Last Updated on October 21, 2025 by mcelik

Hematologic disorders affect millions of people worldwide. They have a big impact on their quality of life. These conditions involve abnormalities in the blood, leading to health problems if not treated.
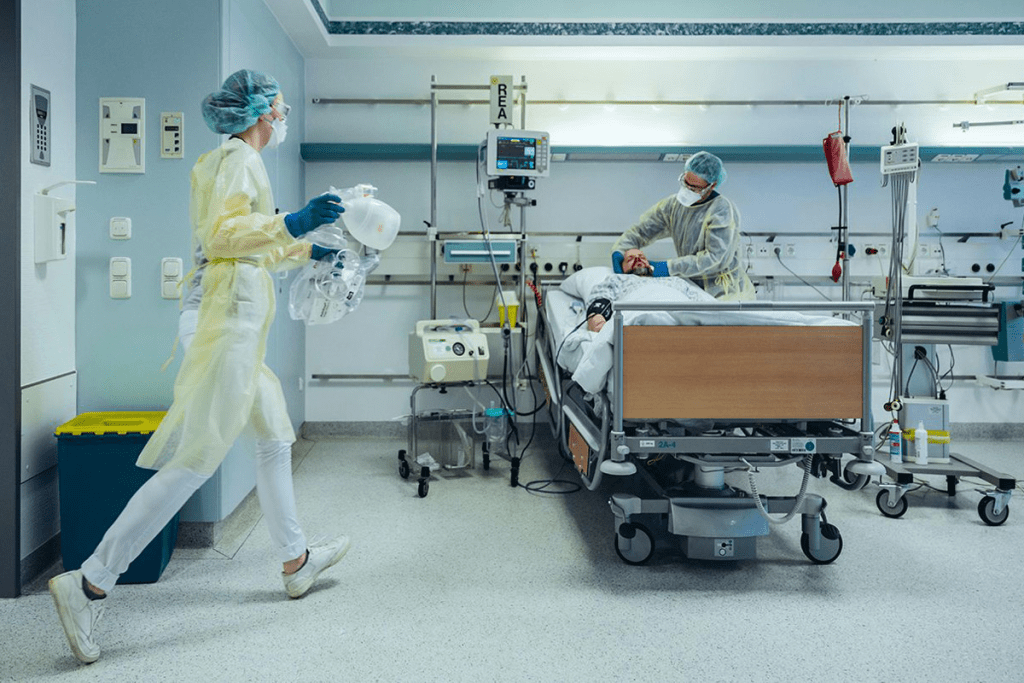
It’s vital to understand hematologic disorders. They can be deadly if not caught and treated early. Hematologists are key in diagnosing and treating these conditions. They use the latest medical techniques and therapies.
Knowing the causes, symptoms, and treatments for hematologic disorders helps manage them. This improves patient outcomes.
Hematology is all about studying, diagnosing, and treating blood disorders. It’s a key part of healthcare. It deals with the details of blood, including red and white blood cells and platelets.
Hematology is a branch of medicine that focuses on blood and its disorders. It also looks at the organs that make blood. Hematologists are experts who have learned a lot about blood and its problems.
“The study of blood is not just about treating diseases; it’s about understanding the very fabric of our being,” says a renowned hematologist. This quote shows how important hematology is in healthcare.
Healthy blood is key for our health. It carries oxygen, fights infections, and helps fix damaged tissues. Blood disorders can really affect our health and life quality. So, knowing how vital healthy blood is helps us see why hematology matters.
| Component | Function |
| Red Blood Cells | Carry oxygen throughout the body |
| White Blood Cells | Fight infections and diseases |
| Platelets | Help in blood clotting to prevent excessive bleeding |
A hematologist is a doctor who deals with blood disorders. They use tests like blood counts and bone marrow biopsies to find problems. They create treatment plans that might include medicine, blood transfusions, or other therapies.
Hematologists do more than just treat. They help patients manage their conditions and stay healthy.
