
Autoimmune Hemolytic Anemia (AIHA) is a rare condition. It happens when the immune system attacks and destroys red blood cells. This leads to a shortage of healthy red blood cells in the body. This condition can significantly impact a person’s quality of life and, if left untreated, can lead to serious complications. It’s important for patients and healthcare providers to understand the prognosis and factors influencing life expectancy to make informed decisions about treatment.
The prognosis of AIHA varies widely. It depends on several factors, including the underlying cause, response to treatment, and presence of complications. We will explore these factors in detail. This will provide insights into the survival rate and life expectancy of patients with AIHA.
Key Takeaways
- AIHA is a rare condition that affects red blood cells.
- The prognosis varies based on the underlying cause and response to treatment.
- Understanding AIHA prognosis is key for informed treatment decisions.
- Several factors influence the life expectancy of AIHA patients.
- Early diagnosis and treatment can significantly improve outcomes.
What Is Autoimmune Hemolytic Anemia?
Autoimmune Hemolytic Anemia (AIHA) is a condition where the immune system attacks the body’s red blood cells. This can greatly affect a person’s life, making it important to know about it.
Definition and Basic Mechanism
AIHA happens when the immune system makes antibodies against the body’s red blood cells. These antibodies mark the cells for destruction. The spleen then removes these marked cells, causing anemia.
The reasons for AIHA can vary. It might be due to genetics or environmental factors. Sometimes, it’s linked to other autoimmune diseases, infections, or medications.
Types of Autoimmune Hemolytic Anemia
AIHA is divided into types based on the antibodies’ temperature sensitivity and the direct antiglobulin test (DAT) results. The main types are:
- Warm Autoimmune Hemolytic Anemia: This is the most common form, where the antibodies are active at body temperature.
- Cold Agglutinin Disease: In this type, the antibodies are more active at colder temperatures, leading to red blood cell agglutination.
- Mixed AIHA: A combination of warm and cold AIHA characteristics.
- Atypical AIHA: Cases that do not fit into the above categories.
Knowing the specific type of AIHA is key to finding the right treatment.
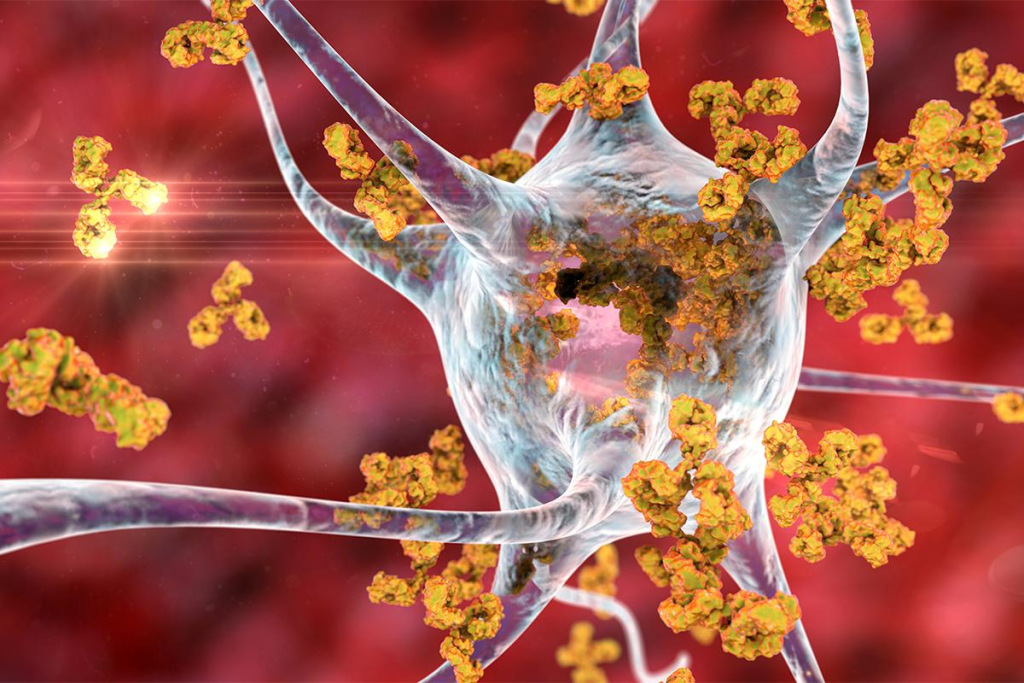
The Pathophysiology of AIHA
The immune system’s problems are at the heart of AIHA. This leads to the breakdown of red blood cells. The body mistakenly attacks its own red blood cells, marking them for destruction.
