Blood cancers affect the blood, bone marrow, and lymphatic system. They impact thousands of people globally. Leukemia, lymphoma, and multiple myeloma which type of blood cancer is most dangerous. Each has its own challenges and survival rates.
It’s important to understand these diseases to find the most deadly cancer. We need to improve the blood cancer survival rate. We’ll look at what makes these cancers hard to treat.
Key Takeaways
- Blood cancers include leukemia, lymphoma, and multiple myeloma.
- Each type of blood cancer has its unique challenges and survival rates.
- Understanding the complexities of blood cancers is key for effective treatment.
- The blood cancer survival rate varies significantly among different types.
- Determining the most deadly cancer among blood cancers requires a detailed analysis.
Understanding Blood Cancers: An Overview
Blood cancers, also known as hematologic malignancies, affect the blood and bone marrow. They are divided into leukemia, lymphoma, and multiple myeloma. Each type has its own set of challenges.
What Defines Blood Cancer
Blood cancer is when abnormal blood cells grow out of control. This can cause problems like anemia, infections, and bleeding issues.
Genetic mutations often lead to blood cancer. These can come from genes, chemicals, or viruses.
How Blood Cancers Differ from Solid Tumors
Blood cancers spread throughout the body, unlike solid tumors. This makes them harder to diagnose and treat.
They affect many systems and organs. Blood cancers are classified by the type of blood cell and how fast they grow. Leukemia, lymphoma, and multiple myeloma need different treatments.
| Type of Blood Cancer | Description | Common Symptoms |
| Leukemia | Cancer of the blood cells, often starting in the bone marrow. | Fatigue, weight loss, frequent infections. |
| Lymphoma | Cancer of the lymphatic system, which is part of the immune system. | Swollen lymph nodes, fever, night sweats. |
| Multiple Myeloma | Cancer of plasma cells, a type of white blood cell. | Bone pain, anemia, kidney problems. |
Knowing the different blood cancers is key to better treatment. Healthcare providers can then tailor therapies for each patient.
The Major Categories of Blood Cancer
Blood cancers are divided into several main types. Each type has its own traits and treatment methods. Knowing these categories helps both patients and doctors understand blood cancer better.
Leukemia: Cancer of the Blood Cells
Leukemia affects the blood cells, starting in the bone marrow. It causes too many white blood cells to grow, leading to problems like anemia and infections. There are different types of leukemia, like acute myeloid leukemia (AML) and chronic lymphocytic leukemia (CLL).
Lymphoma: Cancer of the Lymphatic System
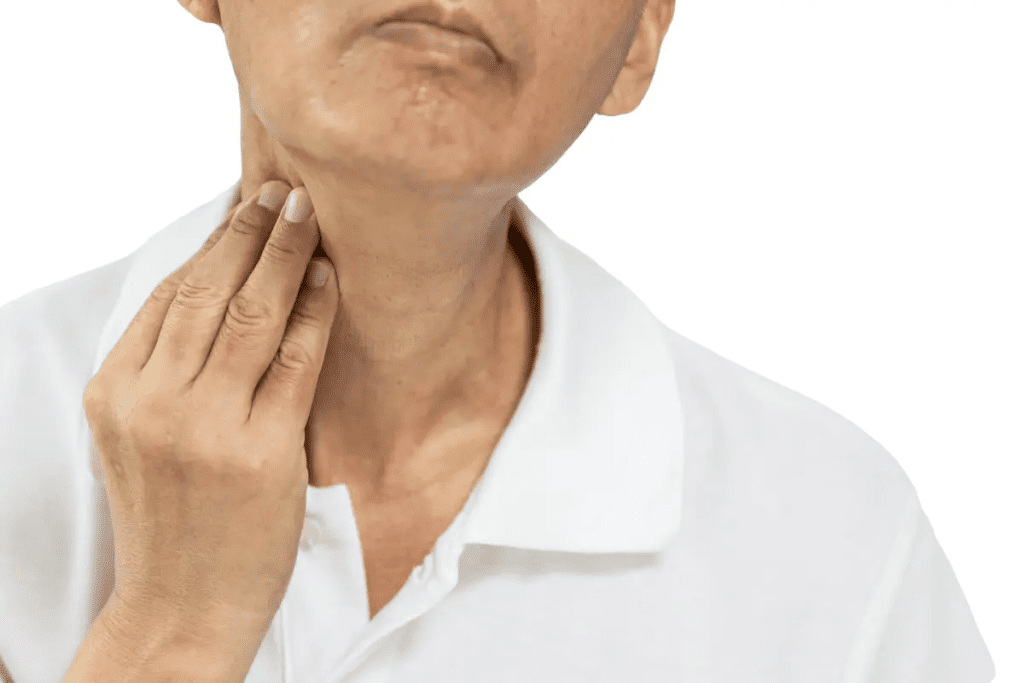
Lymphoma is a cancer of the immune system’s lymphatic system. It happens when lymphocytes grow out of control. There are two main types: Hodgkin lymphoma and non-Hodgkin lymphoma. Symptoms include swollen lymph nodes and fever.