Blood is made up of several important parts, each with a key role in keeping us healthy. The main parts are red blood cells, white blood cells, platelets, and plasma. Knowing about these parts and what they do is key to understanding and treating blood disorders.
Red blood cells, or erythrocytes, are the most common cells in blood. They carry oxygen from the lungs to our body’s tissues and carbon dioxide back to the lungs. This is thanks to hemoglobin, a protein in them that binds to oxygen. These cells are made in the bone marrow and live for about 120 days.
Here are some key functions of red blood cells:
White blood cells, or leukocytes, are vital for our immune system. They fight infections by attacking and destroying harmful substances like bacteria and viruses. There are different types of white blood cells, each with its own role.
The main functions of white blood cells include:
Platelets, or thrombocytes, are small, colorless cell fragments that are key in blood clotting. When we bleed, platelets gather at the injury site, forming a plug to stop the bleeding. They also release chemicals that attract more platelets and clotting factors, helping to form a blood clot.
Key functions of platelets include:
Plasma is the liquid part of blood, making up about 55% of it. It’s mostly water, with proteins, nutrients, hormones, gases, waste products, and ions making up the rest. Plasma carries cells, proteins, and other substances throughout the body.
Clotting factors are proteins in plasma that are vital for blood coagulation. They work with platelets to form blood clots and stop bleeding. Key clotting factors include fibrinogen, prothrombin, and other clotting proteins.
The main functions of plasma include:
Hematologic disorders affect the blood and bone marrow. They can greatly change a person’s life and health.
These disorders are divided into several types. These include anemia, bleeding disorders, clotting disorders, and cancers of the blood. Knowing these types helps doctors diagnose and treat them.
Blood disorders are a big health issue in the U.S. Millions of Americans have these conditions. For example, anemia affects about 3 million, and sickle cell disease impacts around 100,000.
This shows we need to be aware and manage these conditions well. Knowing the risks and how to prevent them is key.
Many things can lead to blood disorders. These include genetics, the environment, and lifestyle. Knowing these risk factors helps prevent them.
To prevent these disorders, we should eat well, avoid harmful things, and get regular check-ups. Early detection and treatment can make a big difference for those with blood disorders.
“Early diagnosis and proper management of hematologic disorders can greatly enhance the quality of life for affected individuals.”
” Expert Hematologist
Understanding hematologic disorders helps us tackle them better. This knowledge improves patient care and outcomes.
Anemia is a common blood disorder that affects millions worldwide. It makes it hard for the body to carry oxygen. This happens because there are not enough red blood cells or they are not good enough.
Iron deficiency anemia is the most common type. It happens when the body doesn’t have enough iron. This is needed to make hemoglobin, a key part of red blood cells. Causes include not eating enough iron, losing blood too much, and needing more iron during pregnancy. Symptoms include feeling very tired, weak, and short of breath.
To treat it, people often take iron supplements and eat more iron-rich foods. Sometimes, finding and fixing the cause of the iron loss is also important.
Vitamin B12 deficiency anemia happens when the body can’t absorb enough vitamin B12. This is more common in older adults and people who don’t eat meat or animal products. Symptoms include feeling tired, having neurological problems, and digestive issues.
Treatment involves getting vitamin B12 injections or taking supplements. It’s also important to eat foods that have enough vitamin B12.
Folate deficiency anemia is caused by not having enough folate. Folate is important for making red blood cells. Causes include eating poorly, taking certain medicines, and needing more folate during pregnancy. Symptoms are similar to iron deficiency anemia.
Treatment includes taking folate supplements and eating more folate-rich foods. It’s also key to fix any underlying causes.
Hemolytic anemia is when red blood cells break down too early. Causes can be genetic, infections, or certain medicines. Symptoms include jaundice, feeling tired, and shortness of breath.
