Last Updated on October 21, 2025 by mcelik

Every year, over 1.8 million people in the United States get cancer. Hematology oncology is key in fighting blood cancers and disorders.
We’ll dive into the world of hematology oncology. It’s about studying and treating blood diseases, including cancer. This field needs a lot of education and training.
Knowing about hematology oncology is important for those in the field or seeking top medical care. We’ll cover the education and training needed for this career.
Hematology oncology is a key medical field that mixes hematology and oncology. It offers full care for blood issues and cancers. This field focuses on diagnosing, treating, and managing blood disorders and cancers.
This specialty combines studying blood problems like anemia and cancer. It gives a complete care approach. This is key to understanding how blood issues relate to cancer and its treatments.
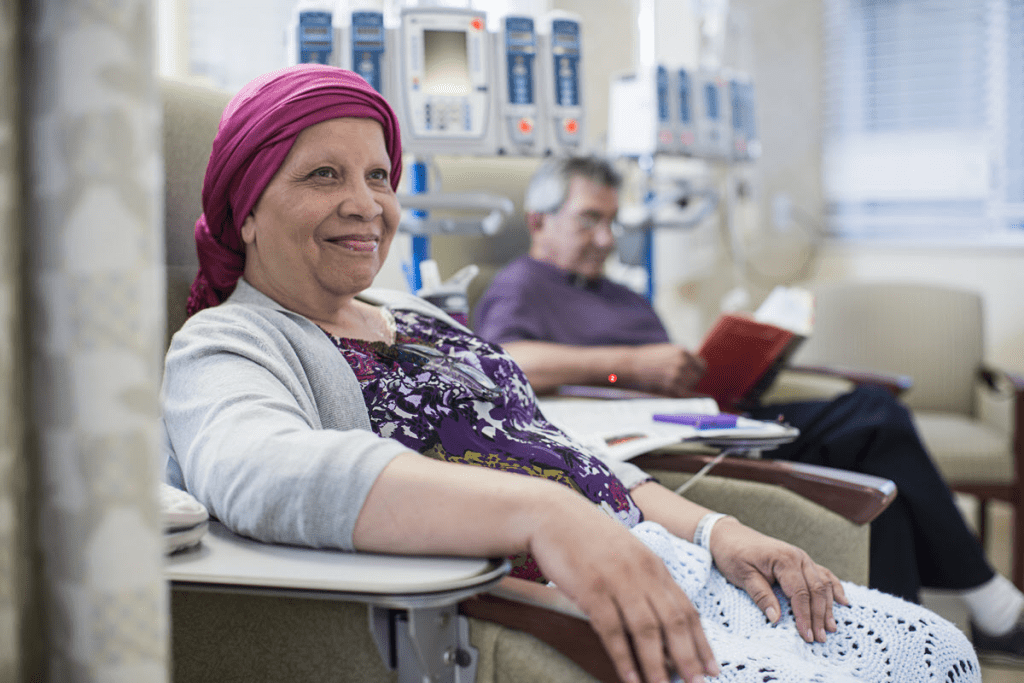
Hematology oncology covers a wide range of conditions. These include leukemias, lymphomas, and other blood cancers. Doctors in this field use treatments like chemotherapy and bone marrow transplants to help patients.
They need to know a lot about blood and cancer. They also understand how treatments affect these conditions.
Hematology and oncology are closely linked. Many blood and lymph system cancers need a full approach. This considers both the blood and cancer aspects.
For example, leukemia affects blood cells and its treatment must understand both. Lymphoma, a cancer of the lymph system, also needs a treatment plan that looks at both the cancer and the immune system.
| Condition | Description | Treatment Approaches |
| Leukemia | Cancer of the blood cells | Chemotherapy, targeted therapy, bone marrow transplantation |
| Lymphoma | Cancer of the lymphatic system | Chemotherapy, radiation therapy, immunotherapy |
| Anemia | Blood disorder characterized by low red blood cell count | Iron supplements, erythropoiesis-stimulating agents, blood transfusions |
In conclusion, hematology oncology is a vital field. It combines blood and cancer studies and treatments. By understanding these connections, doctors can give better care to patients.
Starting a career as a hematologist-oncologist needs a strong educational base. This path is both tough and fulfilling. It requires hard work, dedication, and a love for helping patients.