Multiple Myeloma: Cancer of Plasma Cells
Multiple myeloma affects plasma cells, which make antibodies. In this cancer, plasma cells grow in the bone marrow, harming bones and blood cell production. Symptoms include bone pain and infections.
Myelodysplastic Syndromes (MDS)
Myelodysplastic syndromes (MDS) are disorders with poorly formed blood cells. They can turn into acute myeloid leukemia (AML). Symptoms include anemia and infections. Treatment depends on the type and risk of turning into AML.
Which Type of Blood Cancer is Most Dangerous: Factors That Determine Severity
Several key factors affect how severe blood cancer is. These factors help doctors decide the best treatment and tell patients what to expect. Knowing these factors is very important.
Cellular Origin and Biology
The type of blood cell that turns cancerous is a big deal. Different cells behave differently when they become cancerous. For which type of blood cancer is most dangerousexample, leukemia starts in bone marrow cells, while lymphoma begins in lymphocytes.
The specific genetic changes in these cells also matter. They can make the cancer more aggressive or harder to treat.
Rate of Progression
How fast blood cancer grows is another important factor. Some cancers, like CLL, grow slowly. Others, like AML, can grow quickly if not treated right away.
This speed affects how doctors choose treatments and what the patient’s outcome might be.
Response to Treatment
How well a blood cancer responds to treatment is key. Some cancers get better with the first treatment, while others are harder to treat. The success of treatment can greatly improve survival chances and quality of life.
Risk of Relapse
The chance of the cancer coming back is a big worry. Some cancers are more likely to come back after treatment. Knowing this helps doctors plan follow-up care to catch any recurrence early.
| Factor | Impact on Severity | Example |
| Cellular Origin | Influences cancer behavior and treatment response | Leukemia vs. Lymphoma |
| Rate of Progression | Affects treatment urgency and patient outcomes | CLL vs. AML |
| Response to Treatment | Impacts survival rates and quality of life | Highly responsive vs. resistant cancers |
| Risk of Relapse | Influences follow-up care and monitoring | High-risk vs. low-risk relapse scenarios |
Understanding these factors helps us see how severe blood cancer is for each patient. It helps us create better treatment plans. The mix of these factors shows how complex blood cancer is and why we need care that’s tailored to each person.
Acute Myeloid Leukemia (AML): One of the Most Challenging Blood Cancers
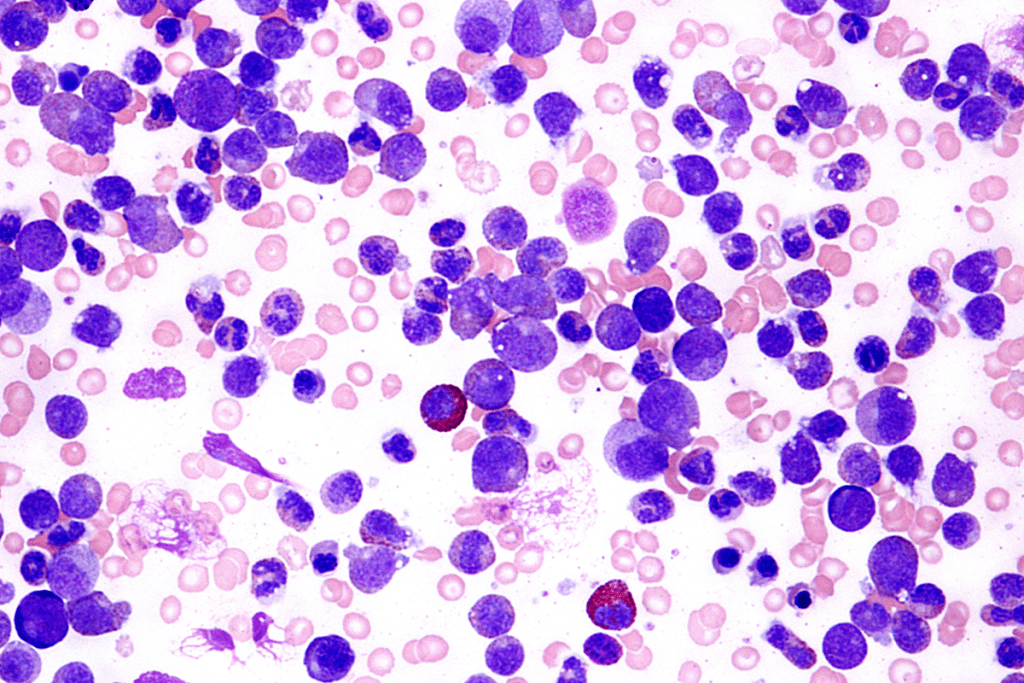
Acute Myeloid Leukemia (AML) is a very aggressive blood cancer. It’s hard to treat because of its fast growth. Abnormal white blood cells fill the bone marrow, stopping normal blood cell production.