How the Immune System Attacks Red Blood Cells
In AIHA, autoantibodies target red blood cells. This causes their destruction through different ways. The complement system is key, helping to break down red blood cells or mark them for removal.
Key mechanisms include:
- Activation of the complement cascade
- Antibody-dependent cellular cytotoxicity
- Splenic sequestration and destruction of red blood cells
The Process of Hemolysis
Hemolysis in AIHA can happen in two ways. Intravascular hemolysis is when red blood cells break down in the blood. This is often due to the complement system. Extravascular hemolysis happens when the spleen removes antibody-coated red blood cells.
The severity of hemolysis varies. This can cause mild anemia or severe hemolytic crises.
| Mechanism | Description | Clinical Impact |
| Intravascular Hemolysis | Direct lysis of red blood cells in the bloodstream | Can lead to severe anemia and hemoglobinuria |
| Extravascular Hemolysis | Removal of antibody-coated red blood cells by the spleen | Results in anemia and splenomegaly |
Knowing how AIHA works is key to finding good treatments.
Warm Autoimmune Hemolytic Anemia
Warm Autoimmune Hemolytic Anemia (AIHA) is the most common type. It happens when the body makes antibodies that attack red blood cells at normal body temperature. About 60-80% of AIHA cases are Warm AIHA.
Characteristics and Prevalence
Warm AIHA is marked by IgG antibodies that target red blood cells. This happens at or near normal body temperature. It’s more common than other AIHA types, making up a big part of cases.
It can affect anyone but is more common in some groups. This includes people with certain diseases or disorders. Symptoms can range from mild to severe, affecting how much blood is in the body.
Specific Causes and Risk Factors
The exact causes of Warm AIHA are not fully known. But, some factors increase the risk. These include genetics, certain diseases, and infections. We’ll look at these in more detail.
The table below shows some risk factors and conditions for Warm AIHA:
| Risk Factor/Associated Condition | Description | Relevance to Warm AIHA |
| Lymphoproliferative Disorders | Conditions characterized by the excessive production of lymphocytes. | Commonly associated with Warm AIHA. |
| Autoimmune Diseases | Diseases where the immune system attacks the body’s own tissues. | Often linked with the development of Warm AIHA. |
| Infections | Certain viral or bacterial infections can trigger autoimmune responses. | May contribute to the onset of Warm AIHA in susceptible individuals. |
Knowing these risk factors helps doctors diagnose and treat Warm AIHA better. They can watch patients closely and start treatment early if needed.
Cold Agglutinin Disease
Cold Agglutinin Disease (CAD) is a rare condition where the body’s immune system attacks red blood cells at cold temperatures. This is due to cold agglutinins, special antibodies that cause red blood cells to clump together.
Distinguishing Features
CAD is different from other autoimmune diseases because of cold agglutinins. These are usually IgM antibodies. They stick to red blood cells when it’s cold, causing them to clump and break down.
People with CAD might notice their hands and feet turning blue or purple. They might also have a type of anemia. How bad the symptoms are can vary a lot.
Triggers and Associated Conditions
CAD can get worse when it’s cold. It might also be linked to infections, like Mycoplasma pneumoniae, or other diseases.
Knowing what triggers CAD is key to managing it. Staying warm can help some people feel better.
Cold Agglutinin Disease Life Expectancy
How long someone with CAD lives can depend on many things. This includes the cause, how bad the hemolysis is, and if they have other diseases.
Studies show that with the right treatment, many people can live active lives. CAD can affect their quality of life, but treatments have gotten better.
Managing CAD needs a full plan. This includes staying warm, treating other diseases, and sometimes using medicines to lower the amount of cold agglutinins.
Secondary vs. Primary AIHA
It’s important to know the difference between secondary and primary Autoimmune Hemolytic Anemia (AIHA). AIHA happens when the immune system attacks red blood cells, causing them to break down too early. The main difference is whether there’s an underlying condition that causes the disease.
Underlying Conditions That Cause Secondary AIHA
Secondary AIHA is linked to infections, autoimmune diseases, and cancers. These can make the immune system attack red blood cells.
- Infections like HIV, hepatitis, and some bacteria can cause secondary AIHA.
