starts with your primary care doctor. They check your symptoms, medical history, and test results. They decide if you need a specialist’s help.
Your primary care doctor might refer you to an oncologist for a closer look. This doesn’t mean you have cancer. It means they want to make sure you get the right care.
It’s normal to feel anxious about oncology visits. To help with this, consider:
Knowing what an oncologist does and why you’re seeing one can help. It can make you feel less anxious and more prepared for your visit.
Oncologist referrals often come from health concerns or risk factors. These need a specialist’s look. We’ll look at why people see an oncologist.
Abnormal test results are a big reason for oncologist visits. These can be from routine tests or follow-ups. For example, an odd mammogram or a strange skin spot can lead to a visit.
A family history of cancer can raise your risk. Genetic tests might be suggested to check for cancer-linked genes.
Some symptoms, like unexplained weight loss or pain, might need an oncologist’s check. They’re trained to spot cancer signs.
People at high cancer risk might see an oncologist for preventive care. This includes more tests and early monitoring.
| Reason for Referral | Description |
| Abnormal Test Results | Results from screenings or diagnostic tests that indicate a problem. |
| Family History | A big family history of certain cancers that raises your risk. |
| Suspicious Symptoms | Unusual or unexplained symptoms that need more checking. |
| Preventive Care | Care for those at high risk, with more tests and watching. |
When a primary care doctor decides to send a patient to an oncologist, it’s a big step. They think carefully and prepare well. This choice is made after tests show cancer or other serious conditions might be present.
Primary care doctors are key in finding and treating cancer early. They look at the patient’s history, test results, and their own judgment to decide when to refer. They might refer if tests show something odd, if there’s a family history of cancer, or if symptoms seem cancer-like.
“The primary care doctor is often the first person patients see,” says a doctor with over 10 years of experience. “They use guidelines and their knowledge to know when a patient needs a specialist.”
When a referral is made, the primary care doctor shares important patient info with the oncologist. This includes the patient’s medical history, past test results, and family cancer history. Good communication between doctors is key to keeping care smooth.
The wait time for an oncology appointment can vary a lot. It depends on how urgent the case is, how many oncologists are available, and the healthcare system’s capacity. Non-urgent cases might wait weeks, but urgent ones are seen sooner.
A recent study found that waiting times for oncology consultations can be from a few days to weeks. “Quick access to oncology care is vital for patient results,” says an oncologist. “We try to see patients fast, and even faster for urgent cases.”
Expedited referrals happen when a patient needs to see an oncologist right away. This is for severe symptoms, suspicious test results, or a high cancer risk due to genetics. These quick referrals are important for timely care and better treatment outcomes.
In summary, the referral process to oncology is a careful and coordinated effort between primary care doctors and oncologists. Knowing about this process helps patients get the care they need quickly and effectively.
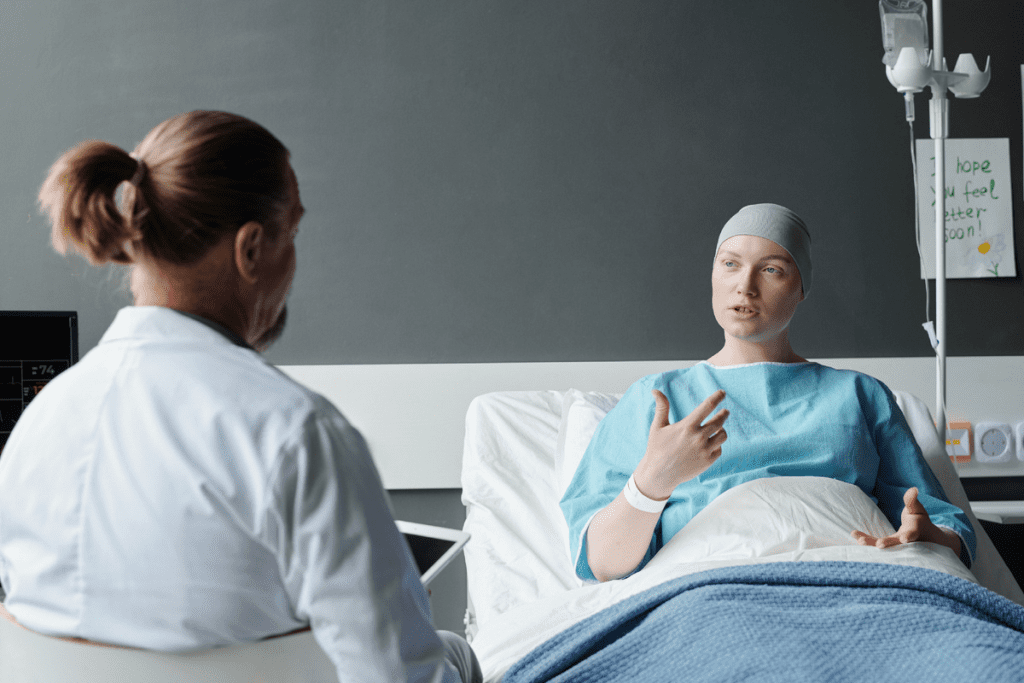
Knowing what to expect at your first oncologist visit can make it less scary. Preparing for this big step can help reduce your anxiety. Learning about the procedures and processes beforehand can make a big difference.