Why AML is Difficult to Treat
AML is tough to treat for many reasons. It’s a disease that changes a lot from person to person. This makes it hard to find one treatment that works for everyone.
Also, AML often hits older adults. They might have other health problems that make treatment harder. The disease can cause serious infections and bleeding because it stops normal blood cells from working.
Key Challenges in Treating AML:
- Genetic heterogeneity
- Age-related comorbidities
- Risk of severe infections and bleeding
Survival Rates and Prognosis
The outlook for AML patients varies a lot. It depends on age, the leukemia’s genetics, and how well the patient responds to treatment. Generally, about 40% of AML patients live five years or more. But, this number is much lower for older patients or those with certain genetic traits.
| Age Group | Five-Year Survival Rate |
| 20-39 years | around 60% |
| 40-59 years | around 45% |
| 60 years and older | around 10% |
Treatment Challenges Specific to AML
Treating AML is hard because it grows fast and needs quick action. The usual treatment is strong chemotherapy, which can have big side effects. Many patients also develop resistance to chemotherapy, leading to relapse.
New treatments like targeted therapies and immunotherapies offer hope for AML patients. But, these treatments are new and need more research to reach their full promise.
Acute Lymphoblastic Leukemia (ALL): Comparing Adult vs. Childhood Outcomes
Acute Lymphoblastic Leukemia (ALL) shows a big difference in outcomes between adults and children. Children usually have a better chance of recovery. This is due to several reasons, like the disease’s nature, the patient’s health, and how well they respond to treatment.
ALL is a blood cancer where too many immature white blood cells, called lymphoblasts, are made. It’s the most common cancer in kids but can also affect adults, with different results.
Poorer Outcomes in Adults
Adults with ALL face tougher challenges than kids. Several reasons explain this:
- Biological Differences: The genes of ALL cells are different in adults and kids. Adults often have riskier genetic traits.
- Comorbidities: Adults usually have other health problems. This makes them less able to handle strong chemotherapy.
- Treatment Response: Adults tend to react slower to treatment and are more likely to have the cancer come back.
Treatment Approaches and Challenges
Treatment for ALL includes chemotherapy, targeted therapy, and sometimes bone marrow transplants. Kids usually follow a standard treatment plan. But adults need more personalized care because of their health and the type of ALL they have.
| Treatment Aspect | Children | Adults |
| Chemotherapy Intensity | High intensity, well-tolerated | Adjusted based on health, often less intensive |
| Targeted Therapy | Used in combination with chemotherapy | Used, with a focus on specific genetic markers |
| Bone Marrow Transplantation | Rarely needed for initial treatment | Often considered for high-risk or relapsed cases |
It’s important to understand these differences. This helps in creating effective treatment plans for both adults and children with ALL.
Chronic Lymphocytic Leukemia (CLL): When It Becomes Aggressive
CLL turning into a more aggressive cancer is a big worry for both patients and doctors. CLL is a blood cancer that makes too many immature white blood cells, called lymphocytes. Even though CLL is usually a long-term condition, it can get worse in some cases, making it very hard to handle.
Richter’s Transformation: A Deadly Complication
Richter’s transformation is a scary complication of CLL. It turns CLL into a more aggressive lymphoma, like diffuse large B-cell lymphoma (DLBCL). This change is linked to a bad outlook and makes treatment very tough. Richter’s transformation happens in about 2-10% of CLL patients, but the exact number can change.
