Every year, millions of people worldwide face a life-threatening condition. It happens when the body’s response to infection damages its own tissues and organs. Sepsis is a serious medical emergency. It can cause shock, organ failure, and death if not treated quickly.
Sepsis is a challenging condition, but knowing its symptoms and causes is key. When the body’s response to an infection gets out of control, it can lead to a deadly condition.
Key Takeaways
- Sepsis is a life-threatening condition that requires immediate medical attention.
- Understanding the symptoms of sepsis is critical for timely treatment.
- Septic shock is a severe complication of sepsis that can lead to multiple organ failure.
- Prompt medical intervention is essential to prevent long-term damage or death.
- Understanding the definition of sepsis is crucial for early identification of the condition.
Understanding Blood Infections and Their Severity
Blood infections can range from mild to very serious, like sepsis. It’s important to know about these infections to understand the risks and what can happen.
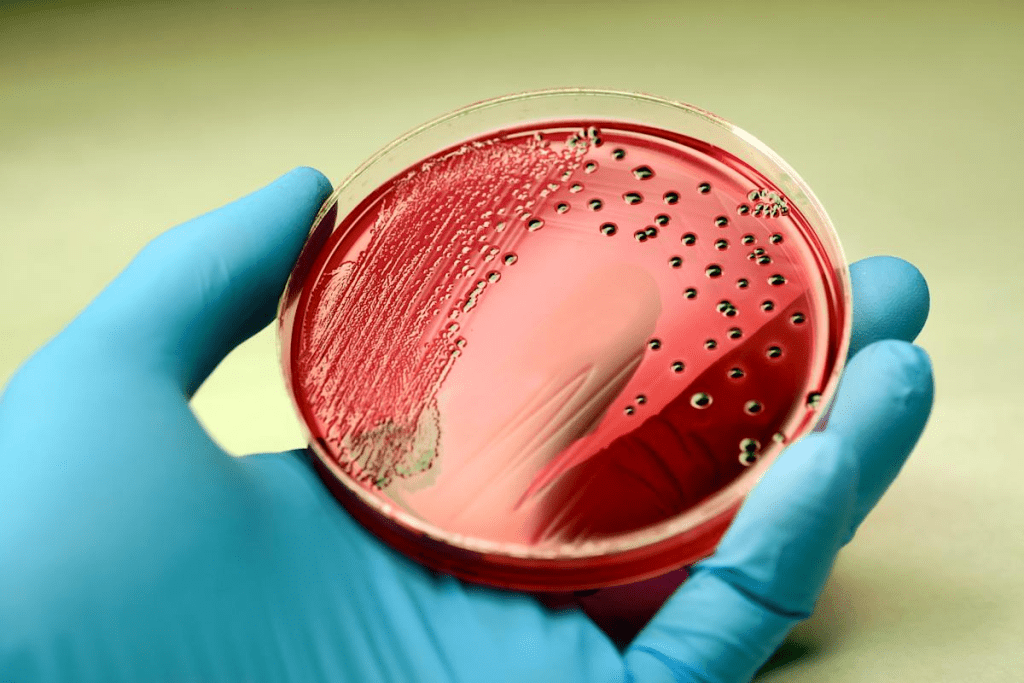
Common Types of Blood Infections
There are different kinds of blood infections. They are caused by various things:
- Bacterial infections, which happen when bacteria get into the blood.
- Viral infections, though rarer, can also be very serious.
- Fungal infections, mainly in people with weakened immune systems.
Why Blood Infections Are Dangerous
Blood infections are dangerous because they can cause inflammation and harm organs. Sepsis is a severe condition. It happens when the body overreacts to an infection, leading to inflammation everywhere. This can cause organs to fail and even death if not treated right away.
Sepsis: The Most Serious Blood Infection

Sepsis is a life-threatening condition. It happens when the body’s response to an infection damages its own tissues and organs. It’s a complex and potentially fatal medical emergency that needs immediate attention. We will explore the definition of sepsis, distinguish it from septicemia, and compare it with other systemic infections to understand its severity and implications fully.