Your first visit will start with a review of your medical history. The team will talk about your symptoms, past illnesses, and treatments. A detailed assessment is key to creating a good care plan.
The oncologist will then do a physical exam. They might look for any unusual signs or symptoms. This thorough check helps figure out what to do next.
Your oncologist will ask many questions to understand your situation. They might ask about:
Answering these questions truthfully and fully is important for your care plan.
After the initial check-up, your oncologist might order more tests. These could include:
To get the most out of your first oncology visit, consider the following:
Being prepared is essential for a productive first appointment. By knowing what to expect and being organized, you can make the most of your visit. This is the first step towards a detailed care plan.
Cancer diagnosis uses many tests and procedures. Oncologists use these to decide on treatments. These steps are key to finding out the cancer type and stage. This helps in making treatment plans that fit each person.
Oncologists use several tests to find cancer. These include:
A biopsy is a key tool for finding cancer. It involves taking a tissue sample for examination. There are different types of biopsies, including:
Biopsy results help oncologists know if cancer is present, what type it is, and its stage. This information guides the treatment plan.
Imaging tests are essential for diagnosing and staging cancer. Common imaging studies include:
These imaging studies help oncologists understand how far cancer has spread. They plan treatments based on this information.
Genetic and molecular tests look at cancer cell genetics. These tests find specific mutations or changes. This information helps decide on treatments. Examples include:
Knowing a tumor’s genetic makeup helps oncologists tailor treatments. This makes treatments more effective for each person.
Oncologists play a key role in cancer care at different stages. They help from the start to the end of treatment. These doctors specialize in diagnosing, treating, and managing cancer.
Oncologists often start early with screening programs. These programs aim to find cancer early, even before symptoms show. Early detection can greatly improve treatment success.
For example, mammograms and colonoscopies are common tests. They help find breast and colon cancers early.
If you have a family history of cancer or risk factors, talk to your doctor. They might refer you to an oncologist for screening.
Other doctors might find cancer first. For instance, a dermatologist might spot skin cancer, or a gastroenterologist might find colon cancer. After a diagnosis, an oncologist helps plan treatment.
This step is important. It ensures the patient gets care suited to their cancer and health.
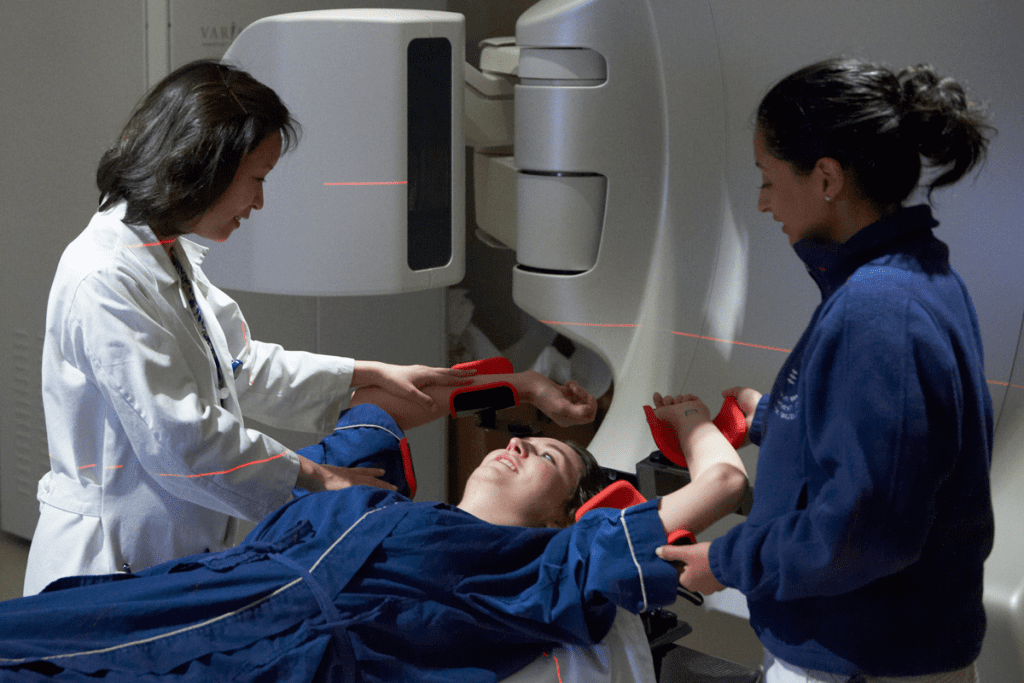
Oncologists are key in planning treatment. They work with a team to create a plan. This plan might include surgery, chemotherapy, or radiation.