To diagnose Richter’s transformation, doctors use a mix of clinical checks, imaging, and biopsies. The exact reasons for this transformation are not clear. But, some genetic traits and specific mutations might play a part.
Addressing Treatment Resistance
Another big problem in treating advanced CLL is resistance to treatment. As CLL gets worse, it often stops responding to usual treatments. This makes it hard to keep the cancer in check. The cancer cells’ ability to resist treatment often comes from genetic changes.
- Genetic Mutations: Some mutations, like those in the TP53 gene, mean a worse outlook and less treatment success.
- Treatment Strategies: New treatments, like targeted and immunotherapies, are being tried to beat CLL resistance.
In summary, CLL can turn aggressive through Richter’s transformation and become resistant to treatment. This creates big challenges for both patients and doctors. It’s key to understand these issues to find better ways to manage CLL.
Aggressive Non-Hodgkin Lymphomas: Diffuse Large B-Cell and Others
Aggressive non-Hodgkin lymphomas are a big challenge in cancer treatment. They grow fast and don’t respond well to usual treatments. We’ll look at these lymphomas, focusing on diffuse large B-cell lymphoma and how genetic changes like double-hit and triple-hit lymphomas affect them.
Double-Hit and Triple-Hit Lymphomas
Double-hit and triple-hit lymphomas are types of non-Hodgkin lymphoma with specific genetic problems. They have changes in the MYC gene and sometimes in BCL2 and/or BCL6 genes. This makes the disease more aggressive and harder to treat.
A study in the Journal of Clinical Oncology found that patients with double-hit lymphoma have a much lower survival rate. This shows we need to find and treat these lymphomas early and with specific plans.
“The presence of double-hit or triple-hit genetic features in lymphoma patients necessitates a more aggressive and targeted therapeutic strategy to improve outcomes.”
Treatment Challenges in Aggressive Lymphomas
Treating aggressive non-Hodgkin lymphomas, like diffuse large B-cell lymphoma, is tough. Because these diseases are different, one treatment doesn’t work for everyone. We must think about the patient’s age, health, and the lymphoma’s genetic makeup when planning treatment.
| Treatment Approach | Characteristics | Challenges |
| Chemotherapy | Standard first-line treatment | Resistance, toxicity |
| Targeted Therapy | Specific to lymphoma cells | Cost, accessibility |
| CAR T-Cell Therapy | Innovative, personalized | Cytokine release syndrome, neurotoxicity |
We’re always trying to get better at treating aggressive non-Hodgkin lymphomas. By understanding the genetics and clinical features of these diseases, we can create more effective and personalized treatments.
Multiple Myeloma: Treatment Resistance and Relapse
Multiple myeloma is a tough blood cancer that often stops working after treatment. This makes it hard to manage the disease, leading to relapse in many cases.
Why Multiple Myeloma Eventually Becomes Treatment-Resistant
Multiple myeloma becomes resistant because of changes in the cancer cells. Genetic mutations and epigenetic modifications change how myeloma cells work. This makes them less likely to respond to treatment.
- Genetic mutations that activate survival pathways
- Epigenetic changes that silence tumor suppressor genes
- Interactions between myeloma cells and the bone marrow microenvironment
These changes cause drug resistance, making treatments less effective. It’s important to understand these changes to find new ways to treat the disease.
High-Risk Cytogenetic Features
Some genetic features make relapse more likely in multiple myeloma patients. These include:
- Deletion of chromosome 17p
- Translocations involving the immunoglobulin heavy chain locus
- Gain or amplification of specific chromosomal regions
Knowing about these high-risk features helps doctors tailor treatments. This can improve patient outcomes.
Managing multiple myeloma needs a detailed approach. We must consider genetic, molecular, and environmental factors. By understanding resistance and identifying high-risk features, we aim to create better treatments for this disease.
Myelofibrosis and Other Myeloproliferative Neoplasms
Myelofibrosis is a type of myeloproliferative neoplasm. It can turn into more aggressive leukemia. Myeloproliferative neoplasms (MPNs) affect blood cell production in the bone marrow. We will look into these disorders and their impact on patient care.
Transformation to Acute Leukemia
Myelofibrosis can turn into acute myeloid leukemia (AML). AML is a more aggressive and often treatment-resistant blood cancer. This change is linked to a poor prognosis and limited treatment choices.