The first step is undergraduate studies. There’s no specific major needed for medical school. But, most choose science fields like biology, chemistry, or physics. You should take:
Keeping a high GPA, mainly in science, is key for medical school. Also, getting research experience and volunteering in healthcare can boost your application.
After undergrad, you go to medical school for four years. The program is split into:
In clinical rotations, you get real-world experience. This helps you choose your future specialty.
After medical school, you apply for internal medicine residency. This is a tough process. Key factors include:
| Factor | Description | Importance Level |
| USMLE Scores | United States Medical Licensing Examination scores | High |
| Research Experience | Participation in research projects, specially in hematology-oncology | Medium |
| Letters of Recommendation | Strong endorsements from faculty members or supervisors | High |
| Personal Statement | A well-crafted essay outlining career goals and motivations | Medium |
Knowing these factors can help you prepare better. This increases your chances of getting into the program.
The journey to becoming a hematologist-oncologist starts with internal medicine residency. This period is key. It teaches the basics of complex medical conditions, including blood disorders and cancer.
Internal medicine residency lasts three years. Residents see a wide range of medical conditions. The program mixes theory and practice.
The first year covers general internal medicine. Residents rotate through different subspecialties. Later years let them dive into areas like hematology and oncology.
Aspiring hematologist-oncologists learn vital skills during residency. These include diagnostic reasoning, patient management, and communication skills.
Residents learn to tackle complex cases step by step. They use knowledge from different fields to care for patients. They also improve their communication skills. These are key for working with patients, families, and healthcare teams.
Internal medicine residency is a common path to hematology oncology. But, some choose pediatrics. This is great for those interested in pediatric hematology oncology.
Pediatric residency offers a special view on treating blood disorders and cancers in kids. It requires knowing about child development and treating young patients.
The hematology oncology fellowship is a tough program. It’s designed to give future specialists a deep understanding and clinical skills. This training is key for doctors who want to be experts in blood disorders and cancer.
Getting into a hematology oncology fellowship is tough. Doctors apply through ERAS and go to interviews at different places. They look at your clinical experience, research, and letters of recommendation.
To get noticed, you need a solid base in internal medicine. Showing you’re really into hematology and oncology helps. Having research in blood cancers or disorders is a big plus.
Fellowships last three years. The program covers hematology and oncology deeply. You’ll learn about diagnosing, treating, and managing blood disorders and cancers.
The program has clinical and research parts. You’ll work with top doctors to improve your skills. You’ll also do research that helps the field.
| Curriculum Component | Description | Duration |
| Clinical Training | Direct patient care and management | 2 years |
| Research Training | Conducting original research projects | 1-2 years |
| Didactic Sessions | Regular lectures and seminars on hematology and oncology topics | Ongoing |
Fellows need to be good at both treating patients and doing research. They’ll manage patients with blood cancers and disorders. They’ll also do original research and share it at conferences.
Research can be on new treatments, outcomes, or how to apply research to patients. They work with mentors to plan and do their research.
After finishing the fellowship, doctors are ready to be hematologist-oncologists. They have the knowledge and skills to give top care to patients with blood disorders and cancer.
Becoming a hematologist-oncologist takes many years of education and training. We’ll look at each stage and how long it lasts to understand the total time needed.
First, you need a bachelor’s degree, which takes four years. Then, you go to medical school for four years to get an MD or DO. Next, you do a three-year internal medicine residency.
After that, you join a hematology-oncology fellowship program for three years. So, from high school, it’s about 14 years of education and training.
Some people want to add more years for research or specialized training. You can spend extra time on research during medical school or residency. Also, extra fellowship training in a subspecialty can add one to two years.
Key considerations for extensions include:
Compared to other doctors, hematologist-oncologists have a long journey. For example, family medicine doctors need 11 years after high school. Dermatologists need 12-13 years.
The complexity of hematology-oncology as a specialty justifies its lengthy training period. It requires deep knowledge of blood disorders and cancers. Plus, staying current with new treatments and research is essential.
Hematology oncology offers many chances for subspecialization. This lets doctors focus on areas they love and meet patient needs better. As the field grows, the need for specialized knowledge and skills is clear.
Many doctors choose to get more training after their fellowship. These advanced fellowships give deep knowledge and practical experience. They help doctors get better at their jobs and improve patient care.