- Autoimmune diseases, such as SLE and rheumatoid arthritis, can also lead to secondary AIHA.
- Cancers, like lymphomas and leukemias, are another cause of secondary AIHA.
The table below lists some conditions linked to secondary AIHA:
| Category | Specific Conditions |
| Infections | HIV, Hepatitis, Bacterial infections |
| Autoimmune Diseases | SLE, Rheumatoid Arthritis |
| Malignancies | Lymphomas, Leukemias |
Idiopathic AIHA
Primary AIHA, or idiopathic AIHA, happens without a known cause. The immune system attacks red blood cells without a reason.
Managing idiopathic AIHA is tough because the cause is unknown. Treatment aims to stop the immune system from attacking red blood cells and manage symptoms.
Knowing the difference between secondary and primary AIHA is key for good treatment plans. Healthcare providers can tailor care based on whether AIHA is caused by another condition or is idiopathic.
Common Symptoms and Clinical Presentation
Knowing the signs of Autoimmune Hemolytic Anemia (AIHA) is key for early treatment. AIHA can show up in many ways, from mild anemia to severe hemolytic crises.
Early Warning Signs
The first signs of AIHA can be hard to spot. They might include feeling tired, short of breath, or having jaundice. These happen because the immune system attacks red blood cells too early.
- Fatigue and weakness due to anemia
- Shortness of breath, specially during physical activity
- Jaundice, which makes the skin and eyes turn yellow
- Pale skin from having fewer red blood cells
Severe Symptoms and Complications
As AIHA gets worse, symptoms can get much worse too. These might include:
- Increased heart rate and palpitations
- Dark urine from broken-down red blood cells
- An enlarged spleen, causing pain in the upper left abdomen
In extreme cases, AIHA can cause a hemolytic crisis. This is a serious condition that needs quick medical help.
Hemolytic Crisis
A hemolytic crisis is a serious emergency where red blood cells break down fast. Symptoms can include:
- Severe anemia
- High fever
- Severe jaundice
- Confusion or altered mental state
Quick treatment is vital to handle a hemolytic crisis and avoid serious problems.
Diagnosis and Evaluation
Diagnosing Autoimmune Hemolytic Anemia (AIHA) is a detailed process. It includes many tests and evaluations. We’ll explain how AIHA is diagnosed, focusing on the main tests and procedures.
Laboratory Tests
Laboratory tests are key in diagnosing AIHA. The main tests are:
- Direct Antiglobulin Test (DAT): Also known as the Coombs test, it’s a vital test for AIHA. It finds antibodies or complement proteins on red blood cells.
- Complete Blood Count (CBC): This test checks the levels of different blood cells. It shows how severe the anemia is.
- Reticulocyte Count: It measures young red blood cells in the blood. This shows how the bone marrow is responding to anemia.
- Lactate Dehydrogenase (LDH): High LDH levels suggest red blood cell destruction.
Imaging and Other Diagnostic Procedures
Imaging studies and other procedures help support the diagnosis. They also check how the condition affects the body.
- Imaging Studies: Studies like ultrasound or CT scans are not main tools for AIHA. But, they help rule out other conditions or check spleen size.
- Bone Marrow Biopsy: Sometimes, a bone marrow biopsy is done. It checks red blood cell production and rules out other bone marrow issues.
Differential Diagnosis
Differential diagnosis is important in diagnosing AIHA. It means ruling out other causes of hemolytic anemia. We look at other conditions that might cause similar symptoms and lab results, such as:
- Hereditary Spherocytosis: A genetic disorder affecting red blood cells.
- Membrane Disorders: Conditions that affect the red blood cell membrane.
- Other Autoimmune Disorders: Conditions like systemic lupus erythematosus (SLE) that can cause secondary AIHA.
By using clinical evaluation, lab tests, and sometimes imaging studies, we can accurately diagnose AIHA. We can also tell it apart from other conditions.
Treatment Approaches for AIHA
Treating AIHA is complex and involves many steps. It ranges from initial treatments to new therapies. Understanding AIHA and its treatments is key to managing it well.
First-Line Treatments
The first step in treating AIHA often includes corticosteroids like prednisone. These drugs aim to stop the immune system from attacking red blood cells. This helps lower hemolysis and boost hemoglobin levels.
Many patients see improvement with corticosteroids, sometimes even for a long time.