Treatment varies based on the cause. It might include medicines to slow down red blood cell breakdown, removing the spleen in some cases, and managing symptoms.
| Type of Anemia | Causes | Symptoms | Treatment |
| Iron Deficiency Anemia | Inadequate iron intake, chronic blood loss | Fatigue, weakness, shortness of breath | Iron supplementation, dietary adjustments |
| Vitamin B12 Deficiency Anemia | Malabsorption, dietary restrictions | Fatigue, neurological changes, digestive issues | Vitamin B12 injections or supplements |
| Folate Deficiency Anemia | Poor diet, certain medications, pregnancy | Similar to iron deficiency anemia | Folate supplementation, dietary changes |
| Hemolytic Anemia | Genetic disorders, infections, medications | Jaundice, fatigue, shortness of breath | Depends on cause; may include medications, splenectomy |

It’s important to know about sickle cell disease and other hemoglobinopathies. These are genetic disorders that affect how hemoglobin works. Hemoglobin is key for carrying oxygen in our blood.
Sickle cell disease comes from a gene mutation. This mutation changes the beta-globin subunit of hemoglobin. It makes abnormal hemoglobin that changes shape under low oxygen, causing red blood cells to become misshapen and rigid.
These sickled red blood cells are more likely to be destroyed. This leads to anemia. They can also block small blood vessels, causing pain and other problems.
The disease is complex. It involves hemolysis, vaso-occlusion, and inflammation. It’s not just about sickled red blood cells. It also involves many other cellular and molecular pathways.
Thalassemias are caused by mutations in the alpha-globin or beta-globin chains of hemoglobin. Alpha-thalassemia happens when there’s a mutation or deletion in one or more alpha-globin genes. Beta-thalassemia results from mutations in both beta-globin genes.
The severity of thalassemia depends on how many genes are affected. It can range from mild anemia to severe conditions that need frequent blood transfusions.
Managing thalassemias often includes blood transfusions and iron chelation therapy. Bone marrow transplantation may also be an option. Genetic testing has improved prenatal diagnosis and counseling for families at risk.
There are other hemoglobin variants that can cause health problems. For example, Hemoglobin C disease and Hemoglobin E disease can lead to hemolytic anemia. The symptoms can vary widely, and diagnosis requires several tests.
It’s vital to understand these hemoglobinopathies for proper care. We need to know their genetic basis, symptoms, and treatment options. This helps improve outcomes for patients with these conditions.
Blood clotting disorders include hemophilia, von Willebrand disease, and deep vein thrombosis. Each has its own causes and symptoms. These conditions affect how the body makes blood clots, which are vital for stopping bleeding when a blood vessel is hurt.
Hemophilia is a genetic disorder that makes blood unable to clot properly. This leads to prolonged bleeding. The most common types are Hemophilia A and Hemophilia B, caused by a lack of clotting factors VIII and IX, respectively.
Causes and Symptoms: Hemophilia is usually inherited. Symptoms include frequent bruising, joint pain and swelling from bleeding into the joints, and prolonged bleeding after injuries or surgery.
Von Willebrand disease is a bleeding disorder caused by a lack or mutation of von Willebrand factor. It’s the most common inherited bleeding disorder.
Symptoms and Treatment: Symptoms include easy bruising, heavy menstrual periods, and bleeding after childbirth or surgery. Treatment often involves replacing von Willebrand factor through infusion of clotting factor concentrates.
Deep vein thrombosis (DVT) is a condition where a blood clot forms in a deep vein, usually in the legs. It can be life-threatening if the clot breaks loose and travels to the lungs, causing a pulmonary embolism.
Risk Factors and Symptoms: Risk factors include prolonged immobility, cancer, and genetic predispositions. Symptoms include swelling, pain, and redness in the affected limb.
A pulmonary embolism occurs when a blood clot lodges in the lungs’ blood vessels, blocking blood flow. It is a medical emergency requiring immediate attention.