The plan is made just for the patient. It considers the cancer type, stage, and the patient’s health and wishes.
After treatment, oncologists keep an eye on the patient. They check for cancer coming back. They also help with lifestyle changes and treatments to prevent recurrence.
| Stage of Cancer Care | Oncologist’s Role | Typical Procedures |
| Early Detection | Screening and risk assessment | Mammograms, colonoscopies |
| Diagnosis | Confirming diagnosis, staging | Biopsies, imaging studies |
| Treatment Planning | Developing a treatment plan | Surgery, chemotherapy, radiation therapy planning |
| Recurrence Monitoring | Monitoring for recurrence, managing side effects | Follow-up appointments, imaging studies, blood tests |
Knowing when oncologists get involved helps patients. By working with their oncologist and other doctors, patients get care that fits their needs.
Oncologists are key in cancer treatment, helping patients from start to finish. They create treatment plans that fit each patient’s needs.
Good cancer treatment needs a solid plan. Oncologists team up with many experts to plan treatments. They consider the cancer type, stage, patient health, and what the patient wants.
Oncologists keep a close eye on how treatments work. They check often and change plans if needed. They use new tests and scans to see how well treatments are working.
Treatment can cause side effects and problems. Oncologists aim to lessen these and handle them well. They use medicines and lifestyle changes to help manage side effects.
Cancer care works best with a team effort. Oncologists work with surgeons, radiologists, and others to care for patients. This team approach covers all parts of a patient’s care.
Cancer treatment doesn’t stop after the initial treatment. Follow-up care with oncologists is key for long-term health. The time after treatment can be a mix of relief and worry for patients. Regular visits with oncologists are important for checking on recovery, managing side effects, and catching any signs of cancer coming back early.
The number of oncology visits can change a lot. It depends on the cancer type, treatment plan, and patient’s health. Patients usually see their oncologist:
These visits help oncologists see how treatment is going. They can make changes and help manage side effects.
After treatment, patients start a surveillance phase. The follow-up schedule depends on the cancer type, stage, and treatment. A common schedule might be:
| Year | Frequency of Follow-Up |
| 1st Year | Every 3-4 months |
| 2nd Year | Every 6 months |
| 3rd Year and beyond | Annually or as needed |
This schedule can change based on the patient’s health and any concerns.
Long-term care is vital for checking late treatment effects, managing chronic conditions, and providing ongoing support. Oncologists work with other healthcare teams to create a long-term plan. This plan might include regular check-ups, imaging tests, and blood work. For example, patients who had radical cystectomy might need:
When patients finish treatment and enter the survivorship phase, their care team helps them transition to a survivorship care plan. This plan outlines the ongoing care and support needed, including follow-up appointments, screening tests, and managing long-term and late effects. We work closely with patients to ensure a smooth transition, providing them with the resources and support they need to thrive in the survivorship phase.
By understanding the importance of follow-up care and working closely with their oncologist, patients can navigate the post-treatment period with confidence. They know they have the support they need for long-term health and well-being.
Talking well with your oncologist is key to getting your diagnosis and treatment options. Knowing your care plan helps you make smart health choices.