Understanding the definition of sepsis is crucial for early identification of the condition.
Understanding the definition of sepsis is crucial for early identification of the condition.
Difference Between Sepsis and Septicemia
Understanding the definition of sepsis is crucial for early identification of the condition.
Sepsis vs. Other Systemic Infections
Sepsis is distinct from other systemic infections due to its severity and the body’s dysregulated response. While systemic infections involve the infection spreading through the bloodstream, sepsis is characterized by its ability to cause organ dysfunction. Other systemic infections may not necessarily lead to the same level of organ damage or the life-threatening complications associated with sepsis.
| Condition | Definition | Severity |
| Sepsis | Life-threatening organ dysfunction due to a dysregulated host response to infection. | High |
| Septicemia | Understanding the definition of sepsis is crucial for early identification of the condition. | Variable |
| Systemic Infection | Infection spread through the bloodstream. | Variable, potentially high |
By understanding sepsis, its distinction from septicemia, and its comparison to other systemic infections, we can better appreciate the severity of this condition. We also see the importance of prompt medical intervention.
Understanding the definition of sepsis is crucial for early identification of the condition.
Sepsis is a complex condition where the body’s immune system overreacts to an infection. This can cause damage to tissues, failure of organs, and even death if not treated quickly.
Understanding the definition of sepsis is crucial for early identification of the condition.
When an infection happens, the body fights it by releasing chemicals into the blood. In sepsis, this fight goes too far, causing widespread inflammation. This inflammatory response can harm many organs, making them not work right.
Understanding the definition of sepsis is crucial for early identification of the condition.
The fight against infection in sepsis is complex. It starts with a pro-inflammatory response to fight the infection. But, in sepsis, this response gets too strong. It releases too many cytokines, which can harm organ function.
Organ System Impacts
Sepsis can hit any organ system hard, but some are hit more often. Here’s a table showing which organs are most affected:
| Organ System | Potential Impact |
| Cardiovascular | Hypotension, decreased cardiac output |
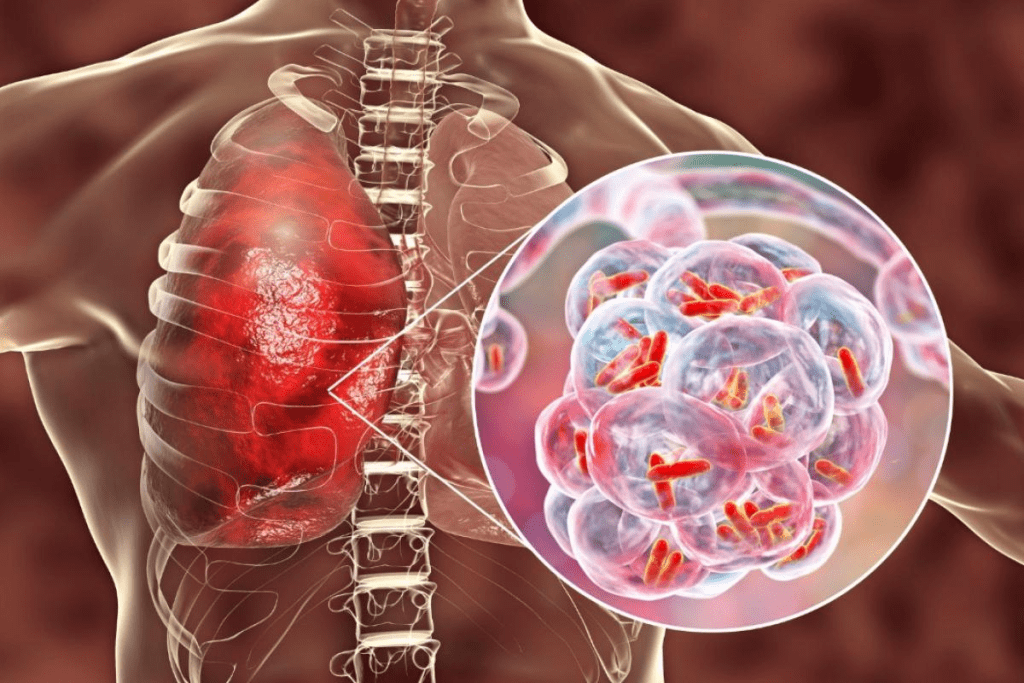
| Respiratory | Acute Respiratory Distress Syndrome (ARDS) |
| Renal | Acute Kidney Injury (AKI) |
| Hepatic | Impaired liver function, coagulopathy |
Knowing how sepsis works is key to treating it well. By understanding how it affects the body and organs, doctors can give better care. This can help patients get better faster.