It’s important to watch how the disease progresses. Monitoring disease progression and finding risk factors early can help reduce this risk.
Limited Treatment Options for Advanced Disease
For those with advanced myelofibrosis or AML, treatment choices are few. Current treatments aim to manage symptoms and improve quality of life. But, we need more effective treatments to tackle the disease itself.
Understanding how myelofibrosis turns into acute leukemia is key. It helps in creating better treatment plans.
The table below highlights key points about myelofibrosis and its transformation to acute leukemia:
| Disease State | Characteristics | Treatment Options |
| Myelofibrosis | Scarring of the bone marrow, anemia, splenomegaly | JAK inhibitors, symptom management |
| Transformation to AML | Aggressive leukemia, poor prognosis | Chemotherapy, targeted therapies, clinical trials |
We aim to improve our understanding and treatment of myelofibrosis and related MPNs. By diving into new research and treatments, we can enhance patient outcomes and quality of life.
Blood Cancer Survival Rates: Comparing the Most Lethal Types
Looking at survival rates for the deadliest blood cancers gives us important insights. Blood cancers like leukemia, lymphoma, and multiple myeloma have different survival chances. These chances depend on the type, stage, and other factors.
Five-Year Survival Statistics
Five-year survival rates are key to understanding blood cancer patient outcomes. Recent data shows that survival rates for all blood cancers have gone up. This is thanks to better treatments. But, there are big differences between the types.
For example, Acute Myeloid Leukemia (AML) has a five-year survival rate of about 40%. On the other hand, Acute Lymphoblastic Leukemia (ALL) has a rate of 68% in adults and 90% in kids. Some lymphomas and multiple myelomas have survival rates from 50% to over 90%. This depends on the specific type and how early it’s caught.
Factors That Influence Survival
Many things can affect how long blood cancer patients live. These include:
- Age: Older patients often face tougher challenges because they can’t handle strong treatments as well. They also might have other health issues.
- Overall Health: Patients who are healthier and have fewer other health problems tend to live longer.
- Response to Treatment: How well the first treatment works and if the cancer goes into remission greatly affects long-term survival.
- Genetic Factors: Some genetic issues can change how well a patient responds to treatment and their overall outlook.
Knowing these factors and how they work together is key. It helps doctors create better treatment plans. This can lead to better survival rates for blood cancer patients.
Treatment Challenges in Aggressive Blood Cancers
Dealing with aggressive blood cancers is tough. We face many hurdles, like drug resistance, barriers that protect cancer cells, and the harm caused by treatments. These obstacles make it hard to treat these cancers effectively.
Drug Resistance Mechanisms
Drug resistance is a big problem in treating aggressive blood cancers. Cancer cells can resist drugs in many ways, like genetic changes or by pumping drugs out. Drug resistance makes treatments less effective, leading to lower success rates and worse outcomes.
- Genetic mutations that alter drug targets or activate alternative signaling pathways.
- Overexpression of drug efflux pumps, such as P-glycoprotein, which reduces intracellular drug concentrations.
- Epigenetic changes that confer resistance to specific therapies.
The Blood-Brain Barrier Challenge
The blood-brain barrier (BBB) is a big challenge in treating blood cancers, like those in the brain. The BBB blocks many drugs from reaching the brain. This barrier makes treating brain cancers hard, and we need new ways to get drugs past it.
“The blood-brain barrier remains a significant obstacle in the treatment of CNS leukemia and lymphoma, requiring innovative approaches to deliver effective therapies.”
Toxicity Limitations
Treatment toxicity is another big challenge. Strong treatments needed to fight cancer can harm patients a lot. Toxicity limitations mean we have to find a balance. We want treatments to work well but also be safe for patients.
- Careful dose adjustment and monitoring to minimize toxicity.
- Use of supportive care measures to manage treatment-related side effects.
- Development of novel therapies with improved safety profiles.
Rare Blood Cancers with Poor Prognosis
Rare blood cancers are tough for doctors to treat because they grow fast and have few treatment options. These cancers have unique features that make them hard to diagnose and treat. We’ll look at some of the rarest and toughest blood cancers, like T-cell lymphomas, blastic plasmacytoid dendritic cell neoplasm, advanced systemic mastocytosis, and acute erythroid leukemia.