Symptoms and Treatment: Symptoms include sudden shortness of breath, chest pain, and coughing up blood. Treatment involves anticoagulant medications to prevent further clotting and, in severe cases, thrombolytic therapy to dissolve the clot.
| Condition | Causes | Symptoms | Treatment |
| Hemophilia | Genetic deficiency in clotting factors VIII or IX | Prolonged bleeding, joint pain, bruising | Replacement therapy with clotting factors |
| Von Willebrand Disease | Deficiency or mutation in von Willebrand factor | Easy bruising, heavy menstrual periods | Replacement therapy with von Willebrand factor |
| Deep Vein Thrombosis | Prolonged immobility, cancer, genetic predispositions | Swelling, pain, redness in the affected limb | Anticoagulant therapy |
| Pulmonary Embolism | Breakage of DVT clot | Sudden shortness of breath, chest pain | Anticoagulant therapy, thrombolytic therapy |
Platelet disorders affect how platelets work in our blood. Platelets are key for blood clotting. Any problem with them can cause serious health issues, like too much bleeding or clotting.
Thrombocytopenia means you have too few platelets. It can happen for many reasons, like bone marrow problems or certain medicines. Symptoms include easy bruising, cuts that won’t stop bleeding, and sometimes, internal bleeding. Doctors use a blood test to find out if you have it. Treatment depends on why it’s happening.
ITP is when your immune system attacks and destroys platelets. This can make your platelet count very low. Treatment includes medicines to calm down your immune system, drugs to suppress it, or sometimes, removing part of your spleen. Managing ITP means keeping an eye on your platelet count and adjusting treatment as needed.
Thrombocytosis means you have too many platelets. It can be due to a bone marrow issue or another condition like an infection. Having too many platelets can raise your risk of blood clots. Treatment might involve fixing the cause or using medicines to lower your platelet count.
Platelet function disorders happen when platelets don’t clot blood right. These can be inherited or caused by other conditions. Tests like platelet aggregometry help diagnose them. Treatment might include medicines to help platelets work better or prevent bleeding.
Handling platelet disorders needs a team effort from doctors, including hematologists and primary care physicians. By finding and treating these issues, we can greatly improve life for those with platelet disorders.
It’s important to know about white blood cell disorders to treat them well. These cells are key to our immune system, fighting infections and diseases. Problems with these cells can cause health issues, from mild to serious.
Neutropenia means you have too few neutrophils, a type of white blood cell. Causes of neutropenia include bone marrow issues, some medicines, and severe infections. Treatment aims to fix the cause and prevent infections.
Leukocytosis is when you have too many white blood cells. This can happen due to infections, inflammation, or other reasons. Finding the cause is key to managing it. This might involve more tests to figure out why your white blood cell count is high.
Lymphocytopenia is when you have too few lymphocytes, another white blood cell type. It can be caused by infections, medicines, or immune system problems. Treatment aims to fix the cause and manage any immune issues.
Eosinophilic disorders involve abnormal eosinophil levels. Eosinophils fight parasites and allergic reactions. Causes include parasitic infections, allergies, or other factors. Treatment focuses on the cause and may include medicines to lower eosinophil levels.
White blood cell disorders can greatly affect health. Understanding these conditions is vital for proper diagnosis and treatment. By addressing the causes and using the right treatments, healthcare can help patients live better lives.
Hematologic malignancies are different types of blood cancers. Each has its own traits and treatment methods. These cancers affect the blood, bone marrow, and lymphatic system, changing how blood cells are made and work.
Leukemia is a blood and bone marrow cancer. It happens when white blood cells grow too much. Symptoms can be tiredness, infections, and bleeding problems.
Diagnosis: Doctors use blood tests, bone marrow biopsies, and genetic tests to find leukemia. Treatment includes chemotherapy, targeted therapy, and stem cell transplants.
Lymphoma is a cancer of the lymphatic system. It’s divided into Hodgkin and non-Hodgkin lymphoma. Symptoms include swollen lymph nodes, fever, and weight loss.
Treatment Approaches: Lymphoma treatment varies by type and stage. It can range from watching it closely to chemotherapy, radiation, and immunotherapy.
Multiple myeloma is a cancer of plasma cells in the bone marrow. It causes bone pain, anemia, and makes infections more likely.
Management: Treatment for multiple myeloma includes targeted therapy, chemotherapy, corticosteroids, and stem cell transplants.
Myelodysplastic syndromes (MDS) are disorders of blood cells. They often lead to acute myeloid leukemia.