Some areas for extra training include:
In hematology oncology, there are many special areas. Each one tackles specific conditions or treatments. These include:
Bone Marrow Transplant: This area cares for patients getting bone marrow transplants. It’s a key treatment for many blood cancers and disorders.
Hemostasis: Hemostasis specialists work on blood clotting problems. They create treatment plans for issues like thrombophilia or bleeding disorders.
By focusing on these areas, doctors can give better care. This leads to better results for patients. As the field keeps growing, the need for these experts will likely increase.
Board certification is key for hematologist-oncologists to show their skills. It proves they know their stuff and can care for patients well in hematology and oncology.
To get certified, hematologist-oncologists need to pass a tough test. The American Board of Internal Medicine (ABIM) offers this certification. They must finish a fellowship in hematology and oncology and meet certain training needs.
The test checks their knowledge in hematology and oncology. It looks at how they diagnose and treat patients. It’s to see if they can use their knowledge in real-life situations.
Keeping certification up is a big deal. Hematologist-oncologists must keep learning and follow the ABIM’s MOC program. This means:
Hematologist-oncologists can choose single or dual certification. Single certification is in one area, like hematology or oncology. Dual certification covers both. Most choose dual because it shows they’re experts in both fields.
Choosing depends on their career goals, practice needs, and what they’re good at.
Hematology and oncology are two medical fields that often work together. Hematology deals with blood disorders like anemia and blood cancers. Oncology, on the other hand, focuses on cancer treatment, including blood cancers.
Hematology and oncology share some similarities, but they also have their own areas of focus. Hematologists handle blood disorders, not all of which are cancers. Oncologists, by contrast, specialize in cancer treatment using various methods.
Even though they differ, these fields are closely connected. Many blood disorders, like leukemia, are treated like cancers. This is why some doctors choose to specialize in both, providing better care for complex cases.
| Aspect | Hematology | Oncology |
| Primary Focus | Blood disorders, including anemia, clotting disorders, and blood cancers | Cancer diagnosis, treatment, and management, including solid tumors and hematological malignancies |
| Common Conditions Treated | Anemia, hemophilia, leukemia, lymphoma | Various cancers, including breast, lung, colon, and hematological cancers |
| Treatment Approaches | Blood transfusions, clotting factor replacement, chemotherapy for blood cancers | Chemotherapy, radiation therapy, surgery, immunotherapy |
Doctors may choose hematology or oncology based on their interests. Some might prefer hematology for its complex blood disorders. Others might choose oncology for its focus on cancer treatment. Their choice can also depend on the patients they want to help.
The training for hematology and oncology starts with basic medical education. To specialize in hematology, doctors need a hematology fellowship. For oncology, they need an oncology fellowship. Many choose a combined fellowship for both, gaining expertise in both areas.
To understand why hematology and oncology are often together, we need to look at their history and benefits. The field of hematology oncology has grown a lot. This is because blood disorders and cancer are closely linked.
In the early 20th century, it was clear that many blood issues were connected to cancer. Hematologists were among the first to handle leukemia and lymphoma, cancers of the blood and lymph system.
“The close relationship between hematology and oncology is not merely a matter of convenience but is based on the biological and clinical overlap between blood diseases and cancer.” – Hematologist-Oncologist
Over time, hematology and oncology have become more connected. Advances in one field help the other. This has led to better treatments for both blood disorders and cancer.
Combining these fields has many benefits. It allows for a more complete approach to treating patients with complex conditions. Treatments for one area can often be used for the other, speeding up progress in both.
| Advantages | Description |
| Comprehensive Care | Patients get care for both blood disorders and cancer. |
| Research Synergy | Advances in hematology help improve oncology treatments, and vice versa. |
| Training and Expertise | Hematologist-oncologists are trained for many conditions, improving care. |
Hematology oncology departments are set up in hospitals and research centers. These departments help specialists work together. This ensures patients get the best care.
Departments of hematology oncology use a team approach. This includes hematologists, oncologists, pathologists, radiologists, and support staff. This model improves care and encourages research and innovation.
Hematologist-oncologists play a key role in treating blood diseases and cancers. They are medical experts with deep training. They diagnose and treat blood-related issues and cancers.