T-Cell Lymphomas
T-cell lymphomas are a group of non-Hodgkin lymphomas that start from T cells. They are not common and can be aggressive, often diagnosed at a late stage. Treatment outcomes vary a lot depending on the subtype, with some being more treatable than others.
The complexity of T-cell lymphomas comes from their varied symptoms and biology. When the disease is advanced, it needs strong treatments like chemotherapy and targeted therapies.
Blastic Plasmacytoid Dendritic Cell Neoplasm
Blastic plasmacytoid dendritic cell neoplasm (BPDCN) is a rare and aggressive cancer from plasmacytoid dendritic cells. It starts with skin lesions and then spreads. The outlook is generally bleak, with a high chance of relapse even after treatment.
Advanced Systemic Mastocytosis
Systemic mastocytosis is when mast cells grow in many organs. Advanced systemic mastocytosis can turn into more aggressive forms, like mast cell leukemia, which has a very poor prognosis. Treatment choices are few, and managing symptoms and slowing disease progression often need a team effort.
Acute Erythroid Leukemia
Acute erythroid leukemia is a rare form of acute myeloid leukemia (AML) with fast-growing erythroid precursors. It has a poor prognosis because of its aggressive nature and resistance to common AML treatments. New treatment approaches are being looked into to better outcomes in this tough disease.
Age and Comorbidities: When Standard Treatments Aren’t an Option
Age and other health issues are key in deciding if standard treatments work for blood cancer patients. As we get older, our bodies change, affecting how we react to treatments. Also, having other health problems can make treatment plans harder.
Treatment Challenges in Elderly Patients
Elderly patients face special challenges when fighting blood cancer. As we age, our strength and health decline. This, along with other health issues, makes treatment tricky.
One big worry is how well older patients can handle strong treatments. They might be more likely to get side effects from treatments. This can hurt their quality of life and how long they live. We need to think carefully about the benefits and risks of treatment, considering the patient’s health and what they want.
Impact of Other Health Conditions
Having other health problems can change how well blood cancer treatment works. Conditions like diabetes, heart disease, or COPD can raise the risk of side effects. For example, heart problems can make some chemotherapy drugs more dangerous.
Also, other health issues can make it hard to do intensive treatments. For example, someone with kidney disease might need special treatment plans. We must look at how blood cancer, other health problems, and treatments all work together to find the best plan for each patient.
Awell-known hematologist says, “Dealing with comorbidities means we need a careful approach to blood cancer treatment. We must balance fighting the cancer with managing other health issues.” This shows why a team of experts from different fields is important. They help manage the patient’s overall health better.
Breakthrough Treatments Changing the Outlook for Difficult Blood Cancers
The field of blood cancer treatment is seeing big changes. New therapies are making a big difference in how we treat tough blood cancers. This is all thanks to recent advances in medical research.
CAR T-Cell Therapy
CAR T-cell therapy is a new way to fight certain blood cancers. It works by taking T cells from a patient, changing them to find cancer cells, and then putting them back in. It’s really promising for patients with hard-to-treat large B-cell lymphoma.
Studies have shown it works well for those who have tried other treatments and failed.
Targeted Therapies
Targeted therapies aim to hit cancer cells directly, without harming healthy cells. They work great for some blood cancers like CLL and AML.
Examples include tyrosine kinase inhibitors and monoclonal antibodies. These treatments have greatly improved patient outcomes.
Immunotherapies
Immunotherapies boost the body’s fight against cancer. This includes checkpoint inhibitors, which are showing promise in treating blood cancers.
These therapies use the immune system to fight cancer, which could lead to better, longer-lasting treatments.
Promising Clinical Trials
New clinical trials are bringing us closer to better treatments for tough blood cancers. These trials are key to learning more and finding new ways to treat these diseases.
Some of the most exciting areas include combining different therapies and new types of immunotherapies.
| Therapy Type | Description | Examples |
| CAR T-Cell Therapy | Genetically modified T cells to target cancer | Tisagenlecleucel, Axicabtagene ciloleucel |
| Targeted Therapies | Drugs targeting specific cancer cell characteristics | Ibrutinib, Venetoclax |
| Immunotherapies | Therapies that boost the immune system’s fight against cancer | Nivolumab, Pembrolizumab |
These new treatments are changing the game for blood cancer patients. They offer hope and better chances of recovery for those with tough blood cancers.
Comparing Blood Cancers to Other Deadly Malignancies
Blood cancers are among the deadliest types of cancer. It’s important to know how they compare to other cancers. This knowledge helps us understand the severity and mortality rates of blood cancers.