Treatment Options: MDS treatment includes supportive care, immunotherapy, and sometimes stem cell transplants.
| Type of Malignancy | Characteristics | Common Symptoms | Treatment Approaches |
| Leukemia | Cancer of blood and bone marrow | Fatigue, infections, bleeding | Chemotherapy, targeted therapy, stem cell transplantation |
| Lymphoma | Malignancy of the lymphatic system | Lymphadenopathy, fever, weight loss | Chemotherapy, radiation, immunotherapy |
| Multiple Myeloma | Plasma cell malignancy | Bone pain, anemia, infections | Targeted therapy, chemotherapy, stem cell transplantation |
| Myelodysplastic Syndromes | Dysfunctional blood cells | Anemia, infections, bleeding | Supportive care, immunotherapy, stem cell transplantation |
Diagnosing blood disorders requires a mix of clinical checks and lab tests. Getting the right diagnosis is key for good treatment and care. We’ll look at the different tests used to spot blood disorders.
A CBC is a basic test that looks at blood parts like red and white cells, and platelets. It tells us a lot about a person’s health and can spot issues like anemia, infections, and leukemia.
Key parts of a CBC include:
A blood smear test looks at a blood sample under a microscope. It helps find problems like sickle cell disease, malaria, and infections.
The blood smear test is great for:
A bone marrow biopsy takes a small bone marrow sample for study. It’s used to find conditions like leukemia, lymphoma, and multiple myeloma.
The steps are:
Genetic testing looks at DNA to find genetic changes that cause blood disorders. It helps diagnose sickle cell disease, thalassemia, and other genetic issues.
Genetic testing can:
Here’s a quick rundown of the tests we talked about:
| Diagnostic Test | Purpose | Conditions Diagnosed |
| Complete Blood Count (CBC) | Measures various blood components | Anemia, infection, leukemia |
| Blood Smear Examination | Identifies abnormalities in blood cells | Sickle cell disease, malaria, infections |
| Bone Marrow Biopsy | Examines bone marrow tissue | Leukemia, lymphoma, multiple myeloma |
| Genetic Testing | Analyzes DNA for genetic mutations | Sickle cell disease, thalassemia, genetic disorders |
Knowing when to see a hematologist is key for those with blood disorder symptoms. Hematologists deal with blood, bone marrow, and the lymphatic system. They diagnose and treat related conditions.
Some symptoms mean you should see a hematologist. These include constant tiredness, frequent infections, easy bruising, and swollen lymph nodes. If you notice these, talk to your primary care doctor first. They might send you to a hematologist.
Other signs that mean a hematologist visit are needed include anemia, blood clots, and odd blood test results. Conditions like sickle cell disease, hemophilia, and certain cancers also need hematologist care.
Usually, a hematologist visit starts with a referral from your primary care doctor. If your doctor thinks you might have a blood disorder or if your symptoms don’t go away, they’ll suggest a specialist. You can also ask to see a hematologist if you’re worried about your symptoms.
Your first visit to a hematologist will be thorough. You’ll share your medical history, get a physical check-up, and possibly some tests like blood counts or bone marrow biopsies. The hematologist will then figure out what’s wrong and plan your treatment.
It’s smart to prepare for your appointment. Write down your symptoms, any questions, and your current medications. This helps your hematologist understand your situation better.
Being ready with questions is important for your appointment. Here are some examples:
Asking these questions helps you understand your condition better. It ensures you’re getting the right care.
Managing blood disorders well needs a deep understanding of different treatments. These disorders include anemia, leukemia, lymphoma, and bleeding issues. Each one needs a special treatment plan.
Medicines play a big role in treating many blood disorders. They help control symptoms, prevent problems, and make life better. For example, iron chelation therapy helps those with too much iron from blood transfusions. Anticoagulants stop blood clots in people at risk.