Second-Line Therapies
For those not helped by corticosteroids or needing them for a long time, immunosuppressive therapy is considered. Drugs like azathioprine or cyclophosphamide help control the immune system. Another choice is rituximab, a monoclonal antibody that targets B cells involved in the autoimmune process.
These treatments can work well, but they also have side effects and risks. These need careful management.
Emerging Treatment Options
Research into AIHA treatment is always advancing, with new options being explored. Targeted therapies are a promising area. They aim to fix the immune system’s problems without weakening it too much. Clinical trials are underway to check their safety and effectiveness.
As we learn more about AIHA, we’re finding new ways to treat it. This could lead to better results for patients.
Managing Complications of AIHA
Managing AIHA complications is key to better patient outcomes. Autoimmune Hemolytic Anemia can cause many issues. These range from sudden hemolytic crises to long-term problems like persistent anemia or organ damage.
Acute Complications
Acute AIHA complications, like hemolytic crisis, need quick medical help. A hemolytic crisis is when red blood cells are destroyed fast. This can cause severe anemia, jaundice, and serious health risks.
To tackle acute hemolytic crises, we use corticosteroids to lessen the immune system’s attack on red blood cells. In serious cases, hospital care is needed. This includes giving blood transfusions.
Chronic Complications
Chronic AIHA complications include ongoing anemia and organ damage from long-term hemolysis. Chronic hemolysis can also lead to iron overload. This can harm the heart, liver, and endocrine organs.
We keep a close eye on patients for signs of anemia, organ issues, and treatment side effects. We adjust treatment plans as needed. This helps manage AIHA while reducing long-term risks.
By tackling both acute and chronic complications, we can greatly improve AIHA patients’ lives. Our care plan is detailed. It tackles the complex needs of this condition.
Autoimmune Hemolytic Anemia Life Expectancy
Knowing how long people with autoimmune hemolytic anemia (AIHA) can live is key. AIHA is a rare disease where the body attacks and destroys red blood cells. This leads to anemia. The life expectancy depends on the type of AIHA, how well treatment works, and any other health issues.
Factors Affecting Prognosis
Many things can change how well someone with AIHA will do. These include the type of AIHA, whether it’s caused by another condition, how well the first treatment works, and any other health problems. People with AIHA caused by another condition might have a different outlook than those without.
How well treatment works is very important. Those who get better with the first treatment usually do better than those who need more or don’t get better.
Statistical Survival Rates
Survival rates for AIHA patients vary a lot. This depends on who is being studied and how they are diagnosed. But, thanks to new treatments, more people are living longer.
A study in a medical journal showed that the 5-year survival rate for primary AIHA was 70-80%. For secondary AIHA, it was 50-60%. But, these numbers can change based on the cause and the person’s health.
Differences Between AIHA Types
The type of AIHA really matters for how long someone can live. Warm AIHA, the most common, usually has a better outlook than cold AIHA. Cold AIHA, like cold agglutinin disease, often lasts longer and can lead to more serious problems.
It’s important for both patients and doctors to know these differences. This helps plan better care. By focusing on the specific type of AIHA, doctors can give more tailored care. This might help improve the patient’s life and how long they can live.
Special Considerations: AIHA in Children
Understanding AIHA in children is key to giving them the best care. Autoimmune Hemolytic Anemia in kids faces special challenges. These need a careful look at diagnosis and treatment.
Pediatric Presentation and Diagnosis
AIHA in kids shows up differently than in adults. Kids often have more severe symptoms like deep anemia, jaundice, and tiredness. To diagnose AIHA in kids, doctors use tests like the Direct Antiglobulin Test (DAT). This test finds antibodies or proteins on red blood cells.
Key Diagnostic Features in Children:
- Hemoglobin levels significantly below normal for age
- Elevated bilirubin levels indicating hemolysis
- Positive DAT result
Treatment Approaches for Children
Treatment for kids with AIHA is made just for them. It often starts with corticosteroids to lower antibody production. Sometimes, intravenous immunoglobulin (IVIG) is used to help the immune system not attack red blood cells.
“The management of AIHA in children requires a multidisciplinary approach, involving pediatric hematologists, immunologists, and other specialists to ensure complete care.” – Expert in Pediatric Hematology
Treatment Options:
| Treatment | Description | Use in Children |
| Corticosteroids | Reduce antibody production | Commonly used |
| IVIG | Modulate immune response | Used in specific cases |
| Blood Transfusion | Address severe anemia | Used cautiously |
Long-term Outlook
The future for kids with AIHA can vary. Some might fully recover, while others need ongoing care. It’s vital for kids to see a pediatric hematologist regularly. This helps keep an eye on their condition and adjust treatments as needed.