Where Blood Cancers Rank Among All Cancer Types
Statistics show that blood cancers, like leukemia and lymphoma, are a big part of cancer cases and deaths. They are among the top 10 most common cancers worldwide.
To see how severe blood cancers are, let’s look at their ranking. The table below compares the incidence and mortality rates of various cancers. It shows where blood cancers stand.
| Cancer Type | Estimated New Cases (2022) | Estimated Deaths (2022) |
| Breast Cancer | 2,261,419 | 685,636 |
| Lung Cancer | 2,206,771 | 1,796,144 |
| Colorectal Cancer | 1,931,590 | 935,173 |
| Leukemia | 437,033 | 309,006 |
| Non-Hodgkin Lymphoma | 544,352 | 259,793 |
| Multiple Myeloma | 176,404 | 117,161 |
Unique Challenges of Hematologic Malignancies
Hematologic malignancies have unique challenges. They affect the blood and bone marrow, leading to issues like anemia and bleeding. Their systemic nature means treatments often target the whole body.
Another challenge is the variety within blood cancer subtypes. For example, leukemia can be acute or chronic, affecting treatment and prognosis differently. Lymphomas also vary in aggressiveness and treatment response.
Understanding these complexities is key to better treatments and patient outcomes. Ongoing research is leading to new therapies, giving hope to those with blood cancers.
Conclusion: The Future of Treating Aggressive Blood Cancers
Aggressive blood cancers are tough to treat because of their complex nature and fast growth. But, the outlook for treating blood cancers is getting better.
New research and treatments are leading to better results for patients. CAR T-cell therapy, targeted therapies, and immunotherapies are giving patients new hope.
We’re seeing a move towards treatments that are more tailored and effective. This is helping patients live longer and better lives. As we learn more about aggressive blood cancers, we’ll see even more advanced treatments.
The future for treating aggressive blood cancers is bright. We have more options and a better understanding of these diseases. To keep improving, we need to keep researching and investing in new treatments.
FAQ
What is the most deadly form of blood cancer?
Acute Myeloid Leukemia (AML) is very deadly. It grows fast and is hard to treat.
What are the different types of blood cancers?
Blood cancers include leukemia, lymphoma, multiple myeloma, and myelodysplastic syndromes (MDS).
How does blood cancer differ from solid tumors?
Blood cancer starts in blood cells or bone marrow. Solid tumors start in organs or tissues.
What is the survival rate for blood cancer?
Survival rates depend on the cancer type, stage, and the patient’s health.
What is Acute Lymphoblastic Leukemia (ALL)?
ALL affects lymphoid cells and is common in kids but can also hit adults.
Why is AML considered difficult to treat?
AML is hard to treat because it grows fast, has genetic issues, and doesn’t respond well to chemo.
What is Chronic Lymphocytic Leukemia (CLL)?
CLL is a slow-growing leukemia that affects lymphoid cells. It can turn aggressive.
What are the treatment challenges for aggressive non-Hodgkin lymphomas?
Aggressive non-Hodgkin lymphomas need strong chemo and targeted therapies. But, they can resist treatment.
How does multiple myeloma become treatment-resistant?
Multiple myeloma can resist treatment due to genetic changes and the growth of resistant cancer cells.
What is myelofibrosis, and how does it relate to blood cancer?
Myelofibrosis is a rare disorder that can lead to acute leukemia. It causes scarring in the bone marrow.
What are the latest breakthrough treatments for blood cancers?
New CAR T-cell therapy, targeted therapies, and immunotherapies have improved treatment for some blood cancers.
How do age and comorbidities impact treatment options for blood cancer patients?
Older patients and those with health issues may not get standard treatments. They need other options.
What are the unique challenges of hematologic malignancies?
Blood cancers face challenges like the blood-brain barrier, which limits treatment.
Can blood cancer be cured?
Some blood cancers can be cured. Others need ongoing care and monitoring.
What is the prognosis for rare blood cancers?
Rare blood cancers, like T-cell lymphomas, often have a poor prognosis. This is because of limited treatment options.
References
Shimony, S. (2015). Acute Myeloid Leukemia: 2025 update on diagnosis, risk assessment, genetic features, and treatment. Current Hematologic Malignancy Reports, 10(3), 216-230. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC11966364/




