Make a list of questions before seeing your oncologist. This way, you can cover all your concerns. Ask about your diagnosis, treatment choices, side effects, and lifestyle changes.
Oncologists use special terms. If you don’t get a term, ask them to explain it. Knowing your diagnosis and treatment is key to making good choices.
Common Terms to Understand:
A good doctor-patient relationship is based on trust, respect, and open talk. Be open with your oncologist about your symptoms, worries, and challenges. This helps them give you the best care.
Having family or a caregiver at appointments is helpful. They offer support, help remember things, and ask questions you might not think of. Talk to your oncologist about who can be there and how they can help with your care.
By using these tips, you can talk better with your oncologist. This makes your cancer journey more confident and easier to handle.
When you get a cancer diagnosis, you might want a second opinion. This can help you get the best care. It gives you more information about your condition and treatment options.
There are times when getting a second opinion is a good idea. These include:
As a renowned oncologist, notes, “A second opinion can offer patients reassurance and confidence in their treatment plan, which is key for their well-being.”
Getting a second opinion is easy. Start by asking your current oncologist for a referral. Many healthcare providers support patients seeking more opinions.
| Steps to Request a Second Opinion | Description |
| 1. Discuss with your current oncologist | Tell them you want a second opinion. |
| 2. Obtain medical records | Make sure all your medical records are sent to the new oncologist. |
| 3. Choose a second oncologist | Look for specialists who know a lot about your cancer type. |
If the first and second opinions are different, don’t worry. Here’s what to do:
It’s important for patients to feel sure about their treatment choices.
Most oncologists see second opinions as part of good care. They know patients want to be well-informed and might want more advice.
“Seeking a second opinion is common and helpful. It lets patients look at different treatments and understand their condition better.” –
Oncologist
Dealing with cancer care can be tough. But knowing you can get a second opinion is reassuring. It lets you take a bigger role in your treatment.
When you get a cancer diagnosis, finding the right oncologist is key. This choice can greatly affect your treatment and care experience.
To find the right oncologist, start by looking at their credentials and experience. Make sure they are board certified in medical oncology, hematology, or radiation oncology. Check their education, training, and any special certifications they have.
The hospital or treatment facility where your oncologist works is also important. Think about these factors:
Understanding your insurance and the oncologist’s practice is key. Here are important points to consider:
Patient reviews and satisfaction ratings offer valuable insights. Look for feedback on:
By carefully considering these factors, you can find an oncologist who has the right credentials and experience. They will also provide the care and support you need during your cancer journey.
Seeing an oncologist is key in cancer care. Oncologists help diagnose, treat, and manage cancer. Knowing when to see one and what to expect is important for your care.
Oncologists are vital from the start to follow-up care. They work with other doctors to give care that fits each patient’s needs. Understanding their role helps patients navigate their cancer journey better.
If you’re facing cancer or treatment, knowing what an oncologist does can ease your worries. This article aims to give you insights into cancer care and the role of oncologists.
An oncologist is a doctor who deals with cancer. They help patients with cancer by creating treatment plans and managing symptoms. They also provide support during treatment.
No, seeing an oncologist doesn’t mean you have cancer. They help with many health issues, not just cancer. You might see one if you have unusual symptoms or a family history of cancer.
There are several types of oncologists. Medical oncologists use medicine to treat cancer. Radiation oncologists use radiation. Surgical oncologists remove tumors through surgery.
At your first visit, your oncologist will review your medical history. They will also do a physical exam and talk about your symptoms and test results. They might order more tests to help diagnose or stage your condition.
Bring any medical records, test results, and a list of your medications to your first appointment. It’s also a good idea to write down any questions or concerns you have.
Oncologists are key in cancer treatment. They create treatment plans, manage symptoms, and provide support. They work with other doctors to give patients the best care.
How often you see your oncologist depends on your cancer type and treatment plan. They will schedule regular visits to check on your progress and adjust your treatment as needed.
Yes, getting a second opinion is okay. Many oncologists encourage it, even for complex treatments.
Start by researching an oncologist’s credentials and experience. Look at patient reviews and ask for referrals from your doctor or other healthcare professionals.
If you get different opinions, talk to each oncologist about your concerns. You might also want to seek more opinions or consult with other healthcare professionals.
Most oncologists value second opinions and are open to working with patients who seek them. They often encourage it, even for complex treatments.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!