Common Causes of Sepsis
Knowing what causes sepsis is key to preventing and treating it. Sepsis is a serious condition where the body’s fight against infection harms its own tissues and organs. We’ll look at the main causes, including infections and their sources.
Bacterial Infections
Bacterial infections are the top reason for sepsis. Gram-positive and Gram-negative bacteria can both cause sepsis. Pneumonia, urinary tract infections, and abdominal infections are common culprits.
Viral and Fungal Triggers
Viral and fungal infections can also lead to sepsis, though less often. Viral infections like influenza and COVID-19 can be severe. Fungal infections are more common in people with weak immune systems.
Most Common Sources of Infection
The usual places where infections start that can lead to sepsis are:
- Urinary tract infections
- Pneumonia
- Abdominal infections
- Skin infections
| Source of Infection | Description | Risk Factors |
| Urinary Tract Infections | Infections in the bladder or kidneys | Older age, catheter use |
| Pneumonia | Understanding the definition of sepsis is crucial for early identification of the condition. | Chronic lung disease, smoking |
| Abdominal Infections | Infections within the abdominal cavity | Recent surgery, perforated ulcer |
By knowing these common causes and sources, we can spot who’s at risk sooner. This helps us act fast to prevent sepsis.
Risk Factors for Developing Sepsis
Knowing the risk factors for sepsis is key to catching it early and treating it well. Sepsis can hit anyone, but some are more at risk because of different factors.
Age-Related Risk Factors
Age is a big factor in sepsis risk. Older adults and young children are more at risk because their immune systems are weaker.
- Adults 65 and older face a higher risk because their immune function drops and they often have chronic health issues.
- Children under 1, like those born early or with low birth weight, are also at a higher risk.
Medical Conditions That Increase Risk
Having certain medical conditions can make you more likely to get sepsis. These conditions make it harder for the body to fight off infections.
- Chronic illnesses like diabetes, cancer, and kidney disease can weaken the immune system.
- Being on immunosuppressive drugs, like those with autoimmune diseases or organ transplant recipients, also raises the risk.
Environmental and Lifestyle Factors
Environmental and lifestyle factors can also up the risk of sepsis. Poor hygiene, unsanitary living conditions, and lifestyle choices that weaken the immune system can make you more susceptible.
- Being exposed to dirty conditions or contaminated water can lead to infections that might turn into sepsis.
- Lifestyle choices like smoking, drinking too much alcohol, and eating a bad diet can also weaken the immune system.
By knowing these risk factors, we can take steps to lower our chances of getting sepsis. Being aware and taking preventive actions are important for managing this serious condition.
Recognizing Sepsis: Signs and Symptoms
Understanding the definition of sepsis is crucial for early identification of the condition.
Early Warning Signs
The first signs of sepsis can be vague but often include fever, tachycardia (rapid heart rate), and tachypnea (rapid breathing rate). You might also feel generally unwell. Catching these signs early is key to better treatment outcomes.
Other early signs include:
- Chills or feeling very cold
- Confusion or disorientation
- Shortness of breath
- High or low body temperature
Advanced Symptoms
As sepsis worsens, symptoms get more severe, including organ dysfunction. Advanced symptoms may include:
- Decreased urine output
- Severe difficulty breathing
- Abnormal heart rhythms
- Septic shock, a dangerous drop in blood pressure
In severe cases, sepsis can turn into septic shock. This is a life-threatening condition that needs immediate medical care.