Hematologist-oncologists handle many tasks. They diagnose and treat blood disorders and cancers. Their duties include:
Hematologist-oncologists work in hospitals, clinics, and private practices. Their job is fast-paced and demanding. They must keep up with new medical discoveries and technologies.
Good patient care needs teamwork. Hematologist-oncologists work with many healthcare professionals. They team up with:
Here’s a quick look at what hematologist-oncologists do:
| Responsibility | Description |
| Diagnosis | Conducting thorough medical histories, physical examinations, and interpreting diagnostic tests. |
| Treatment Planning | Developing and implementing treatment plans, including chemotherapy, targeted therapy, and bone marrow transplantation. |
| Supportive Care | Providing care to manage symptoms and side effects of treatment. |
| Collaboration | Working with other healthcare professionals to ensure complete patient care. |
Hematology oncology deals with blood-related issues and cancers. Specialists in this field handle complex cases. They are trained to manage a wide range of disorders.
These conditions fall into blood disorders, cancers, and overlapping issues. They need thorough care.
Blood disorders are a big part of this field. They include:
These need precise diagnosis and treatment plans. Plans often include medicine, lifestyle changes, and sometimes surgery.
Hematology oncology specialists also treat cancers. These include:
“Treatment for these cancers often involves chemotherapy, targeted therapy, or bone marrow transplantation,” says a leading hematologist. “A team effort is key for good management.”
Some conditions are both blood disorders and cancers. They need a detailed understanding and approach. For example, some myeloproliferative neoplasms can turn into acute leukemia. Treating these conditions requires a plan that covers both aspects.
By grasping these complexities, specialists can offer personalized care. This care improves patient results. Keeping up with new research and treatments is vital in this field.

Knowing what to expect at your first visit with a hematologist-oncologist can ease your worries. This appointment is key to understanding your health and creating a treatment plan. It’s a chance to get a detailed look at your condition.
Your doctor will start by asking about your medical history. They’ll want to know about your symptoms, past health issues, family history, and current medications. A physical exam will also be done to check for signs of blood disorders or cancer.
Key components of the evaluation process include:
To find out what’s wrong, your doctor might run some tests. These could be:
It’s important to follow your healthcare team’s instructions for these tests.
| Test Type | Purpose | Preparation |
| Blood Tests | Check for abnormalities in blood cells | May require fasting; follow specific instructions |
| Imaging Tests | Visualize internal structures | May require contrast dye; inform about any allergies |
| Bone Marrow Biopsy/Aspiration | Examine bone marrow for disease | Local anesthesia used; follow post-procedure care instructions |
After your tests, you’ll have a follow-up to talk about the results and your treatment plan. This plan might include chemotherapy, targeted therapy, or other treatments based on your condition.
“The first visit is critical as it sets the stage for your entire treatment journey. Being prepared and understanding the process can make a significant difference in your experience.” – Hematologist-Oncologist
Your hematologist-oncologist will work with you to create a treatment plan that’s just right for you. They’ll make sure you get the care you need throughout your treatment.
Caring for kids with blood issues and cancer needs a special touch. That’s where pediatric hematology oncology comes in. It combines hematology and oncology to meet kids’ unique needs.
Pediatric hematology oncology specialists get special training. Their education focuses on kids’ differences, preparing them for age-appropriate care. They also get extra years of training in pediatric hematology and oncology.
Becoming a pediatric hematologist-oncologist takes a lot of time and effort. After medical school, they do pediatric residency and then a fellowship in pediatric hematology oncology. It can take over a decade from undergrad to specialized training. This long training prepares them for the challenges of pediatric blood disorders and cancers.
Pediatric hematology oncology focuses on kids’ unique needs. Specialists must handle kids’ emotional and psychological needs along with their medical care. They also keep up with the latest research and treatments for kids.
This field is more than treating diseases. It’s about caring for kids and their families. Pediatric hematology oncology specialists are key in healthcare, bringing hope and healing to those with blood disorders and cancer.
The field of hematology oncology is rapidly evolving. New treatments and research are changing how we diagnose and treat blood disorders and cancers. This leads to better care for patients.
New developments include targeted therapies, immunotherapies, and precision medicine. Targeted therapies aim at specific cancer molecules, sparing healthy cells. Immunotherapies, like CAR-T cell therapy, use the immune system to combat cancer.