Supportive care is very important for kids with AIHA. This includes emotional support for the child and their family. By understanding AIHA in kids, doctors can give better care. This improves the life quality of young patients.
AIHA in Dogs and Other Animals
AIHA affects more than just humans. It impacts dogs and other animals around the world. Autoimmune Hemolytic Anemia in dogs and other animals is a serious condition. It happens when the immune system attacks and destroys the animal’s own red blood cells.
Immune-Mediated Hemolytic Anemia in Dogs
Immune-Mediated Hemolytic Anemia (IMHA) in dogs is when the immune system attacks the dog’s own red blood cells. This marks them for destruction. It leads to hemolysis, or the breaking down of red blood cells, causing anemia.
The exact cause of IMHA in dogs is often unknown. But it can be triggered by infections, medications, and underlying health conditions.
Common signs of IMHA in dogs include:
- Pale gums
- Lethargy
- Loss of appetite
- Rapid breathing
- Dark-colored urine
Treatment Options for Canine AIHA
Treating IMHA in dogs involves suppressing the immune system. This stops the destruction of red blood cells. The main treatments are:
- Corticosteroids: To reduce the immune system’s attack on red blood cells.
- Immunosuppressive drugs: For more severe cases or when corticosteroids are not effective.
- Blood transfusions: To replace lost red blood cells and stabilize the dog.
In some cases, dogs may need to be hospitalized. This is to manage severe anemia and prevent complications.
Prognosis for Pets with AIHA
The prognosis for dogs with IMHA varies. It depends on the condition’s severity, treatment response, and any underlying health issues. With the right treatment, some dogs can recover. Others may need ongoing management.
Pet owners should closely work with their veterinarian. They need to monitor their dog’s condition and adjust treatment as needed.
Living with Autoimmune Hemolytic Anemia
Managing AIHA is a big job. It needs medical treatment, lifestyle changes, and emotional support. Understanding how AIHA affects daily life is key.
Lifestyle Adjustments
Living with AIHA means big changes. Staying away from things that make symptoms worse is important. For example, people with cold agglutinin disease should avoid cold.
Eating right and drinking plenty of water is also key. A diet full of iron, vitamin B12, and folate helps make red blood cells. Talking to a doctor or nutritionist about your diet is a good idea.
Monitoring and Follow-up Care
Keeping an eye on your health is critical. Working with your healthcare team to check your condition and change treatments is important. This might mean regular blood tests to watch for anemia and other issues.
| Monitoring Parameter | Frequency | Purpose |
| Complete Blood Count (CBC) | Every 1-3 months | To assess anemia and hemolysis |
| Lactate Dehydrogenase (LDH) | Every 1-3 months | To evaluate hemolysis |
| Direct Antiglobulin Test (DAT) | As needed | To diagnose and monitor AIHA |
Coping Strategies
Dealing with AIHA is not just about medicine. It’s also about emotional and mental support. Meeting others with AIHA can be really helpful. Support groups online or in person offer a sense of community.
Stress-reducing activities like meditation, yoga, or deep breathing can help. It’s also good to know a lot about your condition and treatment options. This way, you can feel more in control.
Related Conditions: Evans Syndrome and Beyond
Evans syndrome is a rare condition that combines AIHA and immune thrombocytopenia. It shows the wide range of autoimmune blood disorders. This syndrome is complex and poses challenges in diagnosis and treatment.
Evans Syndrome Life Expectancy
The life expectancy for those with Evans syndrome varies. It depends on the condition’s severity, treatment response, and any underlying conditions. Research shows that outcomes can differ greatly, with some patients facing a long-term battle and others severe complications.
Several factors affect life expectancy:
- The success of initial treatment and ongoing management
- Presence of other conditions that make treatment harder
- The patient’s overall health and immune system strength
Other Autoimmune Blood Disorders
There are many other autoimmune blood disorders to know about. These include:
- Immune thrombocytopenia (ITP): Low platelet counts due to immune destruction.
- Autoimmune neutropenia: The immune system attacks neutrophils, a white blood cell type.
- Antiphospholipid syndrome (APS): An autoimmune disorder that can cause blood clots.