The Sepsis Rash and Other Visual Indicators
A sepsis rash or other visual signs can appear. The rash might be due to the infection or the body’s response. Other visual signs include:
- Pale or discolored skin
- Mottled or blotchy skin
Certain groups, like the elderly, young children, and those with weak immune systems, may show different symptoms. For example:
- Elderly individuals may show confusion or altered mental status as an early sign.
- Children may display non-specific signs like irritability or lethargy.
Knowing these variations is key for early detection and treatment in these groups.
The Progression of Sepsis: From Infection to Septic Shock
It’s important to know how sepsis turns into septic shock to catch it early. Sepsis is a serious condition where the body overreacts to an infection. This leads to widespread inflammation. We’ll look at the stages of sepsis, how septic shock develops, and its signs.
Understanding the definition of sepsis is crucial for early identification of the condition.
Sepsis goes through different stages, each with its own traits. The stages are:
- Sepsis: The first stage where the body’s reaction to an infection gets out of control.
- Severe Sepsis: A more serious stage where organs start to fail.
- Septic Shock: The most severe stage, with deep problems in blood flow, cells, and metabolism.
Understanding Septic Shock
Septic shock is a part of sepsis with very serious problems. It has a higher risk of death than sepsis alone. Patients with septic shock need quick and effective treatment to survive.
Clinical Features of Septic Shock
The signs of septic shock include:
| Clinical Feature | Description |
| Hypotension | Persistent low blood pressure despite enough fluids. |
| Organ Dysfunction | Failure of organs like the kidneys, liver, or lungs. |
| Hyperlactatemia | High lactate levels showing tissue lack of oxygen. |
Spotting these signs is key to diagnosing septic shock and starting the right treatment.
When to Seek Medical Help for Suspected Sepsis
Knowing when to seek help for suspected sepsis can save lives. Sepsis is a serious condition where the body attacks itself due to infection. It’s important to act fast when sepsis is suspected.
Red Flag Symptoms
Spotting red flag symptoms is key to getting medical help quickly. These include:
- High or very low body temperature
- Rapid heart rate
- Rapid breathing rate
- Confusion or disorientation
- Severe pain or discomfort
If you or someone you know shows these signs, act fast. Sepsis is a medical emergency. Waiting too long can cause serious harm, like organ failure and death.
Emergency Response
When sepsis is suspected, quick action is needed. Here’s what to do:
- Call emergency services or get to the hospital right away.
- Share as much info as you can about symptoms and medical history.
- If the situation gets worse, don’t wait to act.
| Symptom | Action |
| High fever, chills | Seek medical help immediately |
| Rapid heart rate, rapid breathing | Call emergency services |
| Confusion, disorientation | Seek immediate medical attention |
Communicating Effectively with Healthcare Providers
Talking clearly with healthcare providers is key when dealing with suspected sepsis. Be ready to share details about symptoms, medical history, and any recent infections or injuries. This helps doctors make the best decisions for your care.
By knowing when to seek help and how to talk to doctors, you can help manage sepsis. Remember, time is of the essence in treating sepsis.
Diagnosing Sepsis: Medical Approaches
Healthcare professionals use many methods to diagnose sepsis. These include clinical checks and advanced tests. Accurate diagnosis is key for quick and effective treatment.
Diagnostic Criteria for Sepsis
The Sequential Organ Failure Assessment (SOFA) score is the main tool for diagnosing sepsis. It measures organ dysfunction. A score of 2 or more means serious organ issues and a higher risk of death.