Precision medicine tailors treatments to each patient’s genetic makeup. This method is showing great promise in treating leukemia and lymphoma.
The fast pace of new treatments and technologies requires ongoing education for doctors. Fellowship programs now include training in these new areas. This ensures hematologist-oncologists can offer top-notch care.
There’s also a growing need for interdisciplinary collaboration. Hematologist-oncologists are working with geneticists and radiologists for a more complete approach to care.
Research is pushing hematology oncology forward. We’re looking at new immunotherapies, better stem cell transplantation, and using artificial intelligence in treatment planning.
The future looks bright for hematology oncology. With ongoing research and education, we can expect even better patient outcomes and quality of life. It’s essential to keep investing in these areas.
The job outlook for hematologist-oncologists is bright. Medical tech is advancing, and more people are living longer. This means more work for these specialists.
More people are getting blood disorders and cancer. This has increased the need for hematologist-oncologists. They are in demand in many healthcare places.
Salaries for hematologist-oncologists vary. They depend on where you work, your experience, and your specialty. These doctors are well-paid because of their training and the complexity of their work.
| Practice Setting | Average Salary Range |
| Private Practice | $400,000 – $600,000 |
| Academic Institution | $350,000 – $550,000 |
| Research Organization | $300,000 – $500,000 |
Hematologist-oncologists can work in academia or clinical settings. Academic work includes research, teaching, and patient care. Clinical work focuses mainly on treating patients.
Choosing between academia and clinical work depends on personal goals and preferences. Both paths are important for the field’s progress and offer rewarding careers.
Thinking about a career in hematology oncology? It’s a big decision that needs careful thought. You’ll need to consider your interests, skills, and what you want to achieve. This field requires a lot of time and effort, with at least 11 years of education and training after high school.
We’ve talked about the steps to become a hematologist-oncologist. This includes undergraduate studies, residency, and fellowship programs. Getting board certified and specializing in areas like pediatric oncology are also key. This career is rewarding, allowing you to help patients with blood disorders and cancer.
Now, think about your own dreams and abilities. Is a career in hematology oncology right for you? If you love caring for patients and want to contribute to research, this path might be perfect.
Hematology oncology is a medical field that deals with blood disorders and cancer. It covers diagnosing, treating, and managing blood-related issues. This includes anemia, clotting problems, leukemia, lymphoma, and other cancers.
It takes about 13 to 15 years to become a hematologist-oncologist. This includes studying for an undergraduate degree, medical school, an internal medicine residency, and a fellowship in hematology oncology.
To be a hematologist-oncologist, you need to finish your undergraduate studies. Then, you must attend medical school, complete an internal medicine residency, and finish a fellowship in hematology oncology.
Hematology focuses on blood disorders. Oncology is about treating cancer. Hematology oncology combines both, as many blood disorders and cancers are related.
Hematology and oncology are often together because blood disorders and cancer are closely linked. Many blood cancers, like leukemia and lymphoma, need expertise from both fields for treatment.
The fellowship in hematology oncology lasts three years. It includes both clinical and research training. This prepares you to diagnose and treat blood disorders and cancer.
Hematologist-oncologists diagnose and treat blood disorders and cancer. They manage patient care, work with teams, and keep up with new treatments and technologies.
Specialists in this field treat blood disorders like anemia and clotting issues. They also treat cancers, including leukemia, lymphoma, and multiple myeloma.
At the first appointment, patients get a detailed evaluation. This includes a medical history, physical exam, and diagnostic tests. The specialist will then discuss the diagnosis, treatment options, and follow-up care.
Pediatric hematology oncology deals with children’s blood disorders and cancer. It requires special training in pediatric care. Children’s conditions and treatment responses are different from adults.
Hematologist-oncologists have many career options, including academic and clinical roles. The demand for these specialists is growing. This is because more people are getting blood disorders and cancer.
Yes, it’s a rewarding career. It allows you to make a big difference in patients’ lives. It requires dedication to ongoing education and staying current with new advancements.
South Alabama University. (2023). Hematology and Medical Oncology Fellowship.
https://www.southalabama.edu/colleges/com/departments/internalmedicine/oncology-fellowship.html
Explains fellowship duration of 3 years after internal medicine residency.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!