Knowing about these related conditions is key for effective patient care. Recognizing the wide range of these diseases helps healthcare providers tailor treatments. This ensures each patient gets the care they need.
Research and Future Directions
Research into Autoimmune Hemolytic Anemia (AIHA) is leading to new treatments and a better understanding of the condition. As we dive deeper into AIHA, it’s clear that ongoing research is key to finding effective therapies.
Current Clinical Trials
Many clinical trials are underway to find new treatments for AIHA. These trials are vital for checking if new therapies are safe and work well. For example, researchers are looking at rituximab, a drug that targets B cells, for AIHA treatment.
Some main areas in these trials include:
- Testing new immunosuppressive drugs
- Checking if biologics are safe and effective for AIHA
- Looking into stem cell transplantation for severe AIHA cases
Promising Therapeutic Approaches
New ways to treat AIHA are also being explored. One area is developing targeted therapies that only affect the immune system. For instance, complement inhibitors might help reduce hemolysis in AIHA patients.
Another area is gene therapy to fix the immune system problems that cause AIHA. Gene therapy is very early but could potentially cure AIHA or greatly change its course.
Genetic Research
Genetic research is key to understanding AIHA. It helps find genetic links and the disease’s causes. This research leads to more tailored treatments and better patient results.
Recent studies show genetic factors are important in AIHA. They involve genes related to the immune system and red blood cell production. More genetic research is needed to find new therapy targets and understand AIHA better.
Conclusion
Autoimmune hemolytic anemia (AIHA) is a complex condition. It happens when the immune system attacks red blood cells, causing them to break down early. Our overview of AIHA shows how different it can be, highlighting the need for detailed management plans.
We’ve looked at the different types of AIHA, like warm autoimmune hemolytic anemia and cold agglutinin disease. We’ve also talked about the causes, symptoms, and treatments. Knowing about AIHA is key for both patients and healthcare providers to handle the condition well.
Our goal is to give people the knowledge they need to deal with AIHA. The outlook for people with AIHA depends on many things. These include the cause, how well they respond to treatment, and if they have any complications.
FAQ
What is Autoimmune Hemolytic Anemia (AIHA)?
AIHA is when your immune system attacks and destroys red blood cells. This leads to anemia.
What are the types of Autoimmune Hemolytic Anemia?
There are two main types: Warm Autoimmune Hemolytic Anemia and Cold Agglutinin Disease. Each has its own causes and symptoms.
How is AIHA diagnosed?
Doctors use tests like the direct antiglobulin test (DAT) and complete blood count (CBC). These help find autoantibodies against red blood cells.
What are the symptoms of AIHA?
Symptoms can be mild or severe. They include fatigue, jaundice, dark urine, and shortness of breath. These happen because of fewer red blood cells.
How is AIHA treated?
Treatment starts with corticosteroids. If that doesn’t work, doctors might use immunosuppressive drugs. In some cases, surgery or new treatments are considered.
What is the life expectancy for someone with AIHA?
Life expectancy varies. It depends on the type of AIHA, how well treatment works, and any other health issues. Survival rates give a general idea, but each case is different.
Can AIHA be cured?
Some people can go into long-term remission. But AIHA is often a chronic condition. The chance of a cure depends on the cause and treatment response.
How does AIHA affect children?
Children with AIHA face unique challenges. Diagnosis, treatment, and outlook can differ from adults.
Can dogs get AIHA?
Yes, dogs can get Immune-Mediated Hemolytic Anemia (IMHA). It’s similar to AIHA in humans. Dogs have treatment options and prognostic factors.
What lifestyle adjustments can help manage AIHA?
Patients can monitor their condition and follow up with doctors. Avoiding triggers and using coping strategies can improve life quality.
What is Evans Syndrome?
Evans Syndrome combines AIHA and immune thrombocytopenia. It has its own challenges and management strategies.
Are there ongoing research and new treatments for AIHA?
Yes, research is ongoing. Clinical trials and new treatments, including genetic research, aim to improve AIHA outcomes.
How does Cold Agglutinin Disease impact life expectancy?
Cold Agglutinin Disease, a form of AIHA, has its own characteristics. These can affect life expectancy.
References:
Hansen DL, Möller S, Frederiksen H. Survival in autoimmune hemolytic anemia remains poor, results from a nationwide cohort with 37 years of follow-up. Eur J Haematol. 2022 Mar 18. doi:10.1111/ejh.13764. Retrieved from