We use the SOFA score with clinical checks to spot at-risk patients. The score looks at PaO2/FiO2 ratio, platelet count, bilirubin levels, blood pressure, Glasgow Coma Scale, and creatinine levels or urine output. Each factor is scored from 0 to 4, showing how severe the dysfunction is.
| Parameter | SOFA Score = 0 | SOFA Score = 1 | SOFA Score = 2 | SOFA Score = 3 | SOFA Score = 4 |
| PaO2/FiO2 (mmHg) | >400 | ||||
| Platelet Count (x10^3/ µL) | >150 | ||||
| Bilirubin (mg/dL) | 1.2-1.9 | 2.0-5.9 | 6.0-11.9 | >12.0 |
Laboratory Tests
Laboratory tests are vital for diagnosing sepsis. Tests like complete blood count (CBC), blood cultures, lactate levels, and arterial blood gas (ABG) are used. They show if there’s an infection, how severe the inflammation is, and how much organ damage there is.
High lactate levels mean tissues are not getting enough oxygen, a key sign of sepsis. Blood cultures help find the infection-causing bacteria, guiding the right antibiotics.
Imaging and Other Diagnostic Tools
Imaging studies like X-rays, CT scans, and ultrasounds help find where the infection is. They’re used to spot issues like pneumonia or abscesses that might be causing sepsis.
Other tools, such as echocardiography and specialized tests, are used based on the situation. They help check the heart and other organs.
Treatment Strategies for Sepsis
Sepsis treatment is a mix of actions to fight the infection and help the body heal. It needs a full plan that includes many medical steps.
Emergency Interventions
When sepsis is thought of, emergency interventions are key. First, check the patient’s airway, breathing, and circulation (ABCs) to keep them stable. Giving oxygen therapy is often the first step to boost blood oxygen levels.
Antibiotic Therapy
Antibiotic therapy is vital in treating sepsis, mainly when it’s caused by bacteria. Broad-spectrum antibiotics are given quickly, even before knowing the exact cause. The aim is to start treatment fast to lower the risk of serious problems.
- Administer broad-spectrum antibiotics
- Adjust antibiotics based on culture results
- Monitor for antibiotic resistance
Supportive Care Measures
Besides antibiotics, supportive care measures are also key in managing sepsis. These include giving fluids to keep blood pressure up, feeding the patient, and watching for organ problems. Supportive care helps lessen sepsis’s impact and better patient results.
New and Emerging Treatments
There’s always new research on new and emerging treatments for sepsis. This includes immunomodulatory therapies, new antibiotics, and advanced life-support tools. These new methods aim to boost survival chances and lessen sepsis’s long-term effects.
Complications and Long-term Effects of Sepsis
Complications and long-term effects of sepsis are big worries for patients and doctors. Sepsis is a serious condition that can cause lasting health problems even after treatment.
Organ Damage and Failure
One major problem with sepsis is organ damage and failure. When sepsis turns into septic shock, organs like the kidneys, liver, lungs, and heart can get damaged. Organ failure might need intensive care and sometimes even a transplant.
The damage to organs can vary. It depends on how severe the sepsis is and how well the treatment works. Some people might fully recover, while others could face lasting organ problems.
Post-Sepsis Syndrome
People who survive sepsis often face post-sepsis syndrome. This condition brings physical, cognitive, and emotional challenges. Symptoms include fatigue, muscle weakness, trouble concentrating, and feelings of anxiety or depression.
Post-sepsis syndrome can make daily life hard. It’s important for doctors to offer support and help patients deal with these issues.
Psychological Impact on Survivors
The mental effects of sepsis on survivors are significant. The trauma of nearly dying can cause anxiety, depression, and PTSD. Mental health support is key for sepsis survivors to cope with these issues.
Rehabilitation Needs
Rehabilitation is essential for sepsis survivors to regain strength and independence. A good rehab program includes physical therapy, occupational therapy, and mental support. This helps address the many challenges these patients face.
Understanding sepsis complications and long-term effects helps doctors support patients better. This improves recovery outcomes and enhances quality of life.
Sepsis Survival Rates and Prognosis
Understanding the definition of sepsis is crucial for early identification of the condition.
Factors Affecting Survival
Many things affect how likely someone is to survive sepsis. These include:
- Severity of Sepsis: Those with septic shock face a higher risk of death than those with milder sepsis.