Some common medicines are:
Blood transfusions are key for treating many blood disorders. They give blood parts like red cells, platelets, or plasma to replace what’s missing. For severe anemia, red cell transfusions help tissues get enough oxygen.
| Blood Component | Indication | Benefits |
| Red Blood Cells | Severe anemia, significant blood loss | Improves oxygen delivery to tissues |
| Platelets | Thrombocytopenia, platelet dysfunction | Reduces risk of bleeding |
| Plasma | Clotting factor deficiencies, severe burns | Replaces clotting factors, improves coagulation |
Stem cell transplantation, or bone marrow transplant, can cure some blood disorders like leukemia and lymphoma. It replaces the patient’s bad bone marrow with healthy stem cells from a donor.
Types of Stem Cell Transplantation:
Hematology is growing fast, with new treatments on the horizon. Gene therapy tries to fix genetic problems in blood disorders. Other new treatments include new medicines and immunotherapies.
As research keeps improving, we’ll see more new treatments for blood disorders. This brings hope to patients and their families.
Living with chronic blood disorders can be tough, but it’s possible to live well with the right help. These conditions need ongoing care to avoid serious problems and improve life quality.
Changing your lifestyle can really help manage chronic blood disorders. Regular exercise is key, but it must fit your health and abilities.
Stress management is also vital. Stress can make some conditions worse. Try meditation, yoga, or deep breathing to help.
Eating right is critical for those with chronic blood disorders. The right foods can help control symptoms and prevent issues. For example, people with iron deficiency anemia should eat more iron-rich foods.
“A healthy diet is fundamental in managing chronic blood disorders. It’s not just about managing the condition but also about improving overall well-being.”
” A Hematologist
Having support can greatly improve life for those with chronic blood disorders. This includes groups, counseling, and educational materials.
Managing complications is a big part of living with chronic blood disorders. Regular check-ups and monitoring are vital.
Knowing the signs of complications and when to get help is important. For example, people with clotting disorders should watch for signs of blood clots.
By being proactive, you can live a full and active life despite your condition.
Understanding hematologic disorders is key to managing and treating them. Conditions like anemia and sickle cell disease need a detailed approach. Each disorder has its own set of challenges.
Hematologists play a crucial role in diagnosing blood disorders and tailoring advanced treatments to each patient’s needs. Early detection and personalized treatment plans can greatly improve patient outcomes.
It’s important to keep learning about hematology and blood disorders. We must stay updated on new treatments and technologies. This way, we can offer the best care and improve the lives of those affected.
Hematology is the study of blood and blood disorders. It deals with diagnosing, treating, and managing blood cell issues. This includes red and white blood cells, platelets, and plasma.
Common blood disorders include anemia, sickle cell disease, and hemophilia. Others are thrombocytopenia, leukemia, lymphoma, and multiple myeloma.
A hematologist is a specialist who treats blood disorders. They manage conditions like anemia, bleeding disorders, and blood cancers.
Symptoms vary but can include fatigue, weakness, and pale skin. Shortness of breath, bruising, and bleeding are also signs. Recurrent infections are another symptom.
Tests like complete blood count (CBC) and blood smear examination are used. Bone marrow biopsy and genetic testing are also part of the diagnosis.
A CBC measures the levels of blood cells. It checks red and white blood cells and platelets in the blood.
Anemia is when there’s not enough red blood cells or hemoglobin. It causes fatigue, weakness, and shortness of breath.
Treatment depends on the disorder. Options include medication, blood transfusions, stem cell transplantation, and new treatments.
See a hematologist if you have symptoms like fatigue, bruising, or bleeding. Or if you’ve been diagnosed with a blood condition.
At your first visit, your hematologist will take your medical history and perform a physical exam. They may order tests to find out what’s causing your symptoms.
Managing chronic blood disorders involves lifestyle changes and nutrition. There are also support resources and ways to handle complications.
Stem cell transplantation can save lives for conditions like leukemia and lymphoma. It replaces damaged stem cells with healthy ones.
Blood transfusions have risks like transfusion reactions and infectious disease transmission. Iron overload is another risk.
Some blood disorders can’t be prevented, but others can be managed or prevented. Lifestyle changes like a healthy diet and regular check-ups help.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!