- Promptness and Quality of Care: Getting help early and getting good care can really help.
- Underlying Health Conditions: People with long-term illnesses or weak immune systems are more at risk.
- Age: Older people and young kids are more likely to be at risk because their immune systems might not work as well.
Recovery Timeline
Recovering from sepsis can take a long time and varies a lot. Some people might get better in weeks, while others might take months or even years. How fast someone recovers depends on how bad the sepsis was, any other health issues they have, and how well they were treated.
Supportive care is key in helping people get better. This includes physical therapy, eating right, and talking to a counselor to deal with any lasting effects of sepsis.
End-of-Life Considerations with Severe Sepsis
Sadly, not everyone with sepsis makes it, mainly those with very bad septic shock or other serious health problems. When someone is near the end, it’s important to care for them with kindness and understanding. Doctors, nurses, and other healthcare workers work with patients and their families to make sure care matches what the patient wants.
Talking about how things might end can be hard, but it’s very important. It’s not just about medical stuff, but also about emotional and spiritual support.
Understanding the definition of sepsis is crucial for early identification of the condition.
Understanding the definition of sepsis is crucial for early identification of the condition.
Spreading the word about sepsis is key to better outcomes. By learning and sharing, we can spot sepsis signs early. This leads to quicker medical help and lowers the risk of serious problems.
It’s not just about knowing about sepsis. It’s also about creating a culture of care in healthcare. We need to work together to quickly diagnose and treat sepsis. This ensures those affected get the support they need to heal.
By focusing on sepsis education and awareness, we can greatly help those affected. Let’s keep working to raise awareness and fight sepsis together.
FAQ
What is sepsis?
Sepsis is a serious condition where the body attacks its own tissues and organs. It happens when the body’s response to an infection gets out of control. It’s a medical emergency that needs quick action.
What is the difference between sepsis and septicemia?
Septicemia means bacteria are in the blood. Sepsis is the body’s reaction to that infection. Not everyone with septicemia gets sepsis, but it can happen if not treated.
What are the common causes of sepsis?
Bacterial infections often cause sepsis. Viral or fungal infections can too. Common sources include pneumonia, urinary tract infections, and skin infections.
What are the risk factors for developing sepsis?
Some people are more likely to get sepsis. This includes older adults, young children, and those with weak immune systems or health issues.
What are the signs and symptoms of sepsis?
Signs of sepsis include fever, chills, and a fast heart rate. You might also breathe quickly, feel confused, or have a rash. In severe cases, it can cause low blood pressure and organ failure.
How is sepsis diagnosed?
Doctors use physical checks, lab tests, and imaging to diagnose sepsis. They look for signs of infection and organ problems.
What is the treatment for sepsis?
Treatment for sepsis includes antibiotics and fluids. Patients may also need oxygen, nutrition, and sometimes ICU care.
Can sepsis be cured?
Yes, many people recover from sepsis with the right treatment. But, some may face long-term effects like organ damage or post-sepsis syndrome.
What are the complications of sepsis?
Sepsis can cause organ damage, amputations, and PTSD. In severe cases, it can be fatal.
How can I prevent sepsis?
Preventing sepsis means staying clean, getting vaccinated, and managing health conditions. Seeking medical help for infections quickly is also key.
What is septic shock?
Septic shock is a severe stage of sepsis. It’s marked by very low blood pressure, organ failure, and poor blood flow. It’s a life-threatening condition needing immediate care.
What is the survival rate for sepsis?
Survival rates for sepsis depend on how severe it is, the person’s health, and how quickly and well they’re treated. Early action and treatment help a lot.
References
La DHS. (2025). Sepsis. Global burden. Retrieved from
https://www.who.int/news-room/fact-sheets/detail/sepsis
Highlights that nearly 11 million deaths occur annually due to sepsis, with mortality rates in some regions exceeding 50%. The report emphasizes the importance of early diagnosis and improved management strategies worldwide.

































